Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Mar 28, 2013; 19(12): 1861-1876
Published online Mar 28, 2013. doi: 10.3748/wjg.v19.i12.1861
Published online Mar 28, 2013. doi: 10.3748/wjg.v19.i12.1861
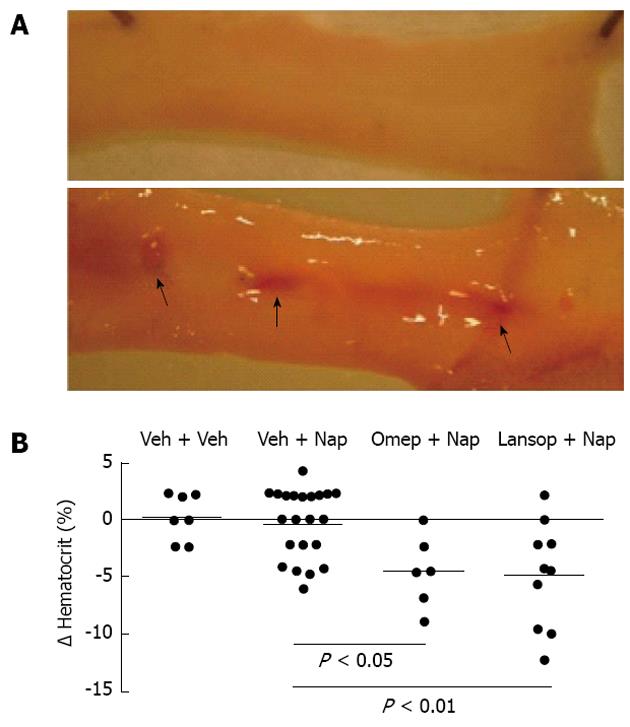
Figure 1 Proton pump inhibitors exacerbate naproxen-induced ulceration and bleeding.
In panel A, the top image is of the jejunum of a rat treated with naproxen for 4.5 d (10 mg/kg twice-daily). There are no ulcers present. The bottom image is of a jejunum of a rat receiving the same naproxen treatment, but also treated with omeprazole at a dose that suppressed gastric acid secretion[37]. The arrows indicate the numerous hemorrhagic ulcers that form with this combination of treatments; Panel B shows the change in hematocrit of rats treated with naproxen (Nap) plus vehicle (Veh), omeprazole (Omep) or lansoprazole (Lansop)[37]. The two proton pump inhibitors significantly enhanced the decrease in hematocrit when co-administered with naproxen (no decrease in hematocrit was observed in rats treated with a proton pump inhibitors alone).
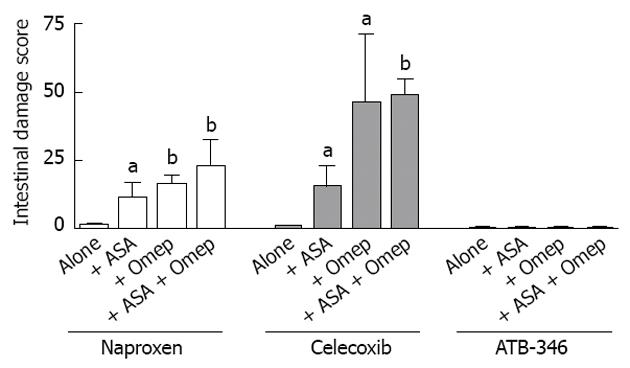
Figure 2 Proton pump inhibitors and low-dose aspirin significantly exacerbate nonsteroidal anti-inflammatory drug-induced small intestinal ulceration.
Rats were treated orally, twice-daily for 4.5 d with equi-effective anti-inflammatory doses of naproxen (10 mg/kg), celecoxib (10 mg/kg) or ATB-346 (14.5 mg/kg). ATB-346 is a hydrogen sulfide-releasing derivative of naproxen[38]. Starting 5 d before the nonsteroidal anti-inflammatory drugs (NSAIDs), the rats began receiving twice-daily treatments with omeprazole (Omep) (10 mg/kg) or vehicle. Starting 3 d before the NSAIDs, the rats began receiving daily doses of low-dose aspirin (10 mg/kg) or vehicle. The results are shown as the mean ± SE of at least 6 rats per group. aP < 0.05, bP < 0.01 vs the corresponding group treated with the NSAID alone. No intestinal damage was observed in rats treated with aspirin (ASA) alone. The exacerbation of small intestinal ulceration with omeprazole was also observed with another proton pump inhibitor, lanzoprazole[37]. This figure was constructed using data from Blackler et al[175].
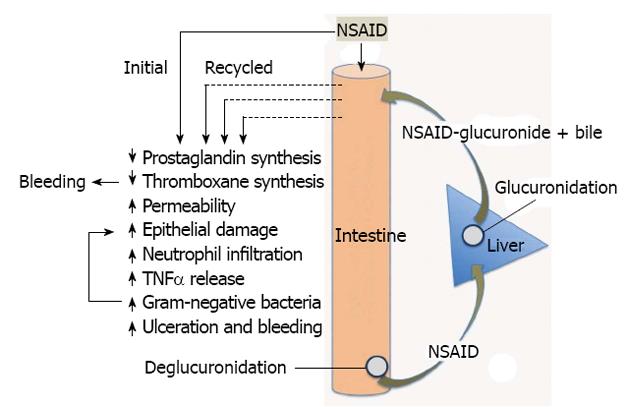
Figure 3 Pathogenesis of nonsteroidal anti-inflammatory drugs-Induced enteropathy.
Nonsteroidal anti-inflammatory drugs (NSAIDs) produce effects during their initial exposure to the small intestine, and when secreted back into the proximal small intestine, along with bile, following their absorption in the distal intestine, and glucuronidation in the liver. Suppression of thromboxane synthesis likely plays an important role in promoting bleeding (especially with aspirin, an irreversible inhibitor of platelet thromboxane synthesis). Repeated exposure of the intestinal epithelium to the combination of NSAIDs and bile will promote damage, and the damage is likely exacerbated by the shift in intestinal bacteria stimulated by the NSAID (elevated gram-negative bacteria). These effects appear to be mediated by endotoxin, acting at least in part through toll-like receptor-4. The interplay among bile, bacteria and recirculation of the NSAID is complex. For example, bacterial enzymes convert primary bile acids to secondary bile acids (which may be more damaging) and bacterial enzymes are necessary for deglucuronidation, which permits reabsorption and enterohepatic recirculation of NSAIDs. TNFα: Tumor necrosis factor-alpha.
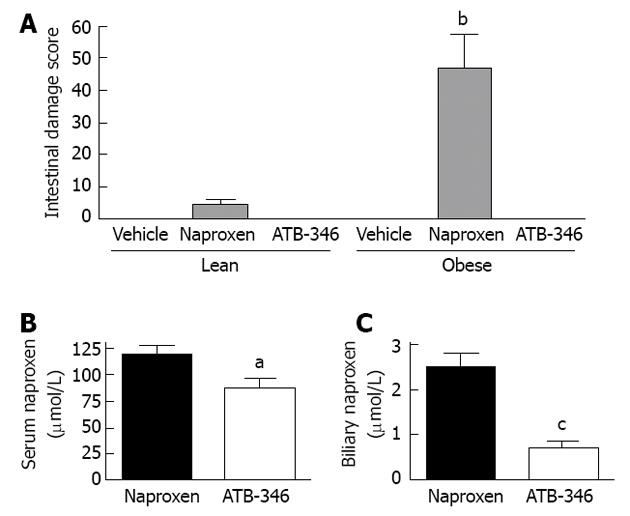
Figure 4 Intestinal safety and altered biliary excretion of ATB-346.
A: ATB-346 is a hydrogen sulfide-releasing derivative of naproxen[38].When administered to obese Zucker rats, twice-daily for 4.5 d at 10 mg/kg, naproxen induced small intestinal damage that was significantly more severe in the obese rats (bP < 0.01). However, at an equimolar dose, ATB-346 did not induce intestinal damage in lean or obese rats[175]; B: The serum levels of naproxen in normal rats after 4.5 d of twice-daily administration of ATB-346 were marginally, but significantly (aP < 0.05) lower than those in rats treated with an equimolar dose of naproxen; C: Biliary levels of naproxen in rats treated with ATB-346 (as above) were markedly reduced compared to those in rats treated with an equimolar dose of naproxen (cP < 0.001).The data shown in this graph are from Blackler et al[175].
- Citation: Wallace JL. Mechanisms, prevention and clinical implications of nonsteroidal anti-inflammatory drug-enteropathy. World J Gastroenterol 2013; 19(12): 1861-1876
- URL: https://www.wjgnet.com/1007-9327/full/v19/i12/1861.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i12.1861