Copyright
©2009 The WJG Press and Baishideng.
World J Gastroenterol. May 28, 2009; 15(20): 2433-2440
Published online May 28, 2009. doi: 10.3748/wjg.15.2433
Published online May 28, 2009. doi: 10.3748/wjg.15.2433
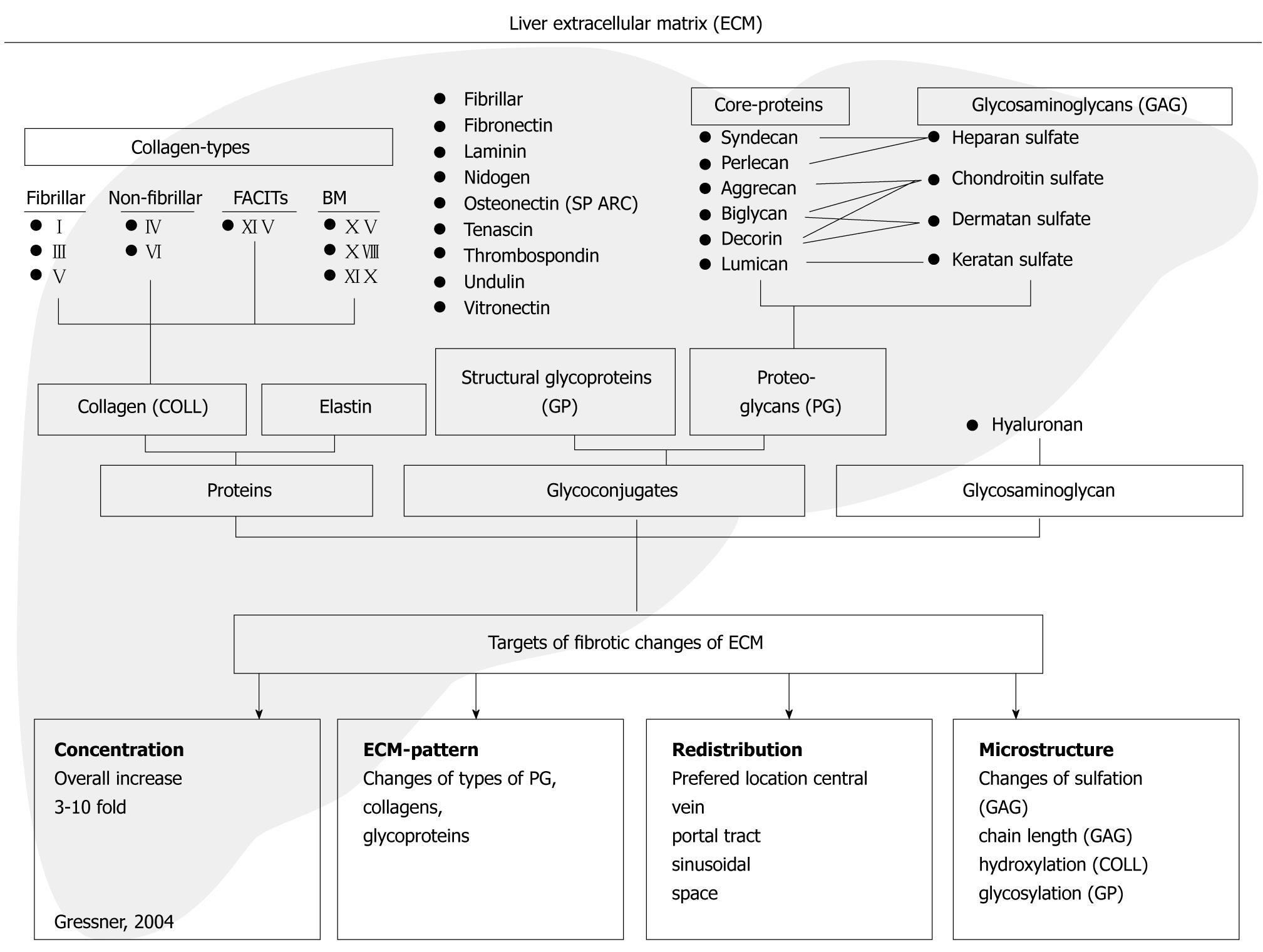
Figure 1 Components of the extracellular matrix (connective tissue) of the fibrotic liver and their major changes.
The binding of glycosaminoglycans (GAG) to the respective core proteins (CP) of proteoglycans (PG) are shown. BM: Basement membranes; FACIT: Fibril-associated collagens with interrupted triple-helices.
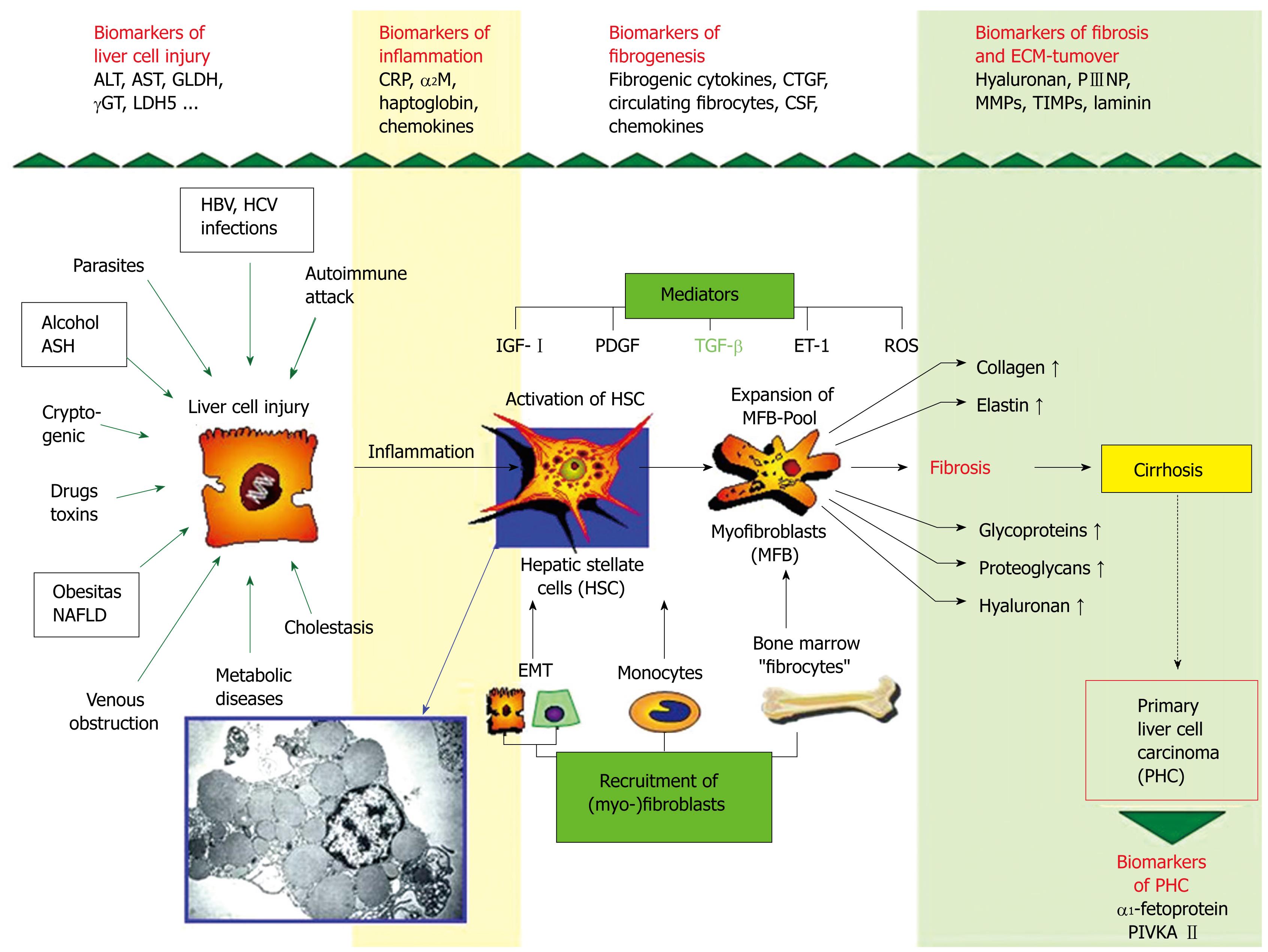
Figure 2 Synopsis of pathogenetic mechanisms of liver fibrosis (fibrogenesis).
The cells produce an increase in extracellular matrix derived from activated hepatic stellate cells (HSC)/expended pool of myofibroblasts (MFB) produce various components of the extracellular matrix (fibrosis) leading to cirrhosis. Newly recognized pathogenetic mechanisms point to the (i) influx of bone marrow-derived cells (fibrocytes) to the liver, (ii) to circulating monocytes and to their TGF-β-driven differentiation to fibroblasts and (iii) to the epithelial-mesenchymal transition (EMT) of hepatocytes and bile duct epithelial cells to fibroblasts. All three complementary mechanisms enlarge the pool of matrix-synthesizing (myo-)fibroblasts. Some important fibrogenic mediators are transforming growth factor (TGF)-β, platelet-derived growth factor (PDGF), insulin-like growth factor I (IGF-I), endothelin-1 (ET-1), and reactive oxygen metabolites (ROS). Abbreviations: ASH: Alcoholic steatohepatitis; NAFLD: Non-alcoholic fatty liver disease. The insert shows an electron micrograph of hepatic stellate cells containing numerous lipid droplets.
- Citation: Gressner AM, Gao CF, Gressner OA. Non-invasive biomarkers for monitoring the fibrogenic process in liver: A short survey. World J Gastroenterol 2009; 15(20): 2433-2440
- URL: https://www.wjgnet.com/1007-9327/full/v15/i20/2433.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.2433