Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Mar 28, 2013; 19(12): 1861-1876
Published online Mar 28, 2013. doi: 10.3748/wjg.v19.i12.1861
Published online Mar 28, 2013. doi: 10.3748/wjg.v19.i12.1861
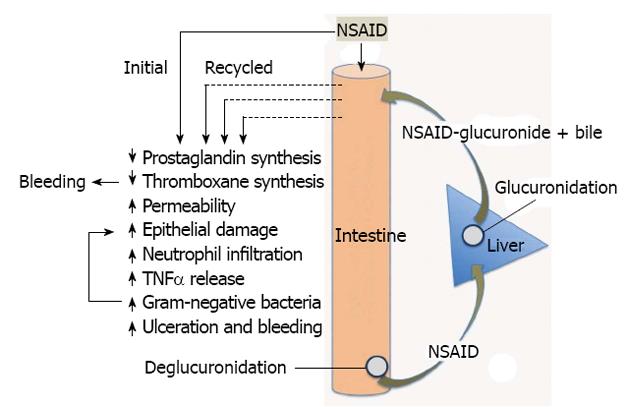
Figure 3 Pathogenesis of nonsteroidal anti-inflammatory drugs-Induced enteropathy.
Nonsteroidal anti-inflammatory drugs (NSAIDs) produce effects during their initial exposure to the small intestine, and when secreted back into the proximal small intestine, along with bile, following their absorption in the distal intestine, and glucuronidation in the liver. Suppression of thromboxane synthesis likely plays an important role in promoting bleeding (especially with aspirin, an irreversible inhibitor of platelet thromboxane synthesis). Repeated exposure of the intestinal epithelium to the combination of NSAIDs and bile will promote damage, and the damage is likely exacerbated by the shift in intestinal bacteria stimulated by the NSAID (elevated gram-negative bacteria). These effects appear to be mediated by endotoxin, acting at least in part through toll-like receptor-4. The interplay among bile, bacteria and recirculation of the NSAID is complex. For example, bacterial enzymes convert primary bile acids to secondary bile acids (which may be more damaging) and bacterial enzymes are necessary for deglucuronidation, which permits reabsorption and enterohepatic recirculation of NSAIDs. TNFα: Tumor necrosis factor-alpha.
- Citation: Wallace JL. Mechanisms, prevention and clinical implications of nonsteroidal anti-inflammatory drug-enteropathy. World J Gastroenterol 2013; 19(12): 1861-1876
- URL: https://www.wjgnet.com/1007-9327/full/v19/i12/1861.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i12.1861