Copyright
©2010 Baishideng Publishing Group Co.
World J Gastroenterol. Nov 21, 2010; 16(43): 5440-5446
Published online Nov 21, 2010. doi: 10.3748/wjg.v16.i43.5440
Published online Nov 21, 2010. doi: 10.3748/wjg.v16.i43.5440
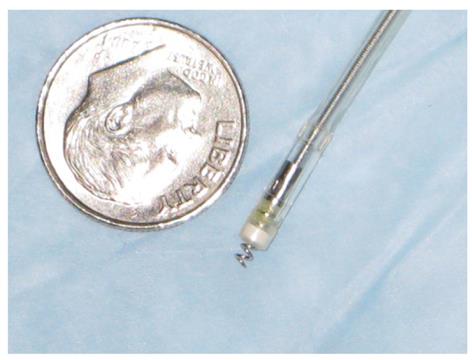
Figure 1 Stimulating electrodes.
Two electrodes (Medtronic CapSureFix Model 5076) were used in this study. This model had an electrically active helix that was designed to extend easily (up to 2 mm) for active fixation and retraction. The electrodes were positioned at 15 cm and 12 cm above the anal verge.
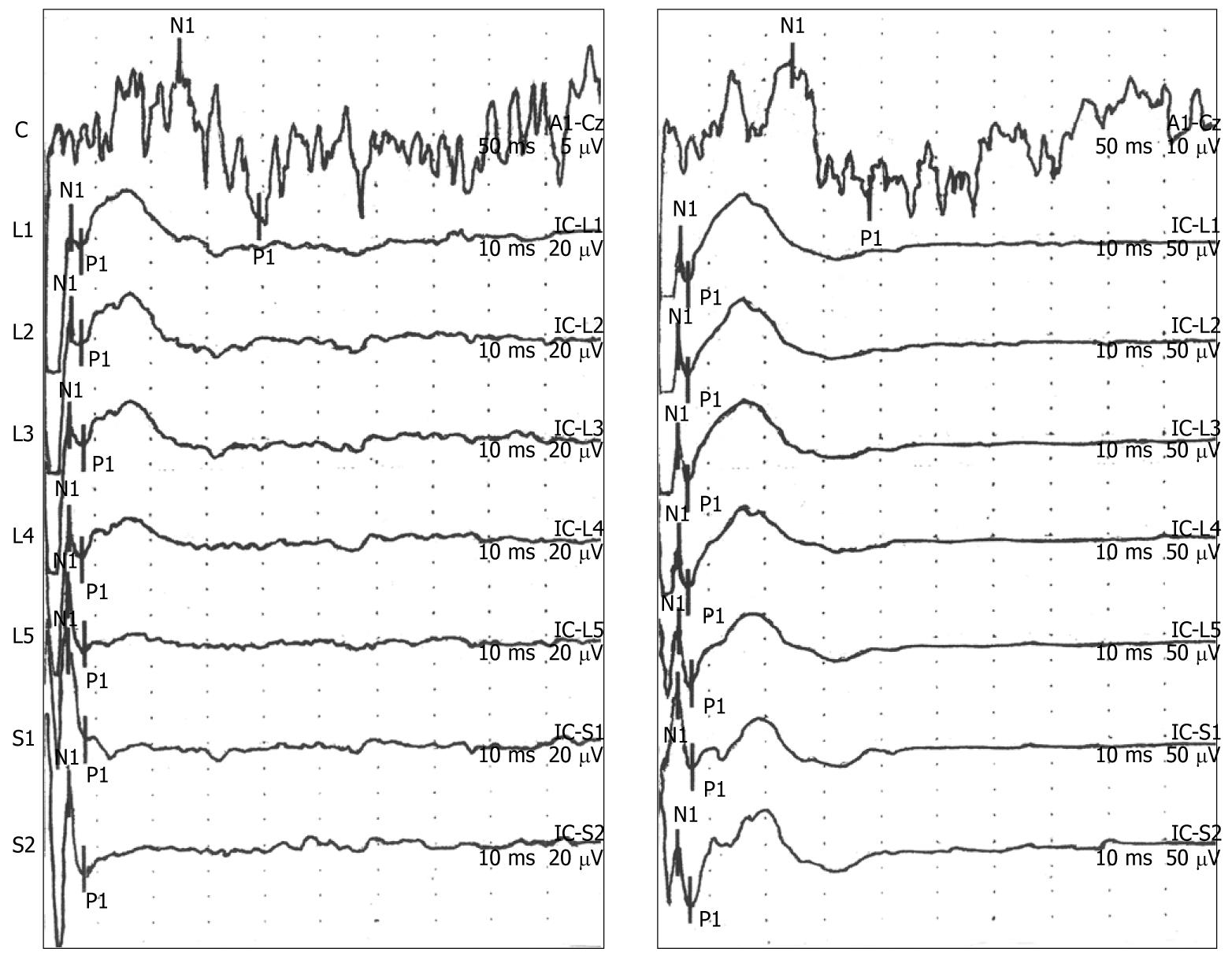
Figure 2 Representative cortical and spinal evoked potential responses to electrical stimulation in the rectum.
Evoked potential (EP) responses demonstrated that the typical morphology for cortical and spinal EP recordings including an N1/P1 wave form that increased with stimulus intensity (threshold intensity, left panel; 2 × threshold intensity, right panel). Note the different scales for measuring the amplitude of EP response in the left panel (cortical, 5 μV/division; spinal, 20 μV/division) and right panel (cortical, 10 μV/division; spinal, 50 μV/division). Summary latency and amplitude results for recordings obtained using an electrical stimulus 1.5 × threshold is presented in Table 2.
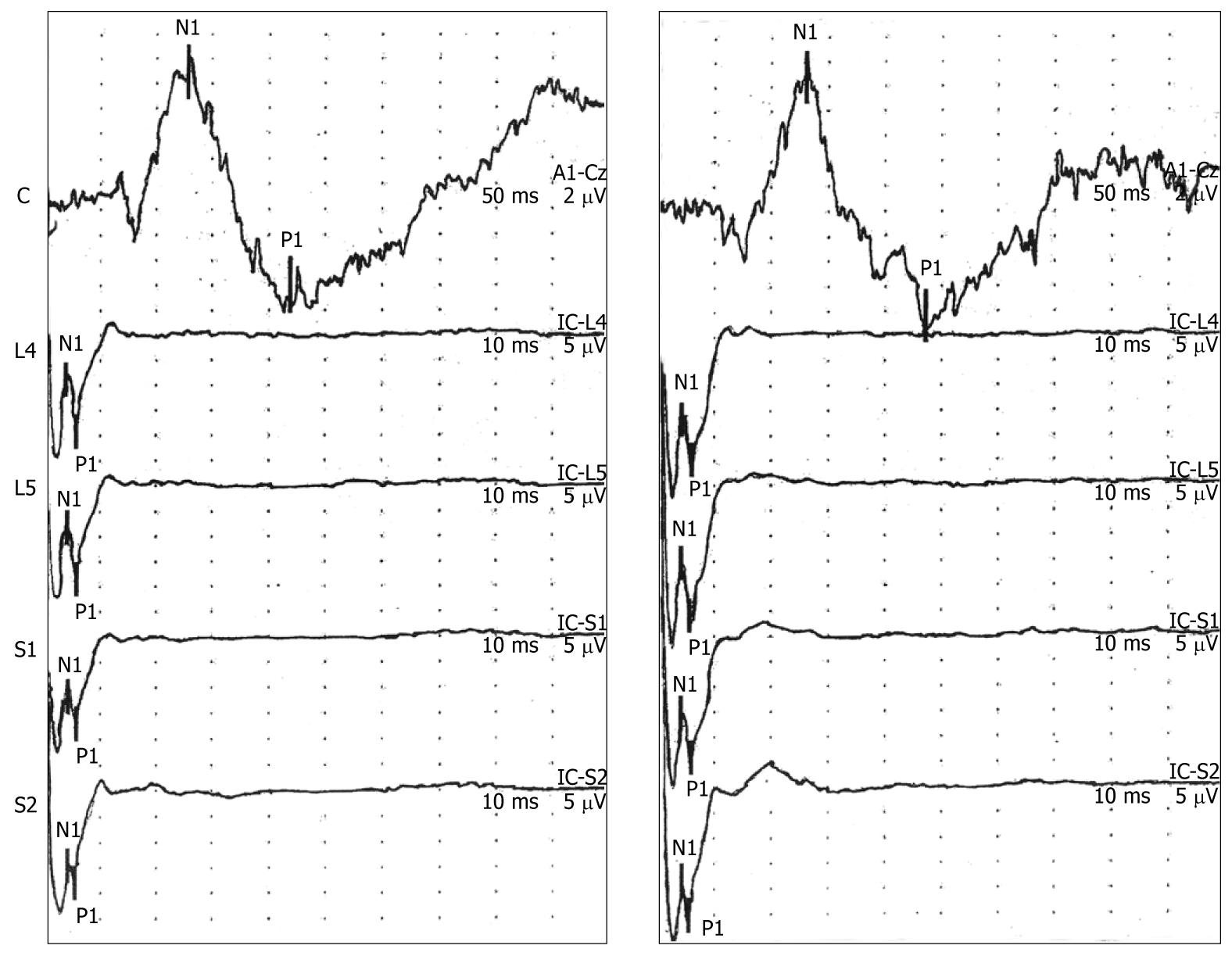
Figure 3 Evoked potential responses were reproducible over time.
Representative cortical and spinal evoked potential responses from two recording sessions for one volunteer are shown in this figure. No significant changes in the latency and amplitude values were observed compared to the initial recording session. Summary data are presented in Table 3.
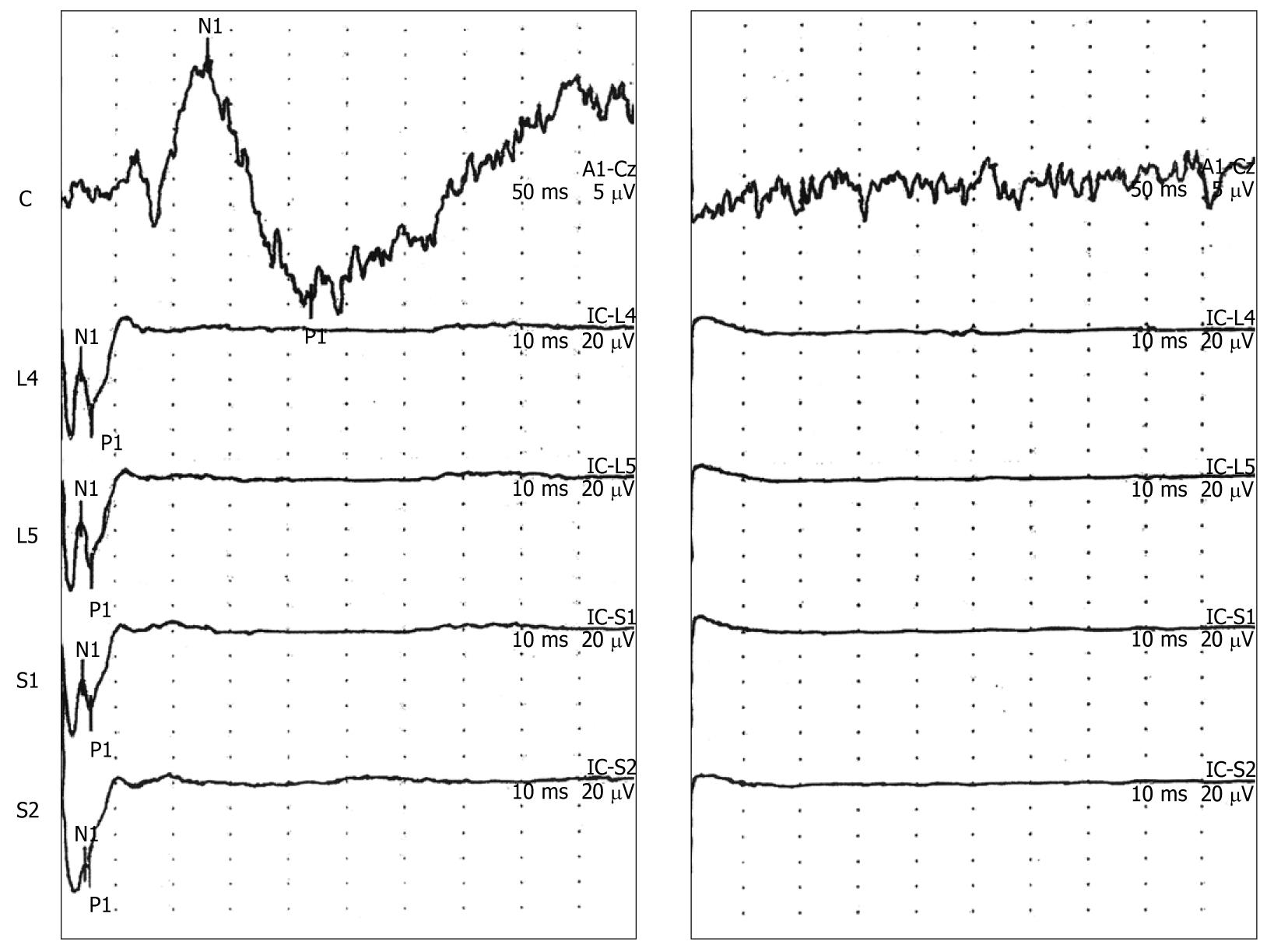
Figure 4 Application of Lidocaine jelly to the rectal mucosa at the sites of electrical stimulation resulted in loss of the cortical and spinal evoked potential responses.
A representative evoked potential response (before and after application of Lidocaine) is presented in this figure. In addition, all participants reported a loss in the sensory response to electrical stimulation after application of Lidocaine.
- Citation: Garvin B, Lovely L, Tsodikov A, Minecan D, Hong S, Wiley JW. Cortical and spinal evoked potential response to electrical stimulation in human rectum. World J Gastroenterol 2010; 16(43): 5440-5446
- URL: https://www.wjgnet.com/1007-9327/full/v16/i43/5440.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i43.5440