Copyright
©The Author(s) 2015.
World J Gastroenterol. May 14, 2015; 21(18): 5622-5629
Published online May 14, 2015. doi: 10.3748/wjg.v21.i18.5622
Published online May 14, 2015. doi: 10.3748/wjg.v21.i18.5622
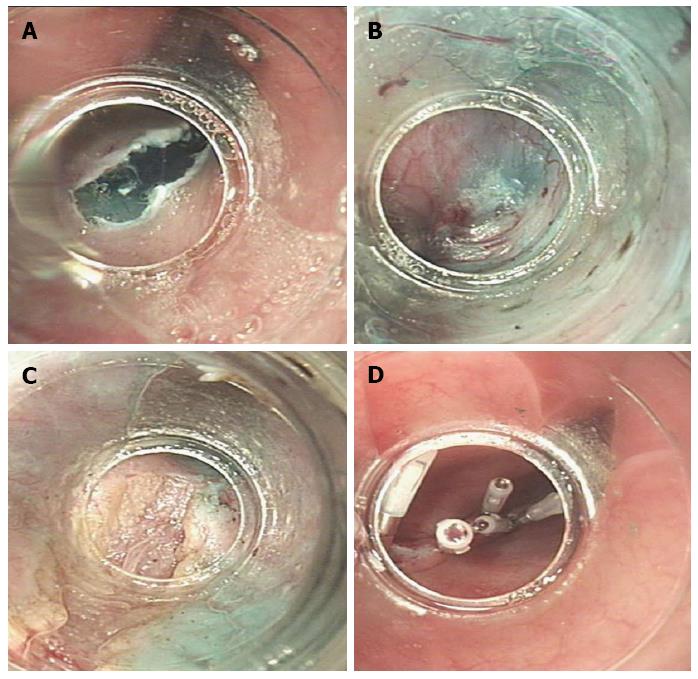
Figure 1 Peroral endoscopic myotomy procedure.
A: A 2 cm oblique incision was made into the mucosal surface; B: A long submucosal tunnel was created by careful electrocoagulation using an insulation-tipped electrosurgical knife; C: Endoscopic myotomy was initiated 2 cm distal to the mucosal entry using a hook knife. The inner circular muscle was dissected while the outer longitudinal muscle layer remained intact; D: After complete myotomy (approximately 10 cm), the mucosal entry site was closed using endoscopic clips.
Figure 2 Eckardt scores.
The Eckardt scores of patients were recorded before peroral endoscopic myotomy and at various times postoperatively; P < 0.01 vs before peroral endoscopic myotomy.
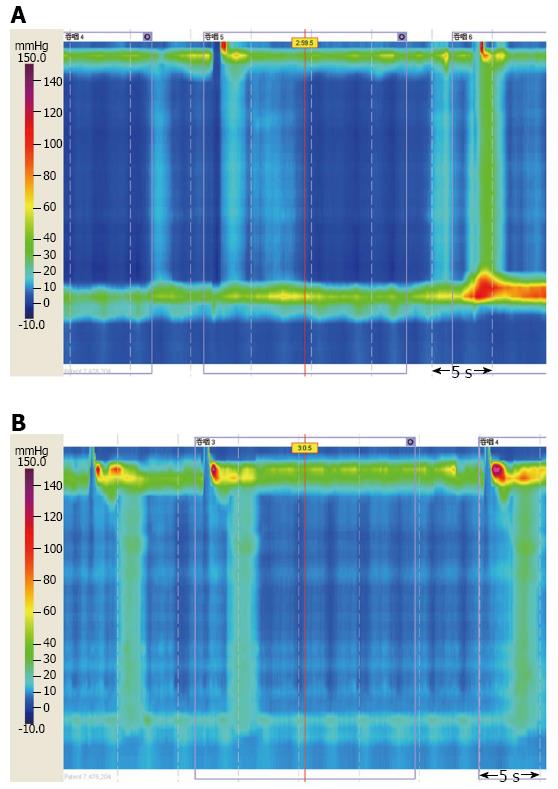
Figure 3 Esophageal high-resolution manometry.
Representative manometric results from a patient with type II achalasia A: Before; and B: One month after peroral endoscopic myotomy. Lower esophageal sphincter pressure was reduced, with relaxation and passage of lower esophageal sphincter seen upon swallowing.
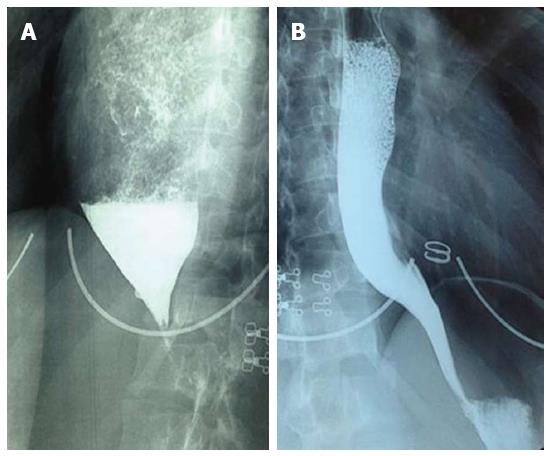
Figure 4 Barium swallow.
A: Dilated esophagus showing a retained column of barium and “bird’s beak”, suggestive of achalasia; B: Esophagogram one month after peroral endoscopic myotomy. Barium passed and was excreted quickly through the lower esophageal sphincter.
- Citation: Lu B, Li M, Hu Y, Xu Y, Zhang S, Cai LJ. Effect of peroral esophageal myotomy for achalasia treatment: A Chinese study. World J Gastroenterol 2015; 21(18): 5622-5629
- URL: https://www.wjgnet.com/1007-9327/full/v21/i18/5622.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i18.5622