Copyright
©2012 Baishideng Publishing Group Co.
World J Gastroenterol. Nov 7, 2012; 18(41): 5870-5878
Published online Nov 7, 2012. doi: 10.3748/wjg.v18.i41.5870
Published online Nov 7, 2012. doi: 10.3748/wjg.v18.i41.5870
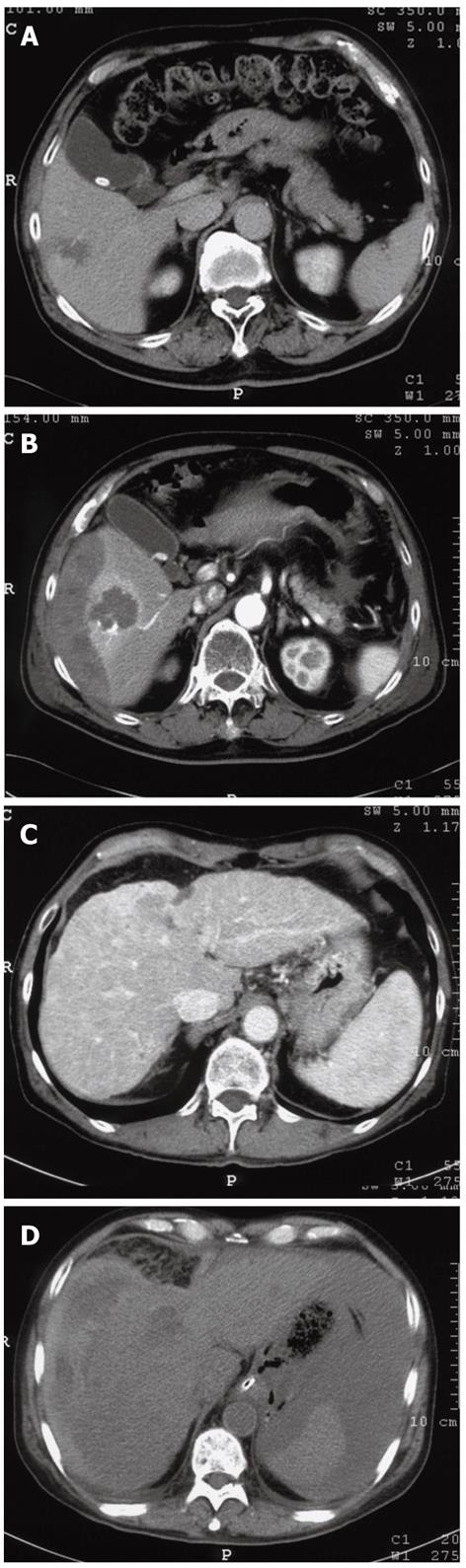
Figure 1 A case showing subcapsular (A, B) and intraperitoneal (C, D) hemorrhage after popping, which occurred during radiofrequency ablation for hepatocellular carcinoma.
A, C: Before ablation; B, D: After ablation. RFA: Radiofrequency ablation; HCC: Hepatocellular carcinoma.
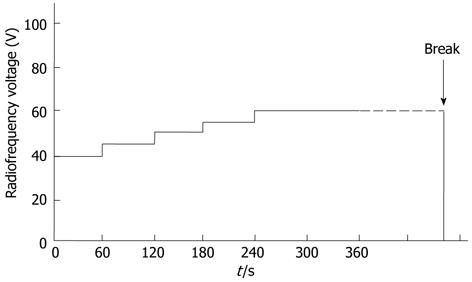
Figure 2 The ablation protocol to avoid popping involves the initiation of power delivery from 40 V with increases of 5 V every minute to a maximum of 60 V until a break is observed.
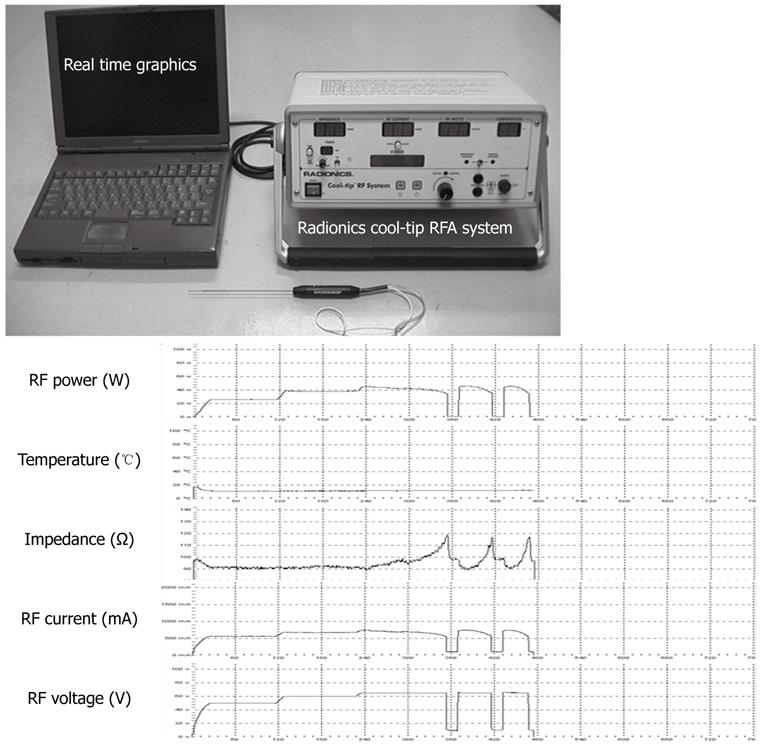
Figure 3 Radio frequency power, radio frequency current, radio frequency voltage, temperature and impedance were intraoperatively monitored using the equipment as shown in the diagram.
RF: Radio frequency.
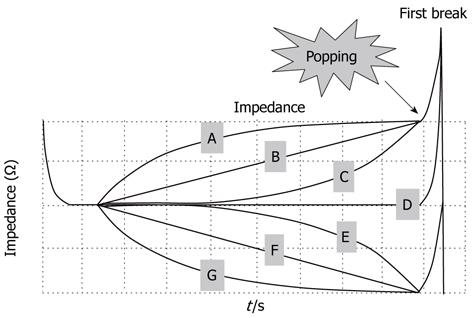
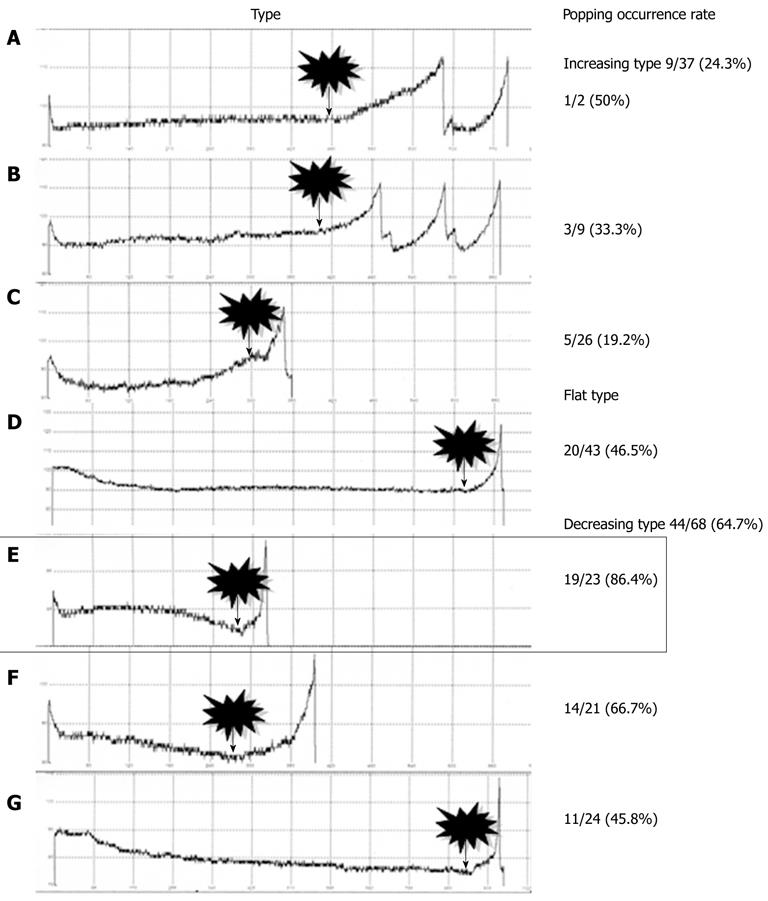
Figure 4 The graph showing the characteristic impedance curve shapes leading to the break point.
The graph showing the seven characteristic impedance curves leading to the break point, which dictated the subgroups into which the previously classified nodules were further sorted. A-C: Increasing type; D: Flat type; E-G: Decreasing type; B, D, F: Three characteristic impedance curve shapes leading to the first break point, into which the 148 nodules were classified: increasing, flat and decreasing.
Figure 5 Subtype E (nodules that showed a rapid decrease in impedance during the latter half of the ablation) exhibited a significantly higher rate of popping compared to subtypes B, C, D and G (P < 0.
05). Decreasing-type nodules exhibited a significantly higher rate of popping compared to increasing-type nodules (P < 0.0001). Flat-type nodules exhibited a significantly higher rate of popping compared to increasing-type nodules (P = 0.039).
- Citation: Iida H, Aihara T, Ikuta S, Yamanaka N. Effectiveness of impedance monitoring during radiofrequency ablation for predicting popping. World J Gastroenterol 2012; 18(41): 5870-5878
- URL: https://www.wjgnet.com/1007-9327/full/v18/i41/5870.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i41.5870