Copyright
©2010 Baishideng.
World J Gastroenterol. Mar 7, 2010; 16(9): 1150-1154
Published online Mar 7, 2010. doi: 10.3748/wjg.v16.i9.1150
Published online Mar 7, 2010. doi: 10.3748/wjg.v16.i9.1150
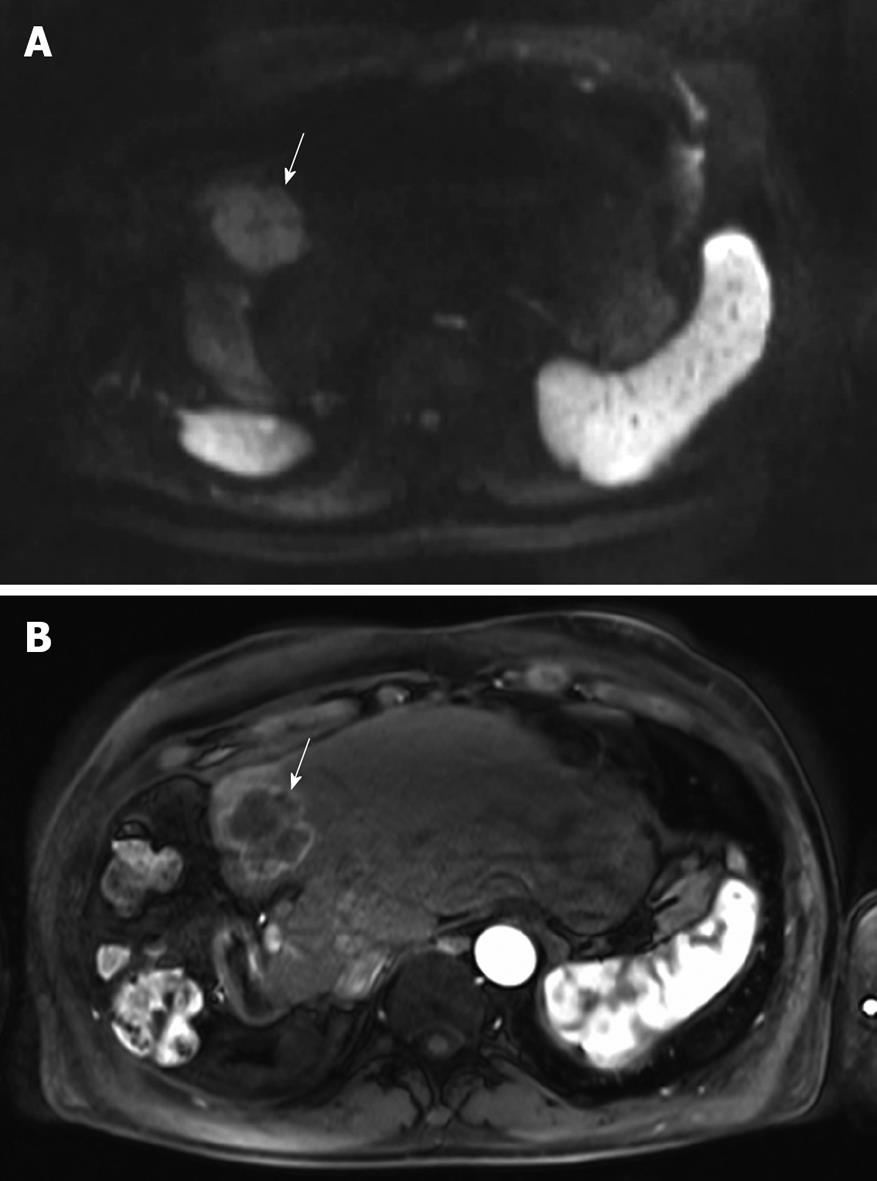
Figure 1 Magnetic resonance imaging (MRI) of the liver before starting hepatic arterial infusion (HAI).
A: The hyperintensity of the solitary large (5 cm) metastasis in segment 4 (arrow) on the axial diffusion-weighted image is consistent with malignancy; B: The metastasis is hypervascular (arrow) on the arterial phase after injection of gadolinium chelate.
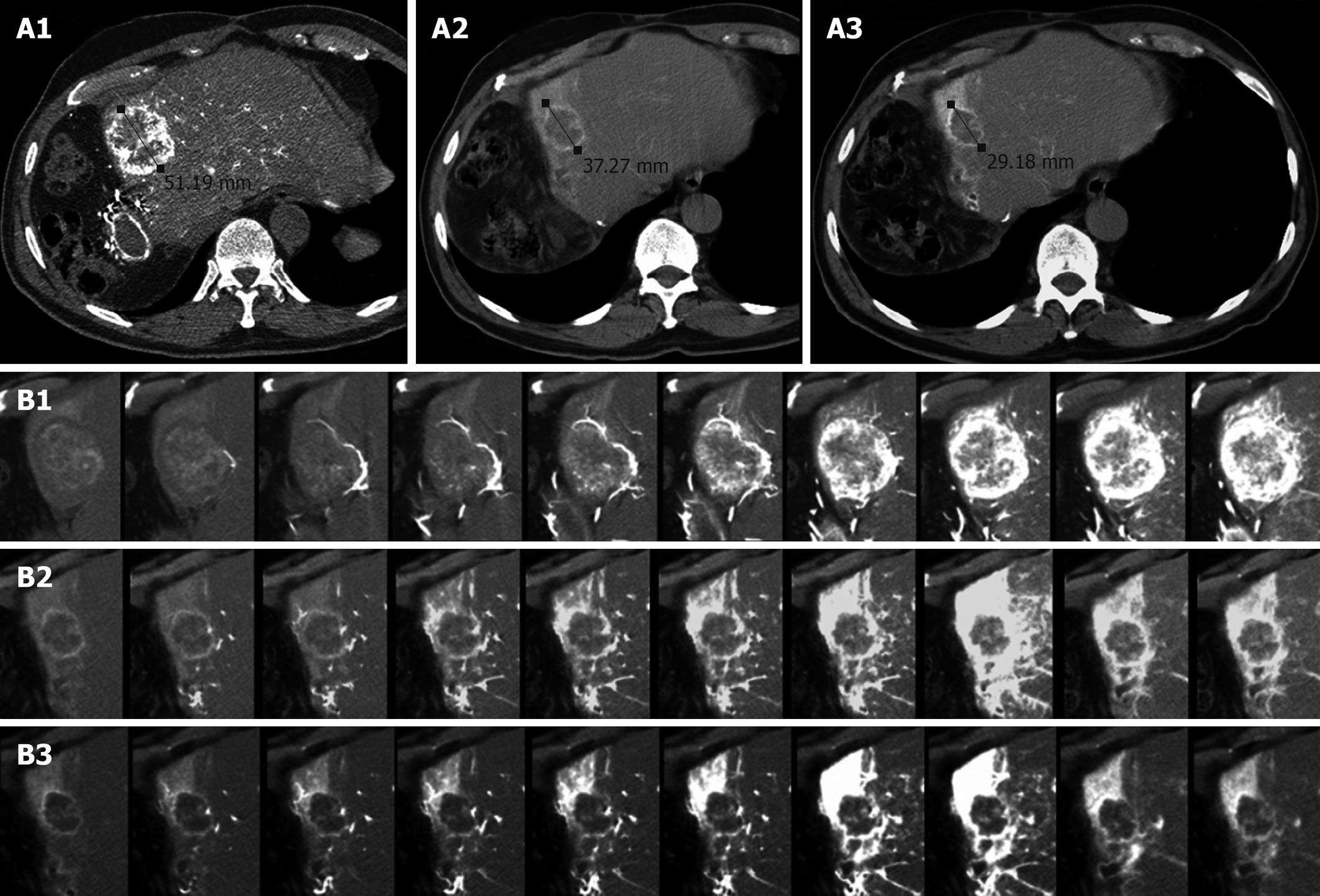
Figure 2 Computed tomography (CT) of liver metastasis.
A: CT arteriography at baseline (A1), after 2 cycles (A2) and after 6 cycles (A3) of HAI. The metastasis was hypervascular at baseline. It became shorter after 2 cycles but remained as a stable disease according to RECIST. After 6 cycles, a partial response was observed (43% reduction in diameter); B: Dynamic contrast-enhanced CT (DCE-CT) scan at baseline (B1), after 2 cycles (B2) and after 6 cycles (B3). At baseline, the tumor was progressively and massively enhanced. After 2 cycles, there was a dramatic decrease in tumor perfusion, strongly suggesting the efficacy of HAI. Normal hepatic segment 4 is strongly enhanced. After 6 cycles, only small enhanced areas are visible within the residual tumor.
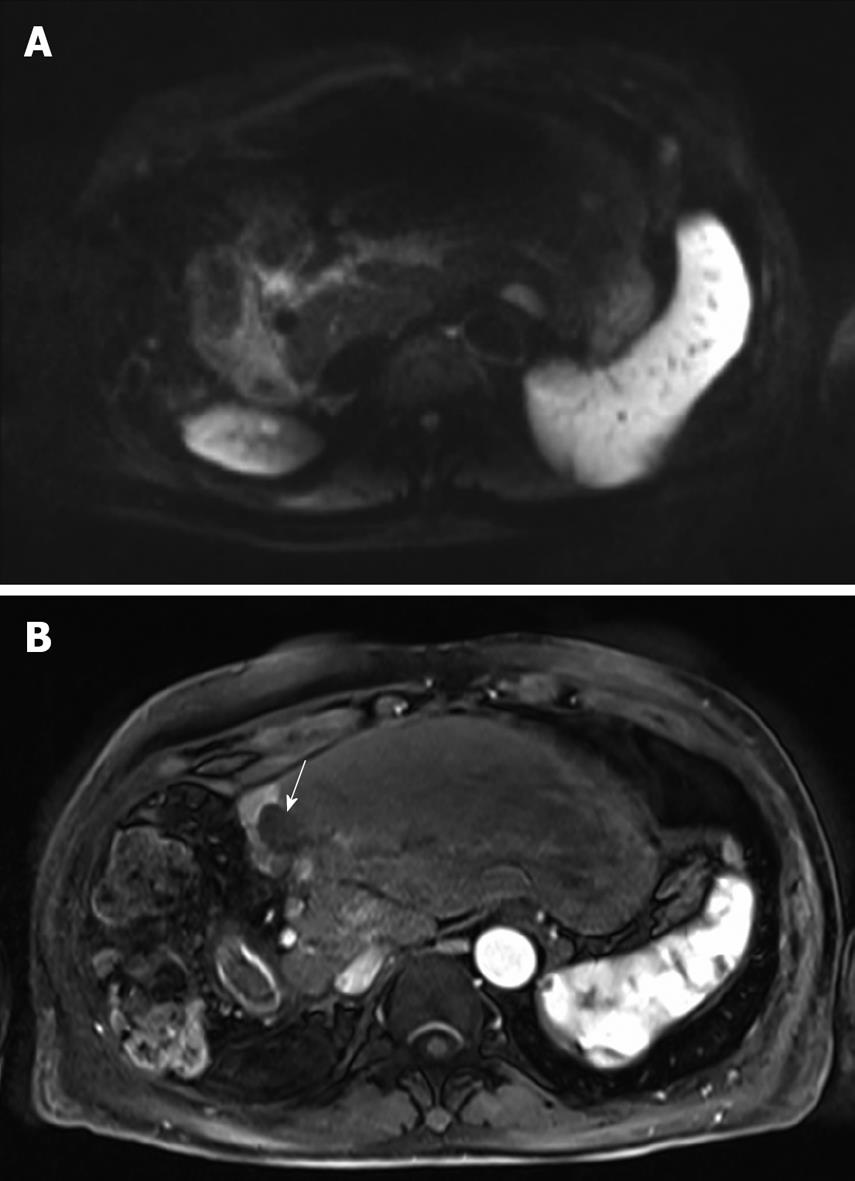
Figure 3 MRI of the liver after 8 cycles of HAI.
A: The lesion is isointense to the liver parenchyma on the diffusion-weighted image thereby suggesting the absence of viable tumor; B: The lesion is completely avascular (arrow) during the arterial phase after injection of gadolinium chelate. Note the enhancement of the remnant segment 4.
- Citation: Guiu B, Vincent J, Guiu S, Ladoire S, Ortega-Deballon P, Cercueil JP, Chauffert B, Ghiringhelli F. Hepatic arterial infusion of gemcitabine-oxaliplatin in a large metastasis from colon cancer. World J Gastroenterol 2010; 16(9): 1150-1154
- URL: https://www.wjgnet.com/1007-9327/full/v16/i9/1150.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i9.1150