Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Mar 14, 2013; 19(10): 1563-1571
Published online Mar 14, 2013. doi: 10.3748/wjg.v19.i10.1563
Published online Mar 14, 2013. doi: 10.3748/wjg.v19.i10.1563
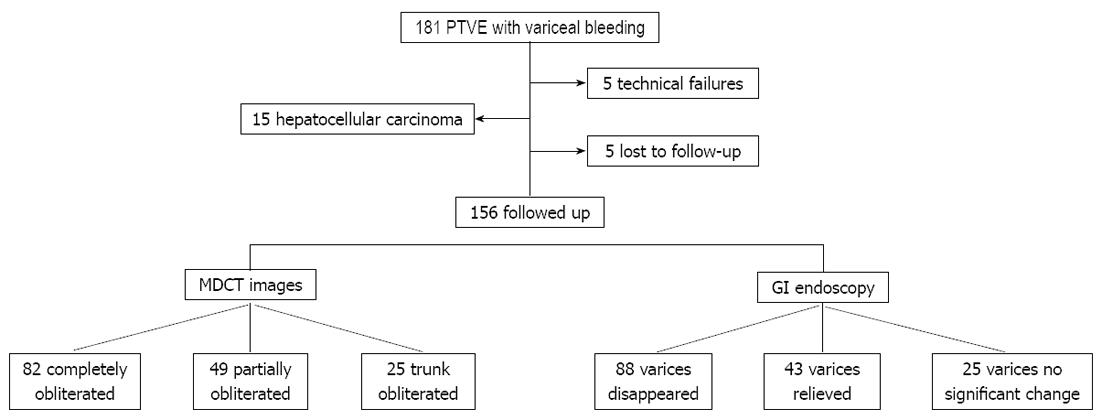
Figure 1 Study flow chart.
PTVE: Percutaneous transhepatic variceal embolization; MDCT: Multi-detector row computed tomography; GI: Gastrointestinal.
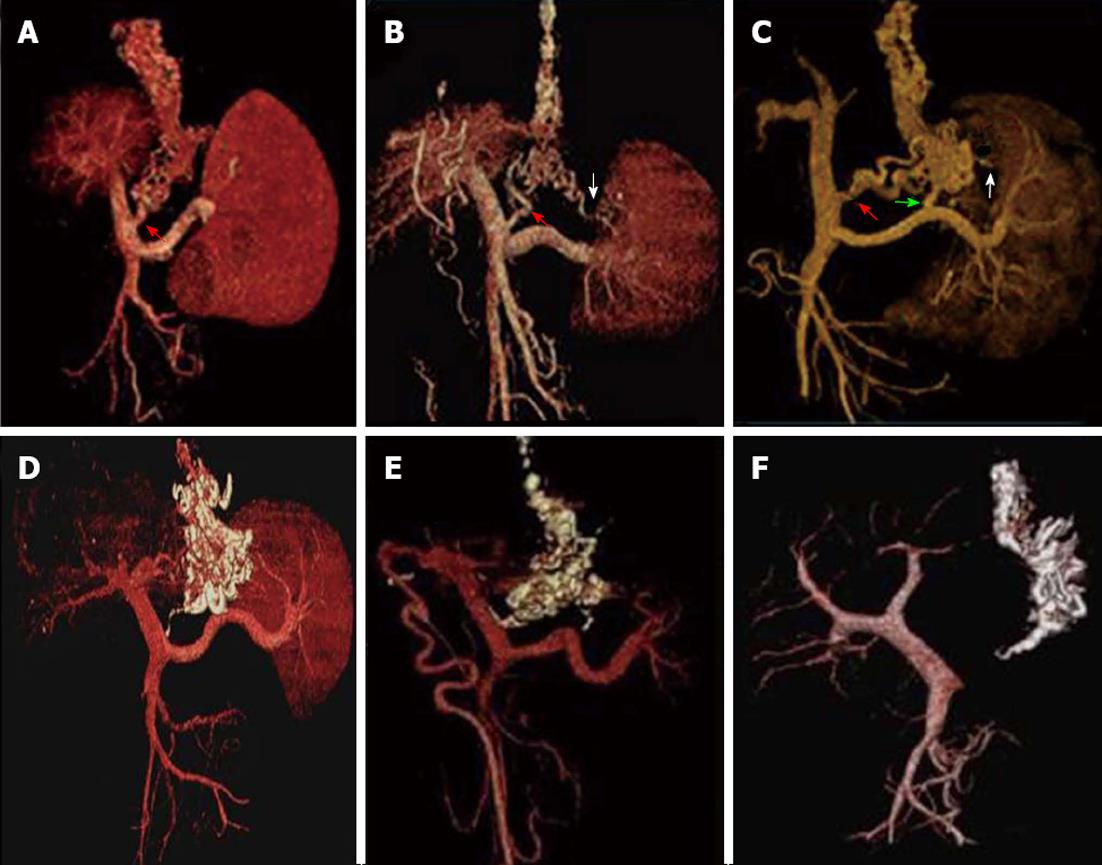
Figure 2 Volume rendering of the multi-detector row computed tomography angiography data set during the portal venous phase demonstrated the esophageal-gastric varices and their afferent vessels before and after percutaneous transhepatic variceal embolization.
A-C: Volume rendering of multi-detector row computed tomography angiography data set during the portal venous phase demonstrates the esophageal-gastric varices and their afferent vessels (left gastric vein (LGV) only for A, LGV and short gastric vein (SGV) for B, LGV, posterior gastric vein and SGV for C); D-F: All varices and their feeding vessels are completely filled with cyanoacrylate (arrows) after percutaneous transhepatic variceal embolization; no flow signals were revealed in any of the cases.
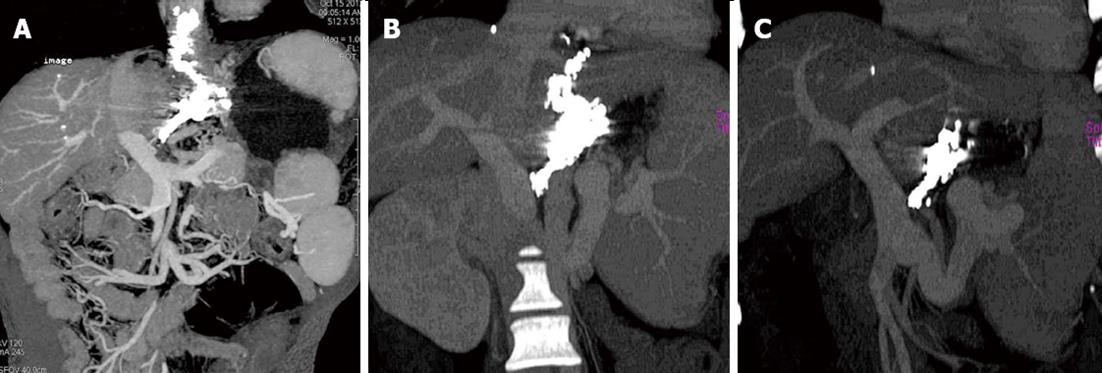
Figure 3 Coronal thin-slab maximum intensity projection of multi-detector row computed tomography angiography during the portal venous phase demonstrates the three different obliteration types of cyanoacrylate.
A: Complete obliteration: with the lower esophageal varices (EVs) and peri-/para-EVs, as well as the adventitial plexus of the gastric cardia and fundus, filled with cyanoacrylate; B: Partial obliteration: along with the left gastric vein (LGV) and its main branches being obliterated with cyanoacrylate, the varices surrounding the gastric cardia and fundus are also obliterated, but without reaching the lower EVs; C: Trunk obliteration: cyanoacrylate mainly obliterates the LGV and its main branches outside of the gastric wall.
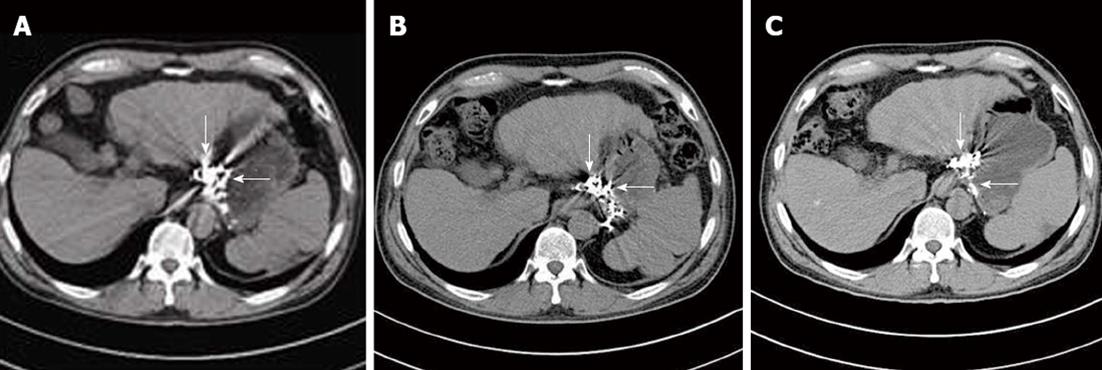
Figure 4 Computed tomography image follow-up revealed the different outcome of cyanoacrylate in the different veins: cyanoacrylate in submucosal varices (within the wall of the fundus, large arrow) disappeared with time, but those in the para- and peri-gastric varices (outside the wall of the fundus, small arrow) remained permanently in the vessels without a time-dependent decrease.
A: The cyanoacrylate in both the gastric varices and peri-and para-gastric varices stayed full at 3 mo after percutaneous transhepatic variceal embolization (PTVE); B: The cyanoacrylate in the gastric varices was reduced at 6 mo after PTVE; C: The cyanoacrylate in the gastric varices nearly disappeared at 12 mo after PTVE, but the cyanoacrylate in the peri- and para-gastric vessels retained the same as before.
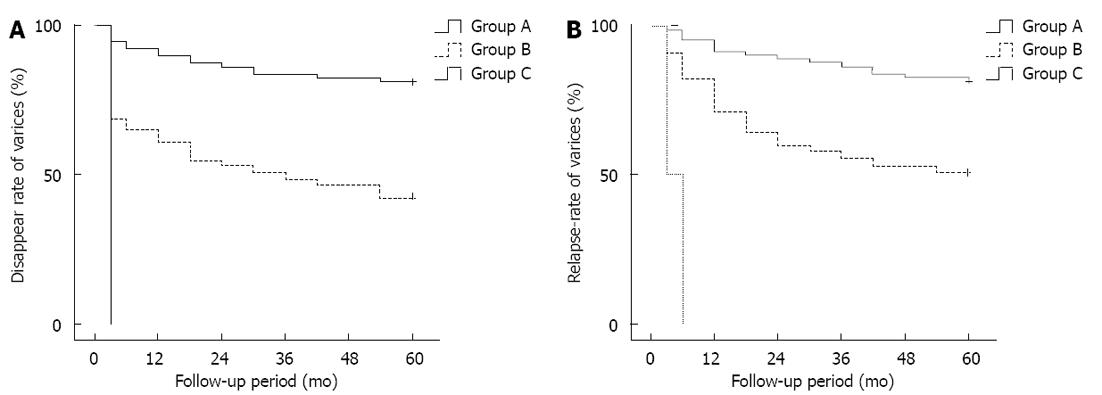
Figure 5 Kaplan-Meier analysis of the disappearance rate (A) and non-relapse rate (B) of varices shown at gastroscopy during the follow-up.
Group A: Complete obliteration; Group B: Partial obliteration; Group C: Trunk obliteration.
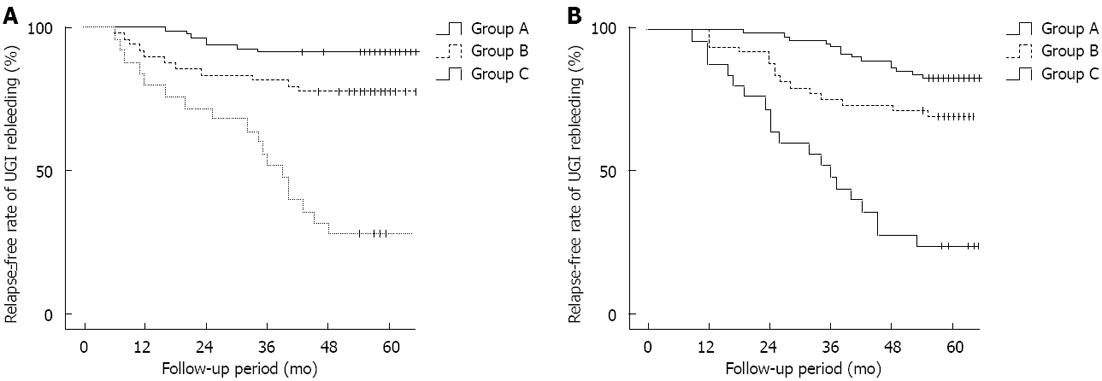
Figure 6 Kaplan-Meier analysis of non-rebleeding (A) and survival rates (B) among the different obliteration types after modified percutaneous transhepatic variceal embolization.
Group A: Complete obliteration; Group B: Partial obliteration; Group C: trunk obliteration.
- Citation: Sun A, Shi YJ, Xu ZD, Tian XG, Hu JH, Wang GC, Zhang CQ. MDCT angiography to evaluate the therapeutic effect of PTVE for esophageal varices. World J Gastroenterol 2013; 19(10): 1563-1571
- URL: https://www.wjgnet.com/1007-9327/full/v19/i10/1563.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i10.1563