Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Jan 7, 2013; 19(1): 35-41
Published online Jan 7, 2013. doi: 10.3748/wjg.v19.i1.35
Published online Jan 7, 2013. doi: 10.3748/wjg.v19.i1.35
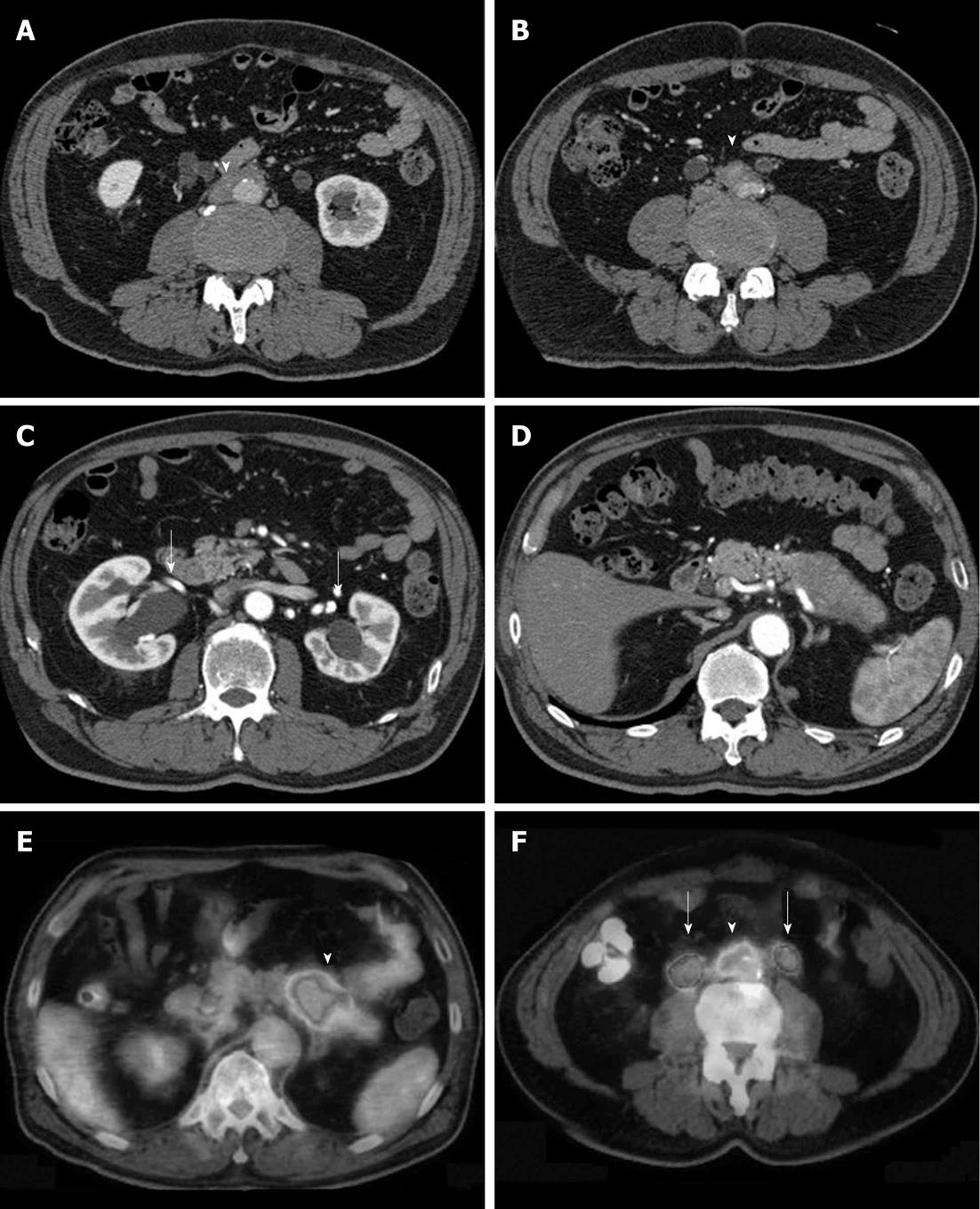
Figure 1 Typical retroperitoneal fibrosis associated with autoimmune pancreatitis.
A, B: Soft tissue (arrow) surrounds the abdominal aorta and common iliac artery; C: Bilateral hydronephrosis (arrows); D: Swelling and capsule-like rim are seen in the body and tail of the pancreas. This case was diagnosed as autoimmune pancreatitis; E, F: Fluorodeoxyglucose positron emission tomography images from the same patient; high fluorodeoxyglucose uptake is seen in the body and tail of the pancreas (arrowhead) and in the retroperitoneal fibrosis lesions (arrowhead) surrounding the common iliac artery (arrows indicate dilated urinary ducts).
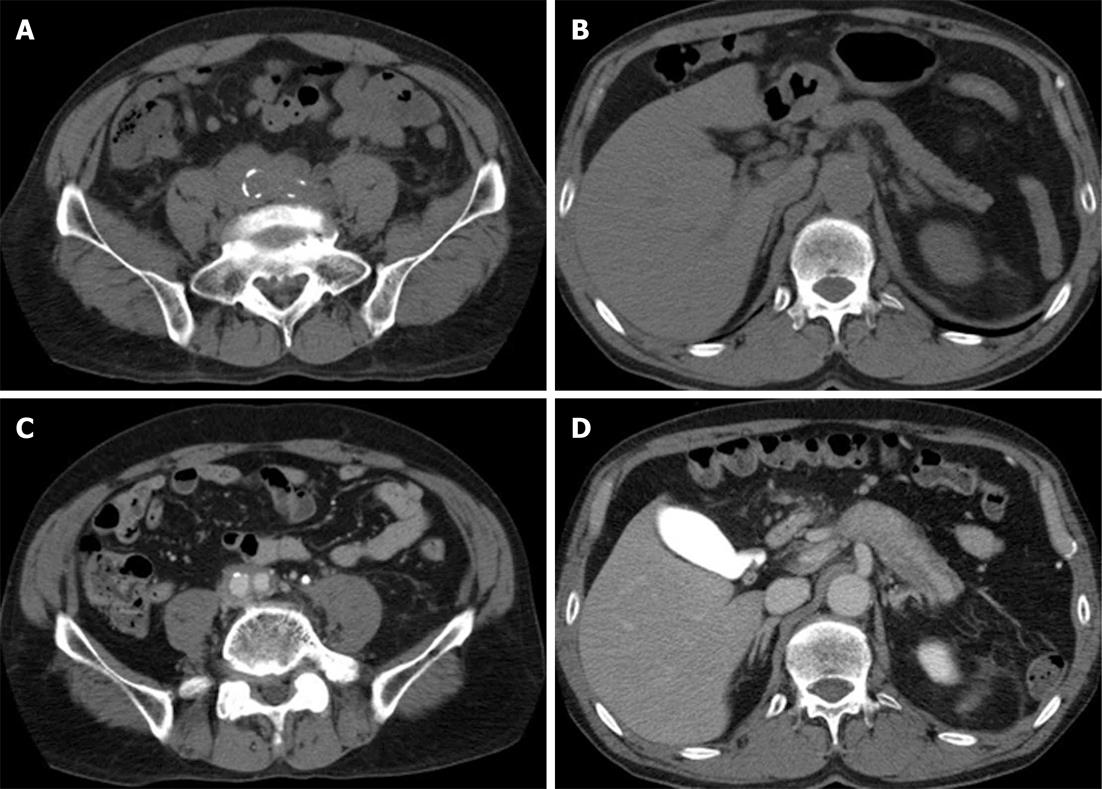
Figure 2 Retroperitoneal fibrosis occurring before the onset of autoimmune pancreatitis.
A 65-year-old man developed hydronephrosis and renal failure. A, B: Soft tissue was observed surrounding the abdominal aorta and common iliac artery. No abnormality was found in the pancreas. The patient was diagnosed with idiopathic retroperitoneal fibrosis, and started receiving prednisolone (PSL) at the dose of 40 mg/d. The dose was gradually reduced over approximately 6 mo and discontinued. The hydronephrosis improved, and the patient continued to be followed up; C, D: Swelling of the pancreas observed on computed tomography images taken about 1 yr and 6 mo after the discontinuation of PSL. Compared with the initial observation, retroperitoneal fibrosis improved, but persisted. The serum immunoglobulin G4 level was 366 mg/dL. At that point, the patient was diagnosed with autoimmune pancreatitis, and started receiving PSL again at the dose of 40 mg/d. The swelling of the pancreas and retroperitoneal fibrosis were improved.
- Citation: Fujimori N, Ito T, Igarashi H, Oono T, Nakamura T, Niina Y, Hijioka M, Lee L, Uchida M, Takayanagi R. Retroperitoneal fibrosis associated with immunoglobulin G4-related disease. World J Gastroenterol 2013; 19(1): 35-41
- URL: https://www.wjgnet.com/1007-9327/full/v19/i1/35.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i1.35