Copyright
©2014 Baishideng Publishing Group Co.
World J Gastroenterol. May 7, 2014; 20(17): 4934-4947
Published online May 7, 2014. doi: 10.3748/wjg.v20.i17.4934
Published online May 7, 2014. doi: 10.3748/wjg.v20.i17.4934
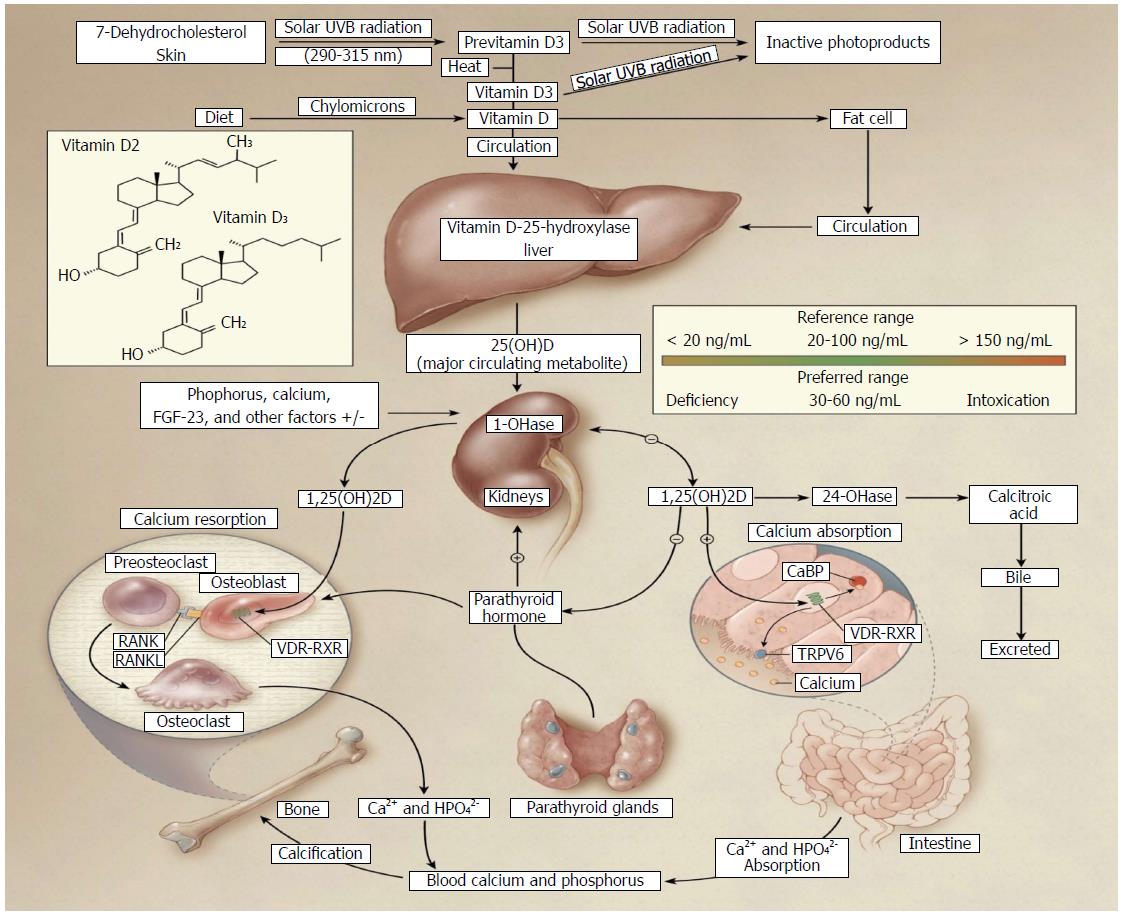
Figure 1 Vitamin D sources and metabolism[8].
Vitamin D can be obtained either from the diet or synthesized in the skin. Under solar ultraviolet (UVB) radiation, 7-dehydrocholesterol in the skin is converted into cholecalciferol (vitamin D3). Vitamin D from the diet enters chylomicrons, which transport it into circulation. Vitamin D is stored in adipose tissue, but when released into circulation, vitamin D binding proteins direct it to the liver where it is converted into its major circulating form, 25-hydroxyvitamin D3 [25(OH)D3] by 25-hydroxylase. In the kidneys, 25(OH)D3 is converted into 1α,25-dihydroxyvitamin D3 [1,25(OH)2D3], the active form, by 1α-hydroxylase. It can now exert its biological effects including calcium absorption, resorption, and bone development. Parathyroid hormone released from the parathyroid glands upregulates hepatic conversion of 1,25(OH)2D3 by stimulating 1α-hydroxylase production; however, autoregulatory mechanisms suppress these actions through negative feedback loops. 1,25(OH)2D3 suppresses parathyroid hormone and 1α-hydroxylase production. Vitamin D is then catabolized by 24-hydroxylase and excreted as calcitroic acid. The recommended optimal range for vitamin D levels is 30-60 ng/mL (75-150 nmol/L). Copyright© 2007 Massachusetts Medical Society. All rights reserved; VDR: Vitamin D receptor; RXR: Retinoid X receptor.
- Citation: Reich KM, Fedorak RN, Madsen K, Kroeker KI. Vitamin D improves inflammatory bowel disease outcomes: Basic science and clinical review. World J Gastroenterol 2014; 20(17): 4934-4947
- URL: https://www.wjgnet.com/1007-9327/full/v20/i17/4934.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i17.4934