Copyright
©2012 Baishideng Publishing Group Co.
World J Gastroenterol. Mar 28, 2012; 18(12): 1373-1378
Published online Mar 28, 2012. doi: 10.3748/wjg.v18.i12.1373
Published online Mar 28, 2012. doi: 10.3748/wjg.v18.i12.1373
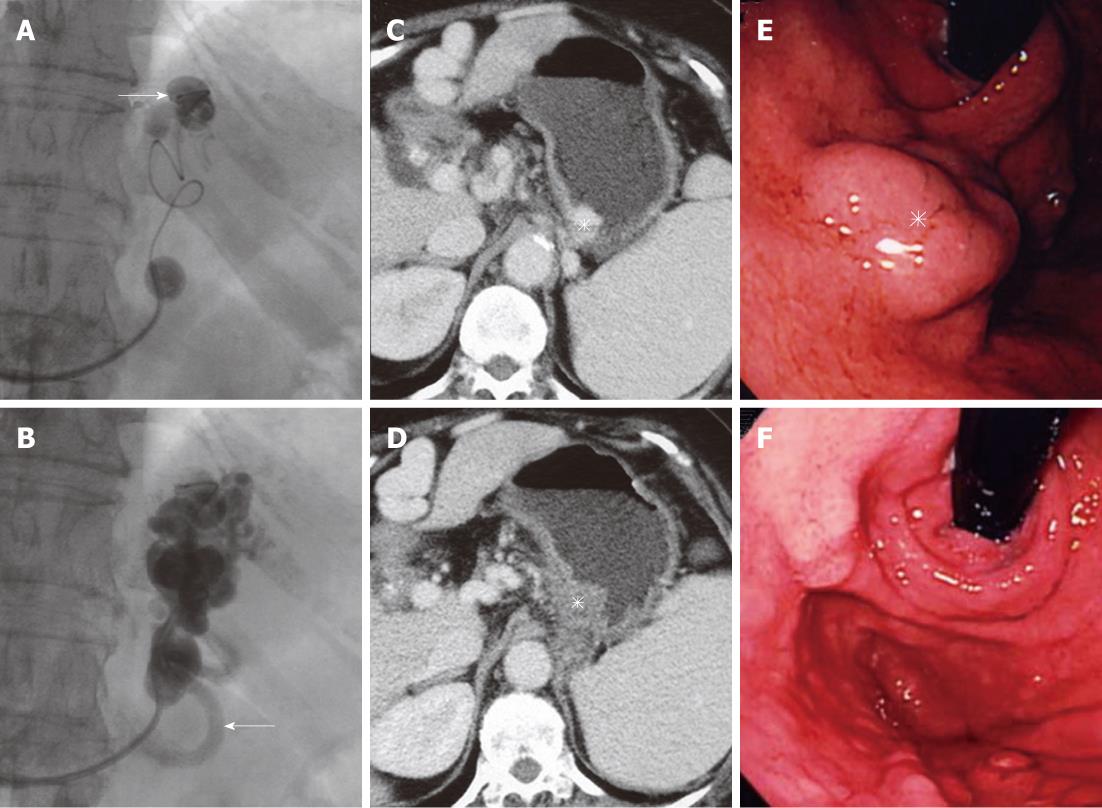
Figure 1 Selective injection of the sclerosant.
A: A microcatheter is navigated close to the gastric varices, and the sclerosant is selectively injected through the microcatheter (arrow); B: The gastric varices and gastrorenal shunt are fully filled with the sclerosant with contrast medium, and the afferent vein (arrow) is opacified; C: Contrast-enhanced computed tomography (CE-CT) before balloon-occluded retrograde transvenous obliteration (BRTO) shows gastric varices (asterisk); D: CE-CT one week after BRTO shows complete thrombosis of the varices (asterisk); E: Endoscopy before BRTO shows tumor-like varices (asterisk) in the fornix of the stomach; F: Endoscopy 3 mo after BRTO shows complete disappearance of the varices.
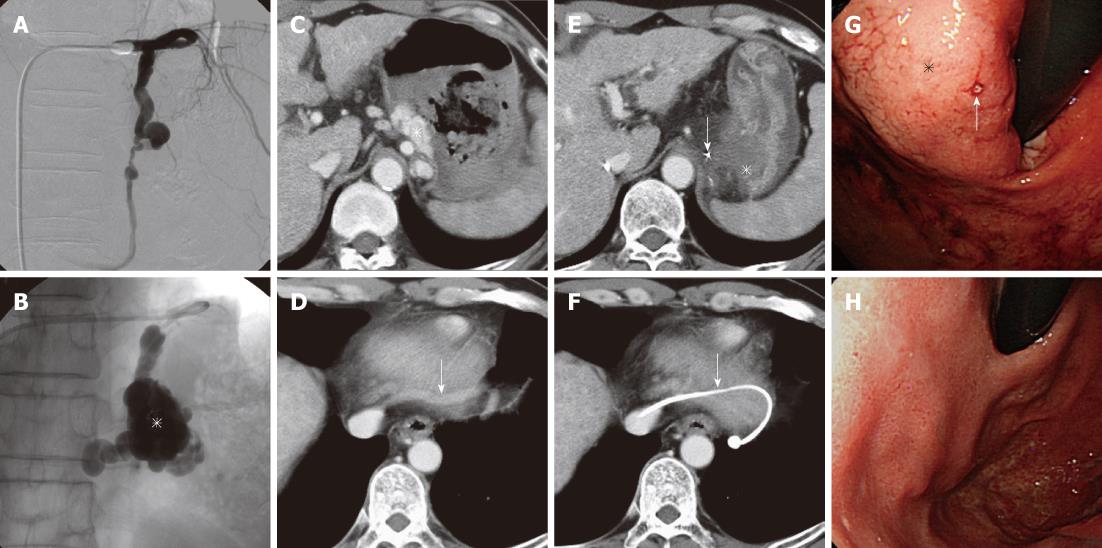
Figure 2 Selective injection of the sclerosant.
A: A balloon catheter is inserted into the gastrocaval shunt. Balloon-occluded venography shows no gastric varices; B: The balloon catheter is advanced further into the shunt, and the sclerosant is selectively injected through the microcatheter which is navigated close to the gastric varices. The varices (asterisk) are opacified sufficiently; C: Contrast-enhanced computed tomography (CE-CT) shows the varices (asterisk) and a large amount of hematomas in the stomach; D: The gastrocaval shunt (arrow) flows into the inferior vena cava; E: CE-CT next day shows complete thrombosis of the gastric varices (asterisk) and the tip of the microcatheter (arrow) close to the varices; F: CE-CT shows the balloon catheter in the shunt (arrow); G: Endoscopy before balloon-occluded retrograde transvenous obliteration (BRTO) shows large gastric varices (asterisk) with a bleeding site (arrow); H: Endoscopy 3 mo after BRTO shows complete disappearance of the varices.
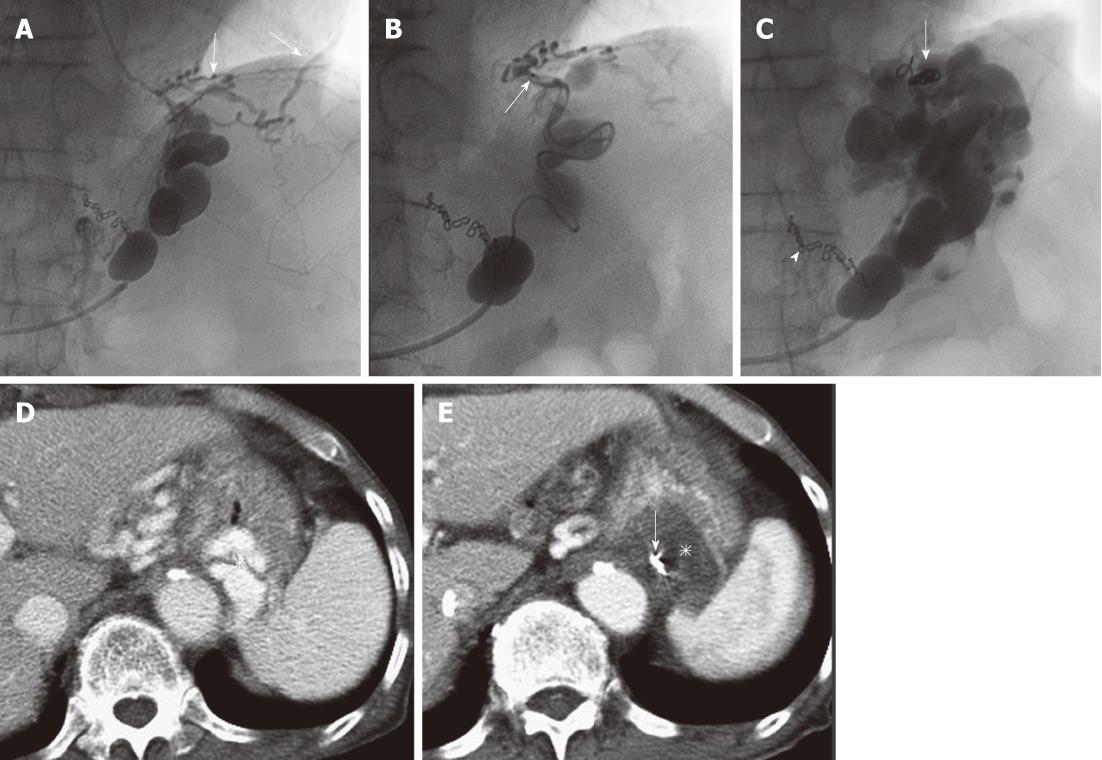
Figure 3 Microcoil embolization of collateral veins.
A: Pericardiophrenic veins (arrows) develop as collateral draining veins; B: A microcatheter (arrow) is navigated into the pericardiophrenic vein and microcoil embolization is performed; C: The sclerosant is selectively injected through the microcatheter which is withdrawn a little, and the gastric varices are opacified sufficiently. Microcoils (arrow) from embolization and surgical clips from previous operation of gastric cancer. (arrowhead) are seen; D: Contrast-enhanced computed tomography (CE-CT) before balloon-occluded retrograde transvenous obliteration (BRTO) shows gastric varices (asterisk); E: CE-CT next day after BRTO shows complete thrombosis of the varices (asterisk) and microcoils close to the varices (arrow).
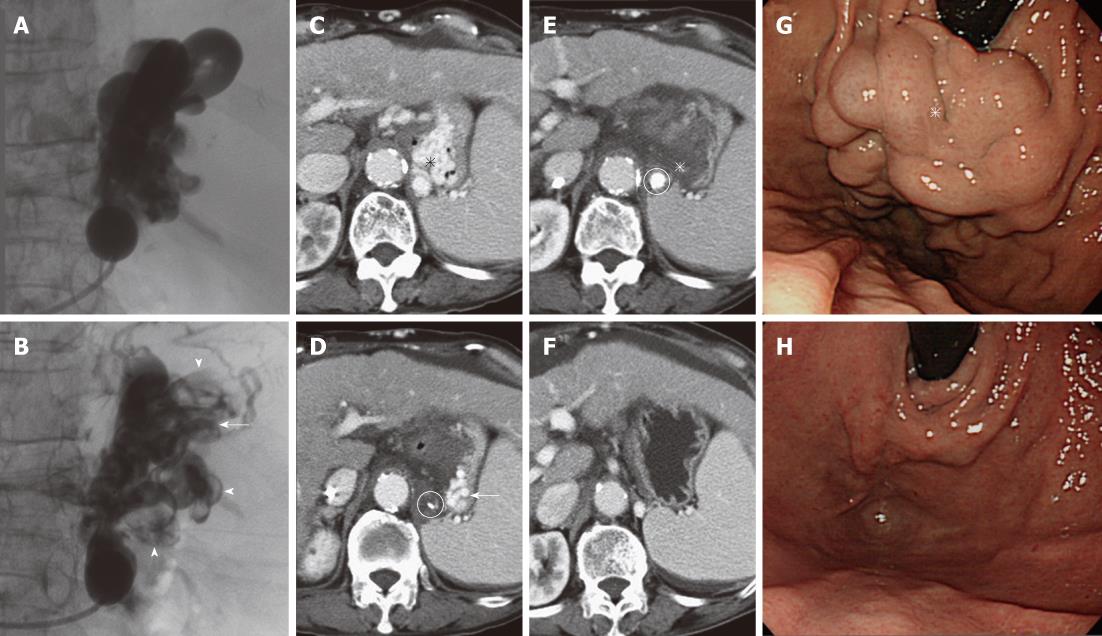
Figure 4 Additional injection of the sclerosant.
A: Fluoroscopic image obtained during the first balloon-occluded retrograde transvenous obliteration (BRTO) shows full opacification of the gastric varices and gastrorenal shunt; B: Fluoroscopic image obtained during the second BRTO (next day) shows partial opacification of the varices and shunt, suggesting residual varices (arrow) and thrombosis of the varices and shunt (arrowheads); C: Contrast-enhanced computed tomography (CE-CT) before BRTO shows large varices (asterisk); D: CE-CT after the first BRTO shows residual varices (arrow) in the lateral portion of the stomach. The microcatheter tip (circle) is in the gastrorenal shunt close to the varices; E: CE-CT after the second BRTO shows complete thrombosis of the varices (asterisk). The sclerosant with contrast medium (circle) is detected in the gastrorenal shunt; F: CE-CT 3 mo after BRTO shows complete disappearance of the varices; G: Endoscopy before BRTO shows bulky varices (asterisk); H: Endoscopy 3 mo after BRTO shows complete disappearance of the varices.
- Citation: Sonomura T, Ono W, Sato M, Sahara S, Nakata K, Sanda H, Kawai N, Minamiguchi H, Nakai M, Kishi K. Three benefits of microcatheters for retrograde transvenous obliteration of gastric varices. World J Gastroenterol 2012; 18(12): 1373-1378
- URL: https://www.wjgnet.com/1007-9327/full/v18/i12/1373.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i12.1373