Copyright
©2010 Baishideng.
World J Gastroenterol. May 7, 2010; 16(17): 2094-2099
Published online May 7, 2010. doi: 10.3748/wjg.v16.i17.2094
Published online May 7, 2010. doi: 10.3748/wjg.v16.i17.2094
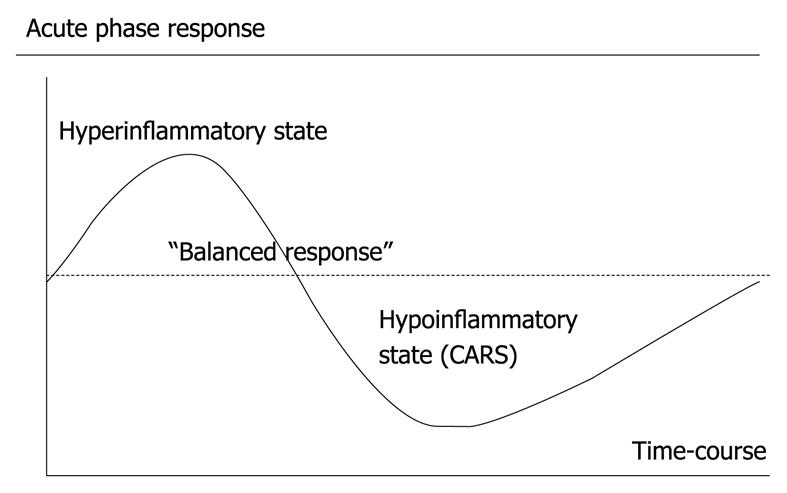
Figure 1 The acute phase response as seen in critical illness, e.
g. severe acute pancreatitis.
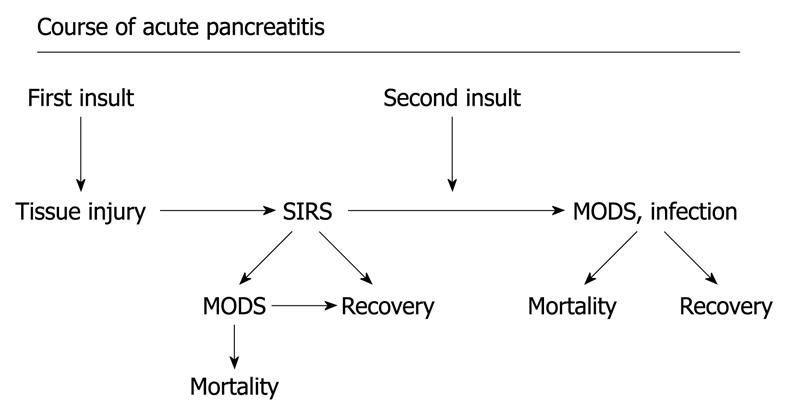
Figure 2 Course of acute pancreatitis.
A potential development in severe acute pancreatitis with the first “insult” resulting in a pronounce systemic inflammatory response and potential development of organ dysfunction, and in the worst scenario early mortality. Later during the course, combination of organ dysfunction and infection, potentially pronounced after the second “insult” (translocation from the gut, burst of proinflammatory cytokines, surgery, etc.) may result in late mortality. MODS: Multiple organ dysfunction syndrome.
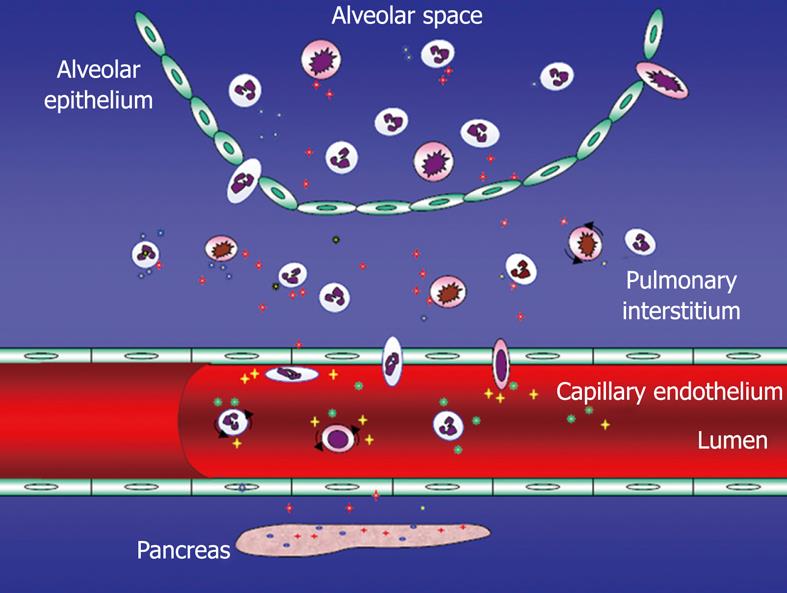
Figure 3 Acute pancreatitis-associated acute lung injury (ALI) - potential mechanisms including endothelial barrier dysfunction.
Several adhesion molecules [selectins, intercellular adhesion molecule-1 (ICAM-1), platelet endothelial cell adhesion molecule-1 (PECAM-1) among others] involved in the extravasation of not at least polymorphonuclear neutrophils (PMNs). Tissue injury by not at least these PMNs.
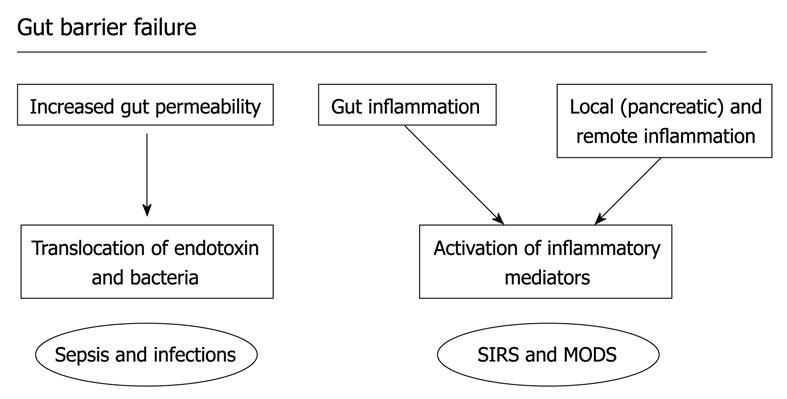
Figure 4 Gut barrier failure.
The increase in permeability of the gut barrier from the intestinal lumen may allow translocation of endotoxin and bacteria and there is also activation of immunocompetent cells in the gut wall and gut associated lymphoid tissue, contributing to the inflammatory response, infection, and potentially the development of organ dysfunction.
- Citation: Zhou MT, Chen CS, Chen BC, Zhang QY, Andersson R. Acute lung injury and ARDS in acute pancreatitis: Mechanisms and potential intervention. World J Gastroenterol 2010; 16(17): 2094-2099
- URL: https://www.wjgnet.com/1007-9327/full/v16/i17/2094.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i17.2094