Published online Sep 6, 2018. doi: 10.12998/wjcc.v6.i9.279
Peer-review started: April 3, 2018
First decision: May 21, 2018
Revised: May 26, 2018
Accepted: June 7, 2018
Article in press: June 8, 2018
Published online: September 6, 2018
Processing time: 157 Days and 10.8 Hours
Carpal tunnel syndrome (CTS) is well recognized as the most common type of peripheral neuropathy. A rare cause of CTS is tophaceous gout. Tophi deposits can accumulate in various structures including the flexor tendons, tendon sheaths, the carpal tunnel floor, transverse carpal ligament, and even the median nerve, causing various symptoms such as pain, numbness, and weakness. Tophi forming in the carpal canal can compress the median nerve, leading to CTS. Here, we describe a 25-year-old male with a family history of tophaceous gout who presented with typical CTS symptoms. Although he had chronic numbness in his right hand, he failed to present with any obvious palpable masses on his forearm or hand. However, his family history, laboratory, clinical, and magnetic resonance imaging findings were consistent with tophi deposits. CTS symptoms were eased through surgical removal of tophi and decompression of the median nerve. No recurrences of gout and CTS symptoms were reported at a one-year follow-up. This case shows that CTS symptoms could be the initial manifestation of tophaceous gout. In patients with a family history of gout and with CTS symptoms, imaging examinations are critical for early diagnosis and selecting appropriate treatment. Surgical removal of “covert” tophi and decompression of the median nerve is an effective option for eliminating symptoms.
Core tip: A rare cause of carpal tunnel syndrome (CTS) is tophaceous gout. This report represents the first case, to our knowledge, of a patient presenting with typical CTS symptoms, yet lacking any visible or palpable signs of gout in any part of his body. Only after magnetic resonance imaging, surgical inspection, and pathological analysis was it clear that the 25-year-old patient had a large gouty tophus attached to the surface of the distal volar radius adjacent to the digital flexor tendons. Surgical removal of the “covert” tophi and decompression of the median nerve is an effective option for eliminating CTS symptoms.
- Citation: Luo PB, Zhang CQ. Chronic carpal tunnel syndrome caused by covert tophaceous gout: A case report. World J Clin Cases 2018; 6(9): 279-283
- URL: https://www.wjgnet.com/2307-8960/full/v6/i9/279.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i9.279
Carpal tunnel syndrome (CTS) is the most commonly diagnosed compression neuropathy of the upper limb[1]. It is usually caused by excessive pressure on the median nerve as it travels through the wrist at the carpal tunnel. The confined anatomic space makes the nerve vulnerable to compression. The causes of CTS include local trauma to the wrist, bleeding disorders, space-occupying lesions, rheumatoid arthritis, diabetes mellitus, and multiple myeloma[1-3]. Deposition of gouty tophi in flexor tendons can also cause chronic and acute CTS. This is extremely rare, with a reported incidence of 0.6%[4]. For the patient of this case report presenting with CTS, it was particularly exceptional that he had no visible tophi in any part of the body. To our limited knowledge, the literature has yet to report tophi-associated chronic CTS in a patient who lacks visible signs of tophi but has a family medical history of gout. Here, we describe such a case of CTS without significantly visible tophi in a 25-year-old male.
A 25-year-old male who was referred to our department presented with typical CTS symptoms of his right hand. The symptoms worsened with extension of the wrist. Intermittent numbness in the three radial fingers of the right hand developed three years ago, but he did not recall a history of trauma or tophaceous gout. The patient reported no previous gouty attack. He did not accept medical treatment during the first two years. His condition worsened, and the numbness in his right hand became significantly aggravated over the previous three months before seeking treatment at our department.
Medical treatment with mecobalamin aimed to ease the numbness began three months ago, but without significant improvement. The patient had normal hand function activities but decreased grip strength. On local physical examinations, joint pain, palpable mass, and redness of the wrist and hand were absent. Obvious atrophy of the thenar muscle was also absent. Phalen’s test and Tinel’s sign were positive. Neurologic examination revealed numbness in the thumb, index finger, middle finger, and half of the ring finger of his right hand. Electromyography revealed reduced conduction velocity and impaired sensory function of the median nerve. Laboratory analyses, including complete blood count and electrolytes, were normal. C-reactive protein was elevated (17.17 mg/L), as was erythrocyte sedimentation rate (28 mm/h). A diagnosis of hyperuricemia was made with an elevated uric acid level of 568 µmol/L.
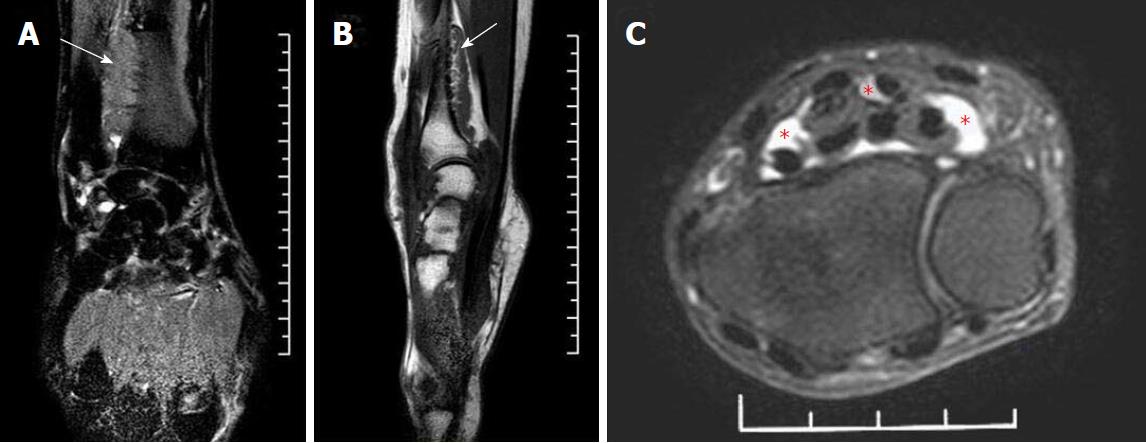
Radiographs revealed no bone erosion or tophi deposition in his hands (Figure 1). Magnetic resonance imaging (MRI) showed a sizable mass adhering to the surface of the distal volar radius with a wide base, and a mass adjacent to the digital flexor tendons at the level of the proximal carpal tunnel; this mass appeared to be pressing on the median nerve (Figure 2). The mass had low-to-intermediate signal intensity on T1-weighted images and high signal intensity on T2-weighted images. Given the gout history of the patient’s father, and the laboratory, clinical, and imaging findings, we speculated this was a case of tophaceous gout compressing the median nerve, resulting in numbness in the hand.
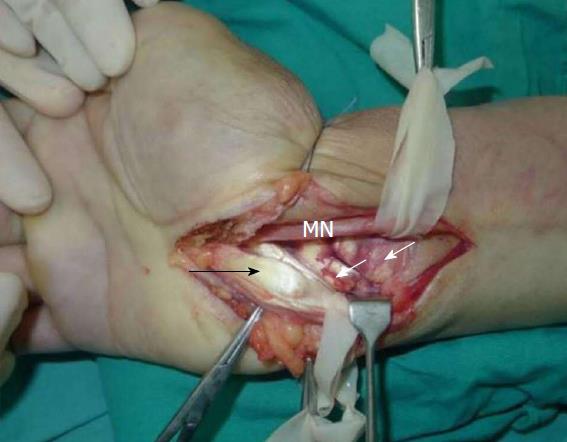
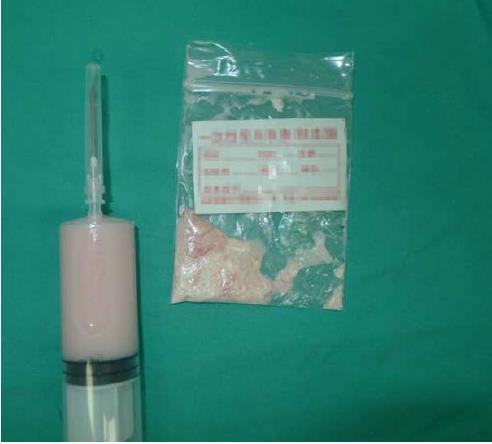
On the basis of imaging findings and the failure to ease numbness through mecobalamin therapy, we decided to perform surgery two days after hospital admission. During the operation, an upper arm tourniquet was applied (inflated to 200 mmHg) without exsanguinating the extremity. A longitudinal incision was made over the carpal tunnel, distal to the wrist flexion crease and proximal to the forearm. With the transverse carpal ligament exposed, the median nerve was identified. We observed a significant bulge in the portion of the median nerve within the canal and a distal impression on the nerve (Figure 3). Large tophi were observed next to the ulnar side of the median nerve, and in the flexor digitorum superficialis and flexor digitorum profundus tendon sheaths of the middle finger, ring finger, and digitus minimus (Figure 4). With the median nerve and flexor tendons protected by the drainage tubes, large gouty tophi were found embedded deep into the distal volar radius (Figure 4). The gouty tophi had irregular boundary shapes, and their surface was soft but without inflammation or ulceration. Thus, we performed a synovectomy of all the affected flexor tendons and we removed the deep gouty tophi (Figures 5 and 6). A definite diagnosis of tophaceous gout was confirmed by the pathology report. The wound was irrigated with saline until clear effluent was observed. Epineurium neurolysis of the median nerve was then performed. Rubber drainage tubes were removed one week later.
The day after surgery, the patient reported marked lessening of numbness in the thumb, index finger, middle finger, and half of the ring finger of his right hand. We then encouraged him to actively flex and extend his hand; uric acid-lowering medication was recommended. The patient was followed closely as an outpatient under orthopedic surgery services and rheumatology services. Long-term management of gout involved daily maintenance medication with allopurinol. With respect to diet, the patient was advised to decrease consumption of meat high in purine content, high fructose corn syrup, and alcohol, especially beer.
Six months after the surgery, the patient recovered full sensory and motor function of the right median nerve, and his uric acid level was normal. As of the 12-mo follow-up, the patient reported no gouty attacks and no recurrence of numbness. Gouty tophi in the operated hand were also absent at the 12-mo exam (Figure 7).
The carpal tunnel is a narrow rigid tube at the base of the hand composed of ligaments and bones. It encompasses the median nerve and the tendons that move the fingers. The confined anatomic space makes the nerve susceptible to compression. Tophaceous gout is a well recognized, but uncommon, cause of CTS. Tophi can be deposited in various structures, including the flexor tendons, tendon sheaths, the carpal tunnel floor, transverse carpal ligament, and even the median nerve[5]. These can cause symptoms associated with these deposits[5]. In the current case, several flexor digitorum superficialis and flexor digitorum profundus tendons were affected by tophi, and more deep tophi were found adhering to the distal volar radius. Interestingly, in this patient the pronator quadratus muscle was also affected, which had never been reported in the literature.
Carpal tunnel compression may be the initial manifestation of gout[6]. Because of its rare frequency, gouty involvement of the flexor tendons and CTS may be overlooked in the differential diagnosis[7]. It was particularly exceptional for this patient, because there were no visible tophi in any part of his body. Gout is more likely to develop in patients whose family members have had gout. It is possible that their genetic makeup predisposes them to gout[8]. Since our patient reported no problem with overconsumption of alcohol, no history of gout, and no visible tophi when he visited our department for local examinations, we diagnosed him as a typical CTS patient. He took mecobalamin but experienced little relief for months. Given the imaging findings and his father’s history of gout, gouty tophi were finally considered to be the likely cause of CTS.
Chen et al[9] performed a retrospective CT and MRI review of patients with a documented diagnosis of gout and who presented with gout-related CTS. This review revealed that gouty tophi should be entertained as a cause of CTS in the appropriate patient population. Ultrasound has also been used in diagnosing CTS caused by gouty tophi of the flexor tendons of the fingers[10]. It is well known that a delayed diagnosis can lead to irreversible nerve injury and complications, including articular changes, tendon rupture, and tenosynovitis[11]. Thus, it is imperative to consider all possibilities when entertaining causes of CTS.
In the present case, surgical intervention was postponed because of a lack of imaging data and our ignorance about his family history of gout. Thus, physicians need to be familiar with tophi-associated CTS and aware of the patient’s family history of gout, as both are critical for differential diagnosis. In addition, imaging examinations, including ultrasound, CT, and MRI are recommended for an early accurate diagnosis. Surgical intervention is recommended to relieve symptoms and to avoid permanent damage.
Poor healing of surgical wounds in gouty patients is well recognized because of the phlogistic characteristics of gout[12]. This did not pose a problem in our case. Complete removal of visible and well-confined tophi, lack of inflammatory lesions, satisfactory rinsing of the area and use of uric acid-lowering agents may explain why this was averted. The disease may recur due to residual tophi. Complete removal of the tophi achieved a good result in our patient. Uric acid-lowering medication, including uricosuric agents and allopurinol, is necessary to avoid recurrence of gout[13]. The target serum urate levels should be less than 6 mg/dL[14]. Reducing the consumption of meat rich in purine content, high fructose corn syrup, and alcohol also was helpful in our case, likely because poor compliance with low-purine diet therapy and consumption of seafood and beer increases the risk of gout[7].
In conclusion, prompt diagnosis accompanied by CT or MRI is necessary to identify the specific causes of CTS in patients with a family history of gout and medication failure. To relieve symptoms and to avoid permanent damage, surgical decompression of the median nerve and complete removal of gouty tophi are recommended whenever a patient presents with symptomatic median nerve compression. Postoperatively, uric acid-lowering therapy should be instituted.
A young man with a family history of tophaceous gout who presented with typical carpal tunnel syndrome symptoms.
Numbness in the thumb, index finger, middle finger, and half of the ring finger of the right hand. The symptoms worsened with extension of the wrist. Normal hand function activities with decreased grip strength.
Tophaceous gout.
Complete blood count and electrolytes were normal. C-reactive protein, erythrocyte sedimentation rate and uric acid level were elevated.
Radiographs showed no bone erosion or tophi deposition in the hands. Magnetic resonance imaging showed a sizable mass adhering to the surface of the distal volar radius, and a mass adjacent to the digital flexor tendons at the level of the proximal carpal tunnel.
Tophaceous gout in the digital flexor tendons.
Surgical removal of the gouty tophi, synovectomy of all the affected flexor tendons, and decompression of the median nerve were performed.
To our limited knowledge, this is the first case report to describe tophi-associated chronic carpal tunnel syndrome without visible signs of tophi but has a family medical history of gout.
Carpal tunnel syndrome is the most commonly diagnosed compression neuropathy of the upper limb, which is usually caused by excessive pressure on the median nerve by many causes. Deposition of gouty tophi in flexor tendons is a rare cause.
Tophaceous gout is a rare cause of carpal tunnel syndrome (CTS). Physicians need to be familiar with tophi-associated CTS and aware of the patient’s family history of gout. Prompt imaging examinations including computed tomography or magnetic resonance imaging are necessary to identify the specific causes of CTS.
CARE Checklist (2013) statement: The authors have read the CARE Checklist (2013), and the manuscript was prepared and revised according to the CARE Checklist.
Manuscript Source: Unsolicited Manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Alimehmeti RH, Itrat M, Jiang B, Shen J S- Editor: Wang JL L- Editor: A E- Editor: Tan WW
| 1. | Levin RA, Felsenthal G. Handcuff neuropathy: two unusual cases. Arch Phys Med Rehabil. 1984;65:41-43. [PubMed] |
| 2. | Rayan GM, Conner S. Posterior interosseous nerve paralysis and amyloid neuropathy of multiple myeloma. Clin Orthop Relat Res. 1982;202-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 3. | Schnetzler KA. Acute carpal tunnel syndrome. J Am Acad Orthop Surg. 2008;16:276-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Rich JT, Bush DC, Lincoski CJ, Harrington TM. Carpal tunnel syndrome due to tophaceous gout. Orthopedics. 2004;27:862-863. [PubMed] |
| 5. | Chuang HL, Wong CW. Carpal tunnel syndrome induced by tophaceous deposits on the median nerve: case report. Neurosurgery. 1994;34:919; discussion 920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Ogilvie C, Kay NR. Fulminating carpal tunnel syndrome due to gout. J Hand Surg Br. 1988;13:42-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Lu H, Chen Q, Shen H. A repeated carpal tunnel syndrome due to tophaceous gout in flexor tendon: A case report. Medicine (Baltimore). 2017;96:e6245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Bardin T, Richette P. [The epidemiology and genetic of gout]. Presse Med. 2011;40:830-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Chen CK, Chung CB, Yeh L, Pan HB, Yang CF, Lai PH, Liang HL, Resnick D. Carpal tunnel syndrome caused by tophaceous gout: CT and MR imaging features in 20 patients. AJR Am J Roentgenol. 2000;175:655-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 65] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Therimadasamy A, Peng YP, Putti TC, Wilder-Smith EP. Carpal tunnel syndrome caused by gouty tophus of the flexor tendons of the fingers: sonographic features. J Clin Ultrasound. 2011;39:463-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Yü TF, Gutman AB. Principles of current management of primary gout. Am J Med Sci. 1967;254:893-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 25] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Tsai CY, Yu CL, Tsai ST. Bilateral carpal tunnel syndrome secondary to tophaceous compression of the median nerves. Scand J Rheumatol. 1996;25:107-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Gutman AB. Uricosuric drugs, with special reference to probenecid and sulfinpyrazone. Adv Pharmacol. 1966;4:91-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 71] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Khanna D, Fitzgerald JD, Khanna PP, Bae S, Singh MK, Neogi T, Pillinger MH, Merill J, Lee S, Prakash S. 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res (Hoboken). 2012;64:1431-1446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1168] [Cited by in RCA: 1108] [Article Influence: 85.2] [Reference Citation Analysis (1)] |