Copyright
©The Author(s) 2015.
World J Gastroenterol. Mar 14, 2015; 21(10): 3121-3126
Published online Mar 14, 2015. doi: 10.3748/wjg.v21.i10.3121
Published online Mar 14, 2015. doi: 10.3748/wjg.v21.i10.3121
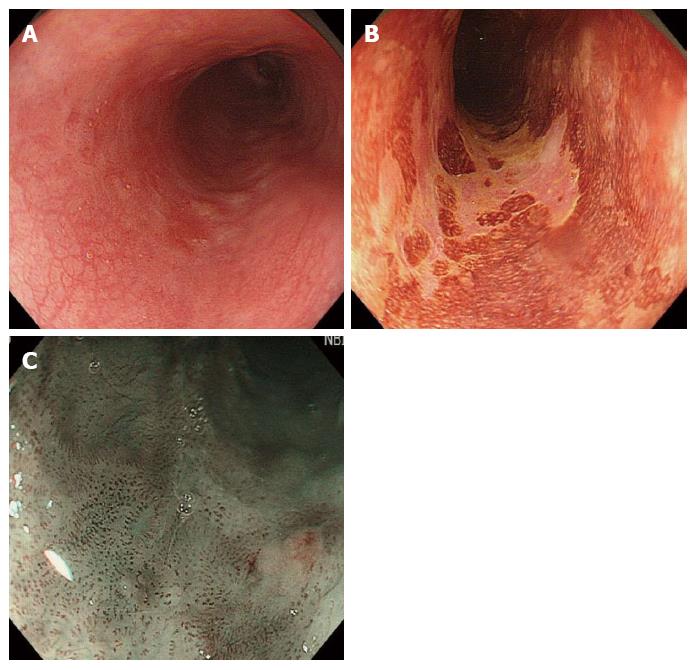
Figure 1 Endoscopic observation of esophageal cancer.
A, B: Lesion had expanded to half of the circumference of the lumen; C: In magnified narrow band imaging (NBI) observation, intraepithelial papillary capillary loop (IPCL) was detected as a small dot pattern.
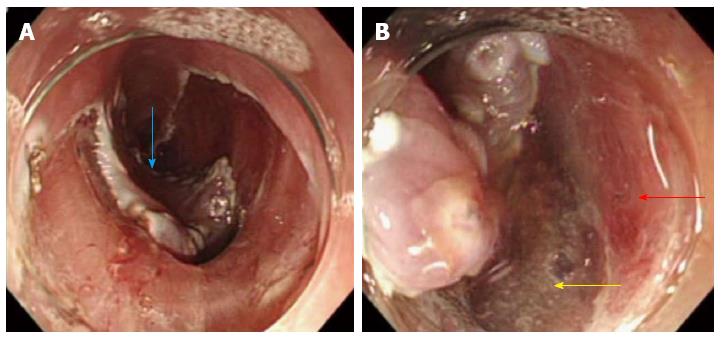
Figure 2 Endoscopic submucosal dissection for esophageal cancer.
A: Depressed area at the center of the lesion became noticeable during the course of submucosal dissection (blue arrow); B: Muscularis propria layer abruptly ended at the center of the cancer lesion. The red arrow indicates the muscularis propria layer, and the yellow arrow indicates the area of the muscularis propria layer defect.
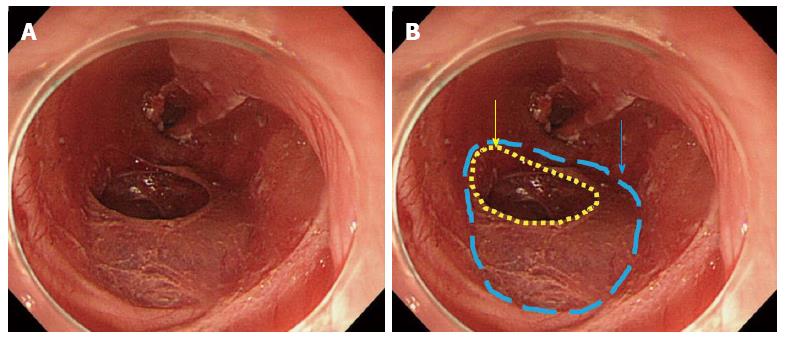
Figure 3 After removing dissected tissue.
A: Ulcer bed after endoscopic submucosal dissection; B: Blue dotted line indicates the defect of the muscularis propria layer, and yellow dotted line indicates the perforation hole.
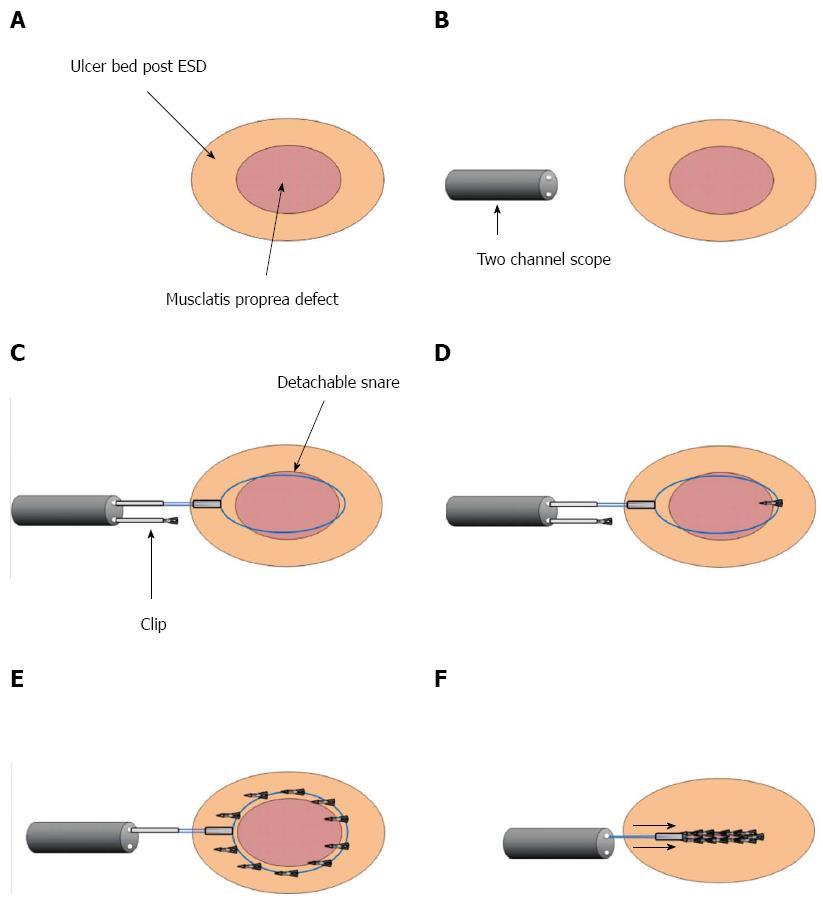
Figure 4 Schema of closure method using detachable snare and clip.
A-D: Detachable snare was fixed with clips surrounding the defect of the muscularis propria layer from the anal to the oral side using a 2-channel scope; E, F: Detachable snare was fixed with about 10 clips. The stopper was tightened and the snare loop was released.
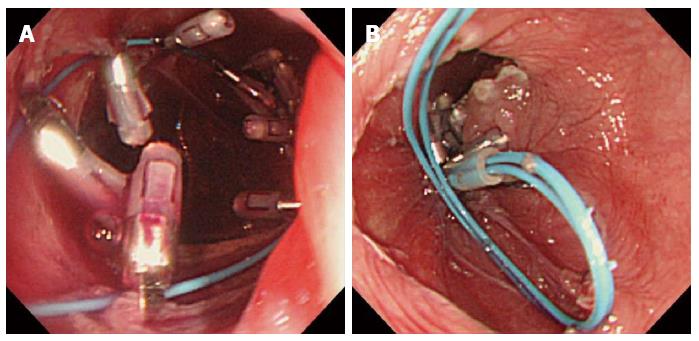
Figure 5 Closing perforated hole.
A, B: Defect of the muscularis propria layer and the perforated hole were successfully sutured.
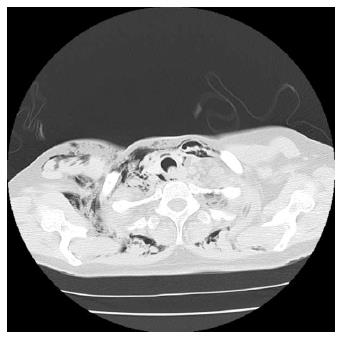
Figure 6 Computed tomography scans immediately after endoscopic submucosal dissection.
Marked mediastinal and subcutaneous emphysema was recognized.
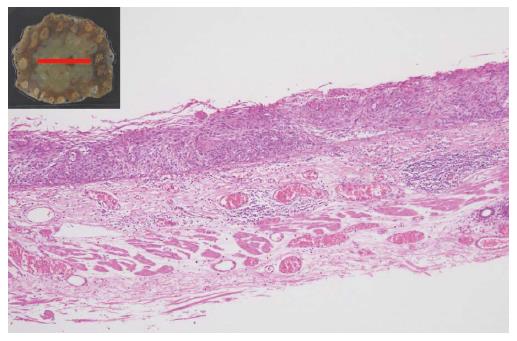
Figure 7 Pathological examination.
Pathological diagnosis revealed that squamous cell carcinoma was retained within epithelial, and the muscularis propria layer was not seen in the resected specimen.
- Citation: Tanaka S, Toyonaga T, Ohara Y, Yoshizaki T, Kawara F, Ishida T, Hoshi N, Morita Y, Azuma T. Esophageal diverticulum exposed during endoscopic submucosal dissection of superficial cancer. World J Gastroenterol 2015; 21(10): 3121-3126
- URL: https://www.wjgnet.com/1007-9327/full/v21/i10/3121.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i10.3121