Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Nov 7, 2014; 20(41): 15200-15215
Published online Nov 7, 2014. doi: 10.3748/wjg.v20.i41.15200
Published online Nov 7, 2014. doi: 10.3748/wjg.v20.i41.15200
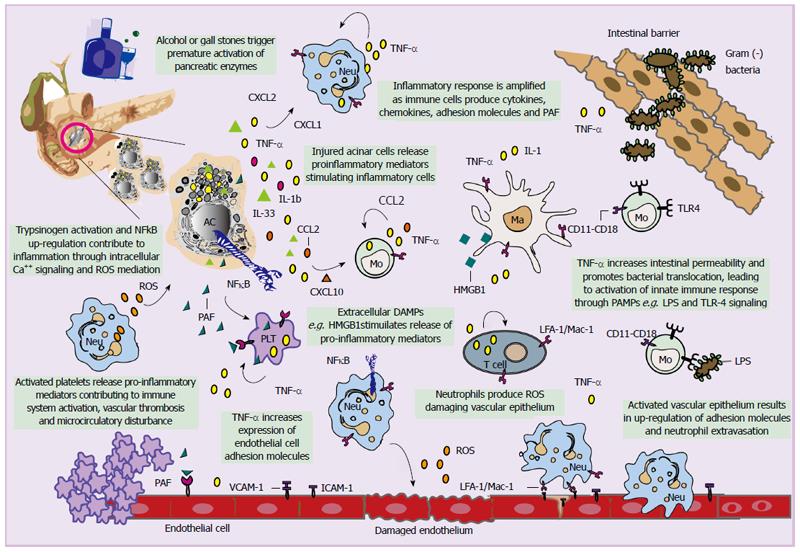
Figure 1 Schematic representation of innate and adaptive immune response mechanisms implicated in acute pancreatitis.
Triggering factors initiate trypsinogen activation and pancreas autophagy. Damaged acinar cells release damage-associated molecular pattern molecules (DAMPs) and pro-inflammatory mediators attracting leukocytes at the site of inflammation. Leukocyte activation leads to increased leukocyte aggregation through increased expression of adhesion molecules and tissue infiltration within the microcirculation. There, these cells increase production of cytokines and other inflammatory mediators including prostaglandins, leukotrienes, thromboxanes, platelet activating factor (PAF), free radicals, nitric oxide and proteases. These substrates increase vascular permeability resulting in neutrophil extravasation and activation, oedema and microvascular disturbances which eventually lead to lack of oxygen and tissue injury. Pro-inflammatory mediators contribute to failure of intestinal barrier function and translocation of intestinal microflora or their products into the vascular bed. Neu: Neutrophil; AC: Acinar cell; Mo: Monocyte; Ma: Macrophage; ICAM-1: intercellular adhesion molecule 1; ROS: Reactive oxygen species; VCAM-1: Vascular adhesion molecule 1; TNF-α: Tumour necrosis factor alpha; NF-κB: Nuclear factor kappa-light-chain-enhancer of activated B cells; IL: Interleukin; CXCL: C-X-C motif chemokine; CCL: Chemokine (C-C motif) ligand; PLT: Platelet; TLR: Toll like receptor; LPS: Lipopolysaccharide; LFA: Lymphocyte function associated antigen; Mac-1: Macrophage-1 antigen.
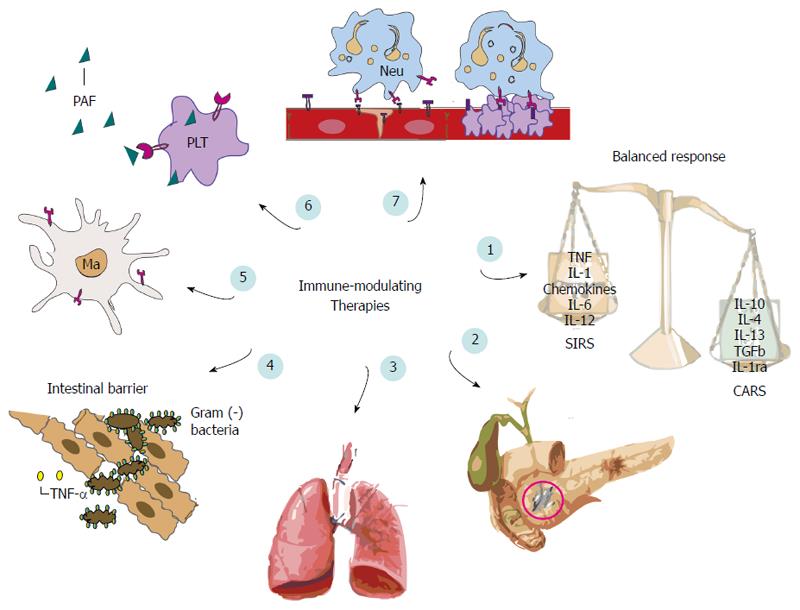
Figure 2 Immune modulating therapies.
(1) Target inflammatory response promoting or attenuating anti and pro-inflammatory mediators respectively (recombinant cytokine/chemokine administration, cytokine/chemokine antagonists, receptor blockade); (2) ameliorate parenchymal and fatty tissue necrosis of the pancreas [e.g., infliximab, blockade of interleukin (IL)-1 receptor, IL-10 blockade, IL-12 suppression, platelet activating factor (PAF)]; (3) alleviate alveolar oedema and development of acute respiratory distress syndrome (e.g., infliximab, IL-10 blockade, IL-8 blockade); (4) correct intestinal barrier and prevent bacterial translocation (e.g., anti-tumour necrosis factor, TNF); (5) modulate immune cell response (e.g., stem cell immunosuppressive strategies); (6) impair platelet activation and further immune activation (e.g., PAF); and (7) protect against endothelial barrier dysfunction, transmigration of neutrophils and concomitant microcirculatory derangements (e.g., adhesion molecule blockade). Ma: Macrophage.
- Citation: Akinosoglou K, Gogos C. Immune-modulating therapy in acute pancreatitis: Fact or fiction. World J Gastroenterol 2014; 20(41): 15200-15215
- URL: https://www.wjgnet.com/1007-9327/full/v20/i41/15200.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i41.15200