Copyright
©2007 Baishideng Publishing Group Co.
World J Gastroenterol. Mar 14, 2007; 13(10): 1505-1515
Published online Mar 14, 2007. doi: 10.3748/wjg.v13.i10.1505
Published online Mar 14, 2007. doi: 10.3748/wjg.v13.i10.1505
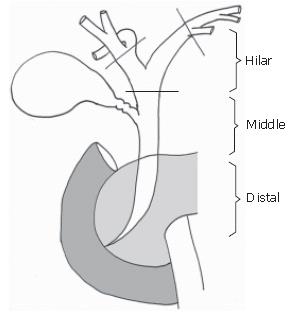
Figure 1 Schema of extrahepatic bile duct.
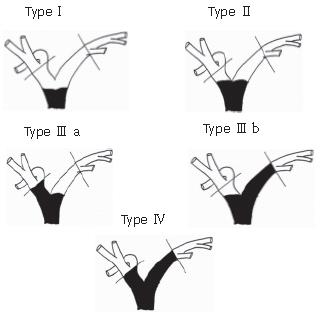
Figure 2 Bismuth-Corlette classification of hilar bile duct cancer[9].
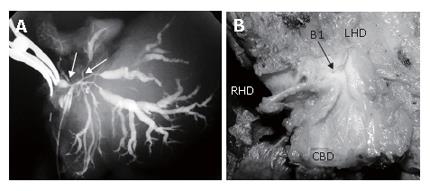
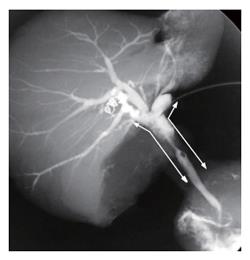
Figure 3 Tumor infiltration of the roots of the caudate branches; A: Cholangiography of a resected specimen.
Hilar bile duct cancer has infiltrated the root of the caudate branches (B1) arising from the confluence of the hepatic duct (arrows); B: Gross appearance of the resected tumor. The caudate branch opens into the hilar neoplasm.
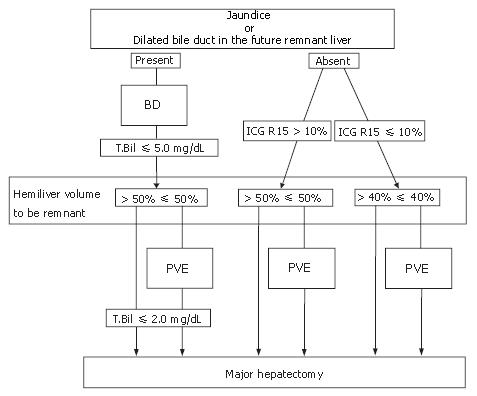
Figure 4 Flowchart of preoperative treatment.
If a patient had jaundice or there were dilated bile ducts in the future remnant liver, biliary drainage (BD) was performed. Surgical interventions were scheduled after sufficient recovery of hepatic function. Portal vein embolization (PVE) was carried out to avoid postoperative liver failure, depending on the liver function and the liver volume to be resected.
Figure 5 Intraoperative view at laparotomy after biliary drainage and portal vein embolization.
A percutaneous transhepatic biliary drainage tube (arrow) has been inserted into the bile duct of segment 3. The right liver is markedly atrophic, and there is a clear line of demarcation between the right and left liver.
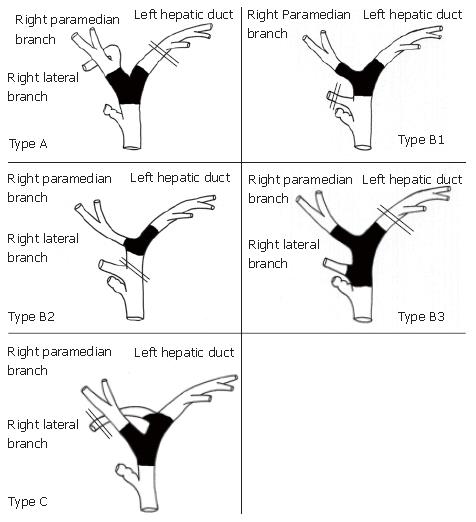
Figure 6 Indications for left trisectoriectomy according to tumor location and the bile duct variations in the anatomy of the right lateral branch of the bile duct.
Double lines indicate the scheduled cut end of the bile duct. Type A, ordinary bifurcation; extended right hepatectomy is the choice of treatment. Type B, the right lateral branch originates from the common hepatic duct; left trisectoriectomy, preserving the right lateral branch, is a useful alternative in Types B1 and B2. Type C, the right lateral branch originates from the left hepatic duct; left trisectoriectomy may provide a longer bile duct margin.
Figure 7 Cholangiography of the resected specimen by HPD.
The tumor is located in the common hepatic duct (Bismuth-Corllete type 2), and microscopic examination showed superficial spread to the right and left hepatic duct and the intrapancreatic part of the common bile duct (arrows).
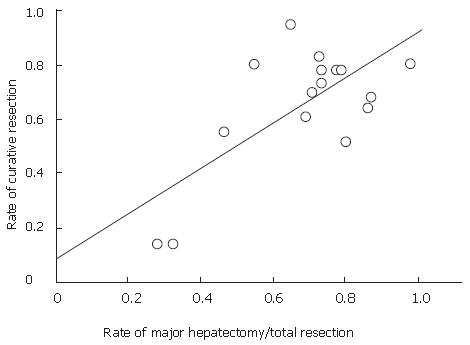
Figure 8 Graph of data from a literature review of the relationship between curative resection and major hepatectomy rate.
The studies are listed shown in Table 1. Curative resection is defined as a microscopic ally negative margin. Linear approximation showed a significant correlation between the rate of major hepatectomy and curative resection (P = 0.0027, R = 0.7).
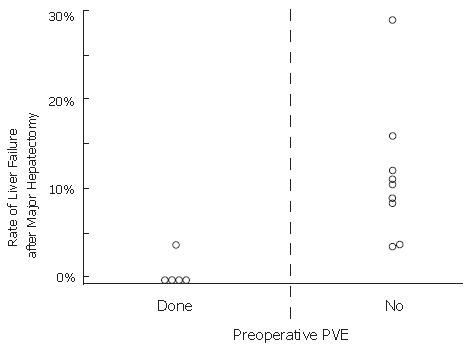
Figure 9 Graph of data from a literature review of the relationship between the preoperative portal vein embolization (PVE) and the rate of postoperative liver failure after major hepatectomy for hilar bile duct cancer.
PVE significantly reduced the incidence of postoperative liver failure (P = 0.0113).
- Citation: Seyama Y, Makuuchi M. Current surgical treatment for bile duct cancer. World J Gastroenterol 2007; 13(10): 1505-1515
- URL: https://www.wjgnet.com/1007-9327/full/v13/i10/1505.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i10.1505