Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Nov 21, 2013; 19(43): 7569-7576
Published online Nov 21, 2013. doi: 10.3748/wjg.v19.i43.7569
Published online Nov 21, 2013. doi: 10.3748/wjg.v19.i43.7569
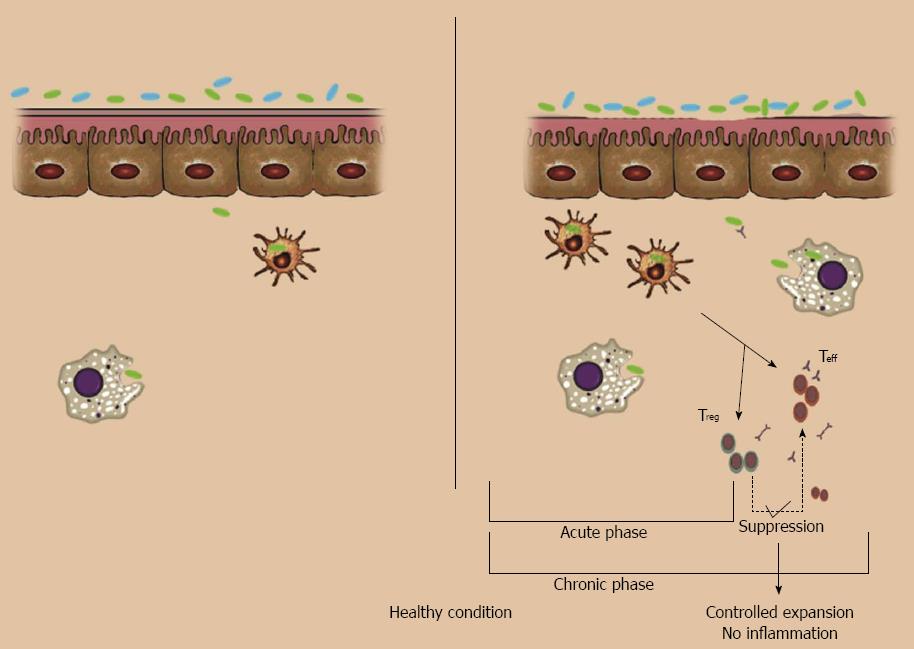
Figure 1 intestinal barrier dysfunction.
Left (normal conditions): no or few commensal bacteria can pass the normal epithelial barrier and those that pass will be swallowed by interstitial macrophages and dendritic cells; it is not necessary to call for adaptive immune cells. Right: in normal situations, if something breaks the barrier (e.g. pathogens and barrier breaker chemicals like ethanol 30%) lots of commensal bacteria in the lumen will pass through the epithelial layer. This acute invasion will be controlled with recruiting of neutrophils and lymphocytes. Even after activation of B cells or T cells, if the defect in barrier function is resolved, apoptotic pathways will control the activated colonies of lymphocytes.
Figure 2 Steps of autoimmunity.
If anything alters the barrier function, lots of luminal antigens can pass to the submucosal layer. If these cells can control the invasion, it is not necessary to call adaptive immunity components, but if the invasion take longer (e.g., in altered tight junction structure) or there are some defects in innate immunity response (e.g., mutations in Toll-like receptors), T cells are activated. If the regulatory system cannot overcome the inflammatory systems, cytokines and reactive destructive mediators further deteriorate the first defect via inducing apoptosis and necrosis in epithelial cells. Activation of T helper type 2 cells leads to a humoral response; also administration of a vaccine of commensal bacteria leads to a humoral immune response to their antigens, so after a disruption in barrier integrity with ethanol, the inflammatory cascade will turn on and induce inflammatory bowel disease in the animal as shown by histopathological findings. TNF: Tumor necrosis factor; TNFR: TNF receptor.
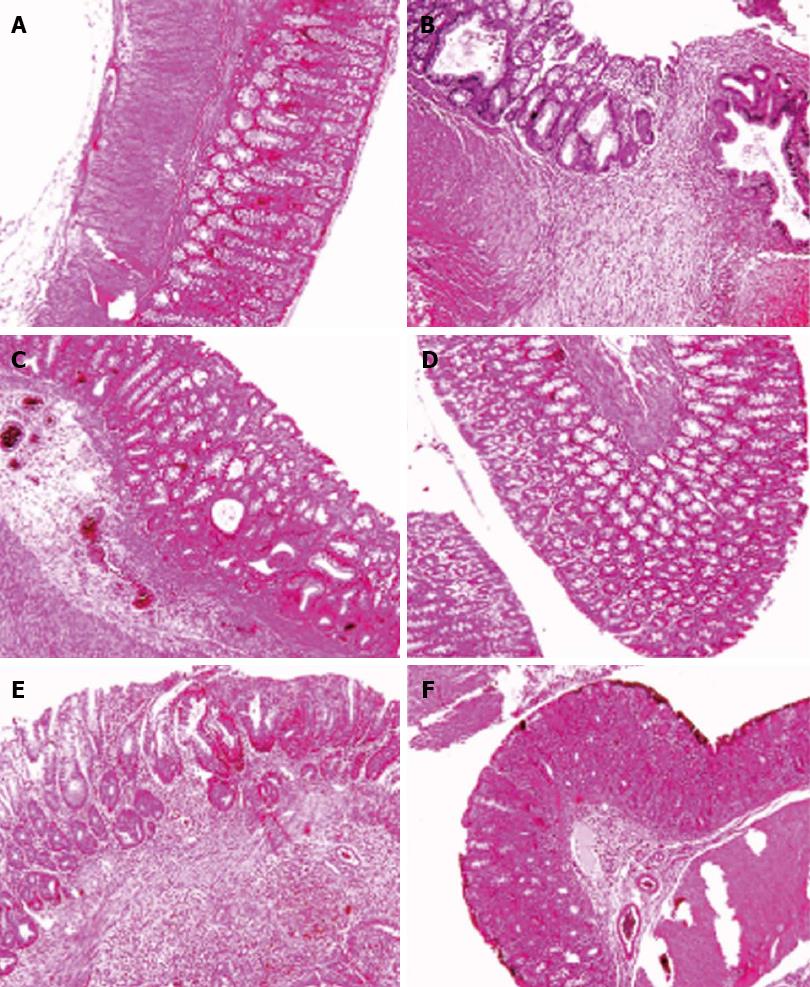
Figure 3 Histological images of colon tissues obtained from different groups.
Microscopic evaluation of the trinitrobenzene sulfonic acid (TNBS) group shows villus atrophy, extensive severe transmural inflammation, granuloma with necrosis and crypt destruction, whereas features in the Sham group were normal. Histological examination of the Ethanol group showed a mild crypt distortion and some crypt abscess, whereas features in the Vaccine group were normal. Microscopic evaluation of the Model group showed mucosal inflammation and crypt distortion, branching and some ulceration with moderate to severe crypt destruction in ulcerated regions. Mild focal inflammation, minimal inflammatory cell infiltration and slight crypt branching were observed in the Infliximab group. A: Sham; B: TNBS; C: Ethanol; D: Vaccine; E: Model; F: Infliximab.
- Citation: Esmaily H, Sanei Y, Abdollahi M. Autoantibodies and an immune-based rat model of inflammatory bowel disease. World J Gastroenterol 2013; 19(43): 7569-7576
- URL: https://www.wjgnet.com/1007-9327/full/v19/i43/7569.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i43.7569