Copyright
©2014 Baishideng Publishing Group Co.
World J Gastroenterol. May 14, 2014; 20(18): 5235-5243
Published online May 14, 2014. doi: 10.3748/wjg.v20.i18.5235
Published online May 14, 2014. doi: 10.3748/wjg.v20.i18.5235
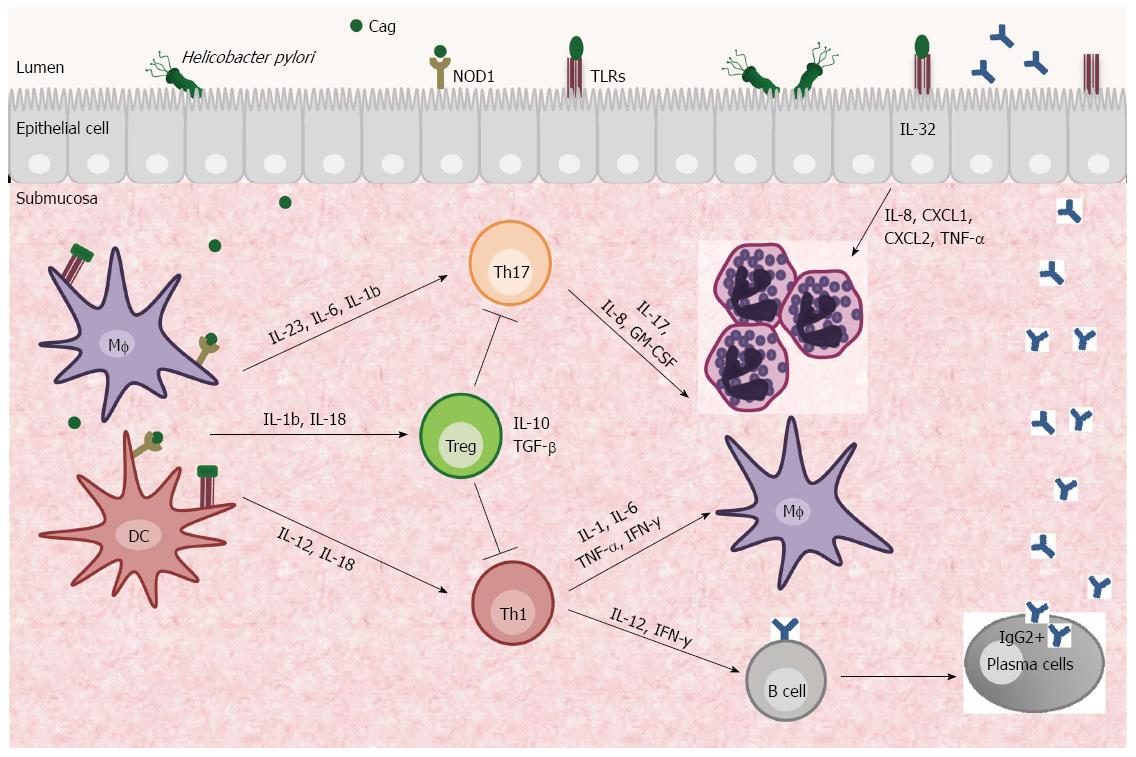
Figure 1 Immunological response elicited by Helicobacter pylori infection.
The presence of Helicobacter pylori (H. pylori) cytotoxins (VacA, CagA, CagL and GGT) and PAMPs (flagella, lipopolysaccharide) in the gastric mucosa activate antigen-presenting cells (APCs), such as dendritic cells and macrophages. These cells stimulate the adaptive immune response through the production of cytokines, such as IL-12 and IL-23, which activate Th1 and Th17 cells, respectively. The cytokines induce an inflammatory process characterization by the recruitment of neutrophils, lymphocytes, macrophages and dendritic cells. Th1 cells release IL-2 and IFN-γ and stimulate B cell differentiation and anti-H. pylori IgG production from secretory plasm cells. Furthermore, epithelial cells recognize the H. pylori antigens and produce IL-32, which induces chemokines and contributes to inflammation. In individuals infected with CagA+ H. pylori, Treg cells are activated by APCs through IL-18 and IL-1β to modulate the immune response and contribute to persistent infection. Consequently, H. pylori-associated pathologies, such as chronic gastritis and gastric adenocarcinoma, may develop. MF: Macrophages; DC: Dendritic cells; PAMPs: Pathogen-Associated Molecular Patterns.
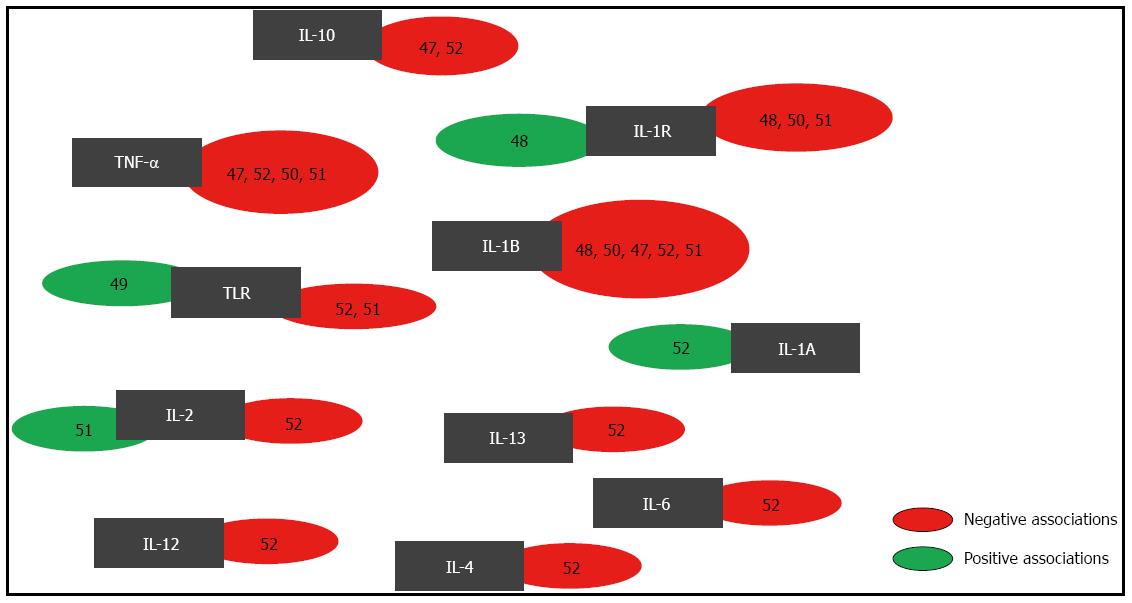
Figure 2 Diagram of the polymorphisms evaluated for risk of Helicobacter pylori infection.
The black boxes contain the cytokines that were studied. In the green boxes on the left are the references of works that identified associations between polymorphisms and Helicobacter pylori (H. pylori) infection, and the red boxes on the right contain the references of publications that identified no associations of polymorphisms with H. pylori infection.
-
Citation: Figueiredo CA, Marques CR, Costa RDS, Silva HBFD, Alcantara-Neves NM. Cytokines, cytokine gene polymorphisms and
Helicobacter pylori infection: Friend or foe? World J Gastroenterol 2014; 20(18): 5235-5243 - URL: https://www.wjgnet.com/1007-9327/full/v20/i18/5235.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i18.5235