Copyright
©The Author(s) 2015.
World J Gastroenterol. Oct 21, 2015; 21(39): 11016-11026
Published online Oct 21, 2015. doi: 10.3748/wjg.v21.i39.11016
Published online Oct 21, 2015. doi: 10.3748/wjg.v21.i39.11016
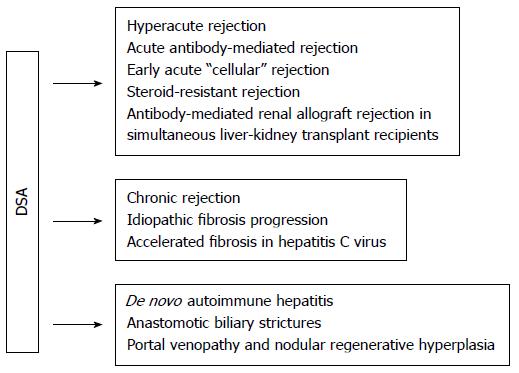
Figure 1 Potential associations of donor-specific human leukocyte antigen antibodies with outcomes in liver transplant or simultaneous liver-kidney transplant recipients.
No associations have been confirmed in large randomized controlled trials. Adapted from O'Leary et al[34]. HLA: Human leukocyte antigen; DSA: Donor-specific anti-HLA antibodies.
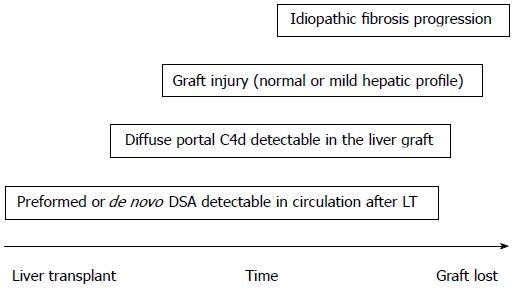
Figure 2 Idiopathic fibrosis progression.
Hypothetical chain of events. DSA: Donor-specific anti-HLA antibodies; LT: Liver transplant.
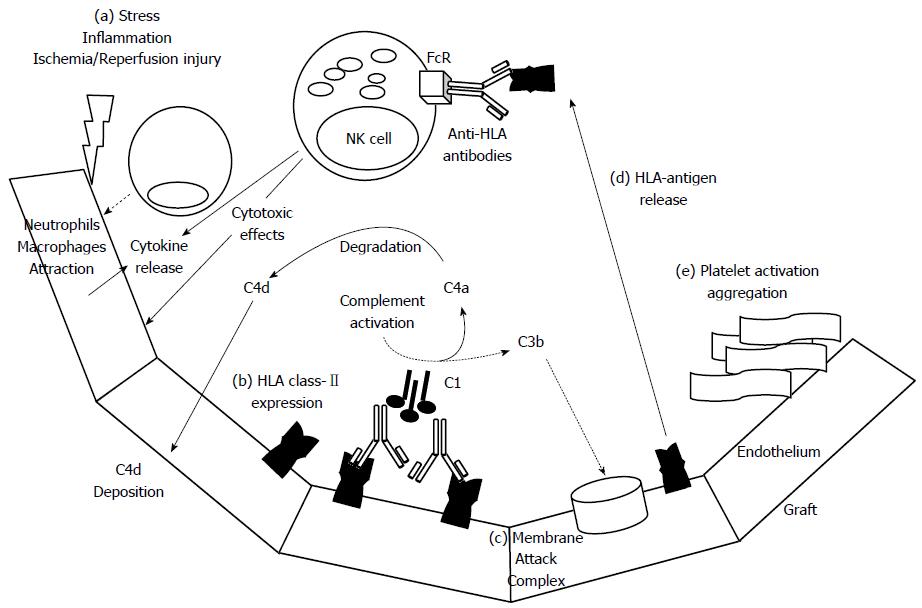
Figure 3 Mechanisms involved in humoral graft damage.
Early post transplantation after ischemia/reperfusion injury (a) the endothelium can release several chemokines and cytokines to gather innate immune cells as neutrophils, macrophages. In this inflammatory setting, the graft endothelium could be activated and expressed human leukocyte antigen (HLA) class-II antigens (b), subsequently, these antigens could be recognized by anti-HLA class-II antibodies. If the antibodies are able to fix complement factors could trigger classical complement pathway that finally induce the membrane attack complex (c) on targeted endothelial cells. During complement activation, C4a component is degraded in C4d and finally deposited on capillaries. After destruction of endothelial cells, the HLA class-II molecules could be released and directly detected by circulating anti-HLA antibodies that once recognized by FC receptors on NK cells could direct cytotoxic actions and cytokine production. Another potential mechanism of humoral graft damage could be driven by platelet activation and thrombi formation (e).
- Citation: Cuadrado A, San Segundo D, López-Hoyos M, Crespo J, Fábrega E. Clinical significance of donor-specific human leukocyte antigen antibodies in liver transplantation. World J Gastroenterol 2015; 21(39): 11016-11026
- URL: https://www.wjgnet.com/1007-9327/full/v21/i39/11016.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i39.11016