Copyright
©2009 The WJG Press and Baishideng.
World J Gastroenterol. Mar 14, 2009; 15(10): 1209-1218
Published online Mar 14, 2009. doi: 10.3748/wjg.15.1209
Published online Mar 14, 2009. doi: 10.3748/wjg.15.1209
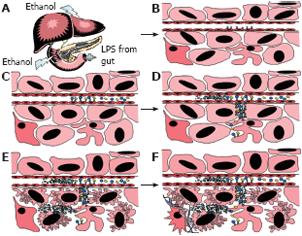
Figure 1 A proposed hypothesis of the two-hit model for the onset and/or progression of alcohol liver disease.
A: The prolonged consumption of ethanol has been associated with an increase in gut permeability. Lipopolysaccaride (LPS) may leak out of the gut and into the blood stream, finding its way back to the liver. B: Meanwhile, the breakdown of alcohol and fats in the liver could modify cellular proteins with malondialdehyde and/or acetaldehyde and result in increased levels of these modified proteins. Receptors on endothelial cells (SECs) specific for LPS and aldehyde modified proteins might also be up-regulated. C: The various scavenger receptors bind LPS and/or aldehyde modified proteins circulating in the blood stream. D: Binding of these molecules causes an increased release of pro-inflammatory cytokines, which are dumped into the blood stream and into the liver through the Space of Disse. The release into the liver causes activation of kupffer cells, binding of LPS and modified proteins, and their release of more pro-inflammatory cytokines. E: The cytokine release from SECs and/or kupffer cells signals immune cells infiltrate into the liver and result in damage to the hepatocytes. F: Damage to the hepatocytes increases the amount of TGF-β and other cytokines, causing the stellate cells and SECs to secrete pro-fibrogenic factors. These factors help to rebuild and remodel the liver parenchyma initiating the wound healing responses. Following repair of the liver, there is scaring and some irreparable damage, which can get better if the insults (LPS and modified proteins) are taken away. However, if alcohol consumption remains there becomes a point whenentence, preferably as two shorter sentences, to clarify this?
- Citation: Schaffert CS, Duryee MJ, Hunter CD, 3rd BCH, DeVeney AL, Huerter MM, Klassen LW, Thiele GM. Alcohol metabolites and lipopolysaccharide: Roles in the development and/or progression of alcoholic liver disease. World J Gastroenterol 2009; 15(10): 1209-1218
- URL: https://www.wjgnet.com/1007-9327/full/v15/i10/1209.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.1209