Copyright
©The Author(s) 2022.
World J Clin Cases. Aug 6, 2022; 10(22): 7808-7824
Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.7808
Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.7808
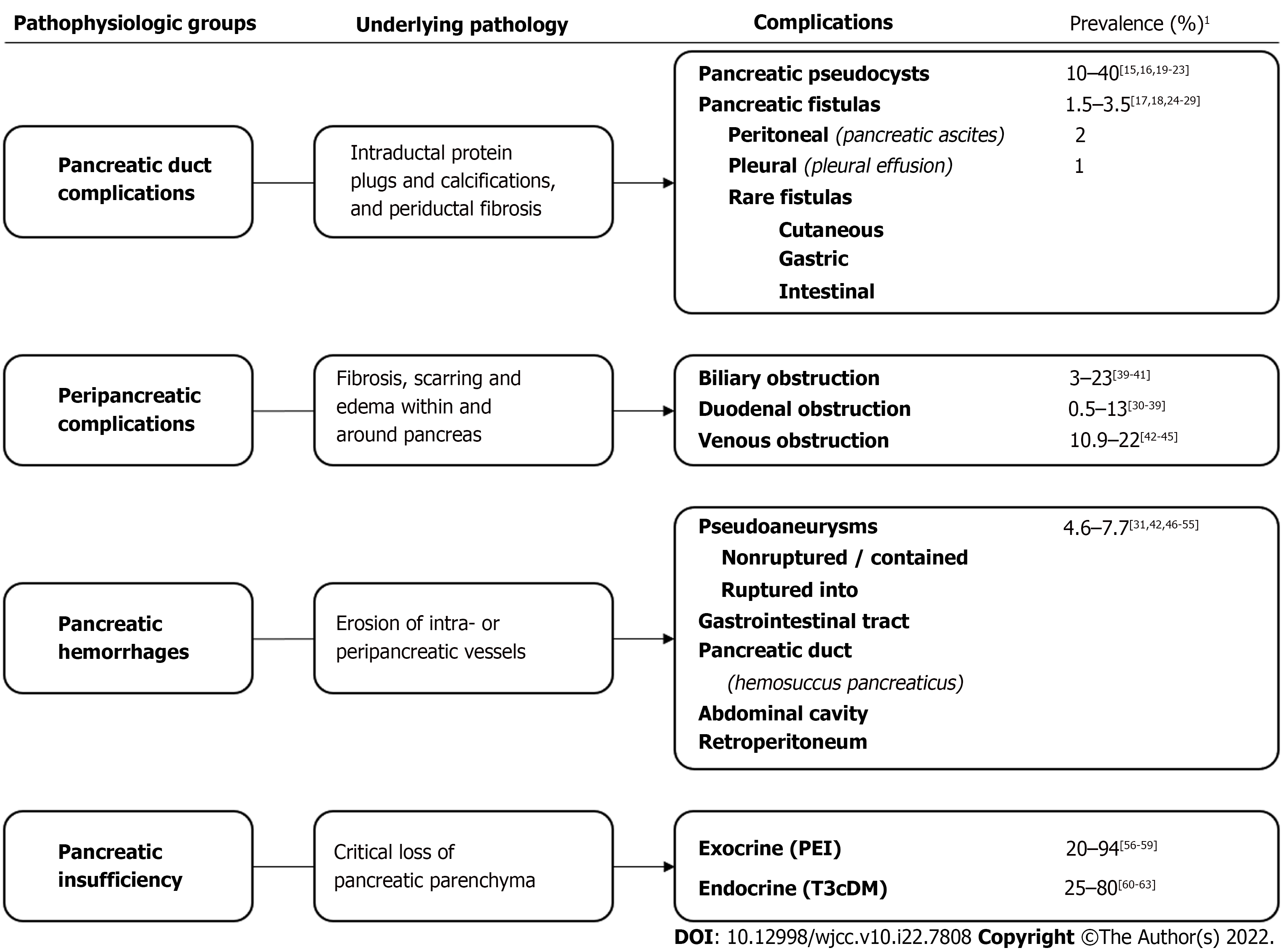
Figure 1 Pathophysiological classification of complications of chronic pancreatitis.
1References to the rates of prevalence. PEI: Pancreatic exocrine insufficiency; T3cDM: Type 3c diabetes mellitus.
Figure 2 Main complications of chronic pancreatitis.
(1) Pancreatic duct complications: 1-A: Pancreatic pseudocyst; 1-B: Pancreatic ascites; 1-C: Pancreatic pleural effusion; (2) Peripancreatic complications: 2-A: Common bile duct stenosis; 2-B: Duodenal stenosis; 2-C: Venous thrombosis (splenic vein); 2-D: Left-side portal hypertension due to splenic vein thrombosis; (3) Pancreatic hemorrhages: 3-A: Peripancreatic pseudoaneurysm; 3-B: Ruptured pseudoaneurysm (into pancreatic duct–hemosuccus pancreaticus); and (4) Pancreatic exocrine and endocrine insufficiency due to extensive loss of functional pancreatic parenchyma (acinar atrophy, fibrosis, inflammatory infiltrates).
Figure 3
Kaplan-Meier curves of complication-free survival of pathophysiologically grouped complications prior to, and following surgical management of chronic pancreatitis in a cohort of 166 patients.
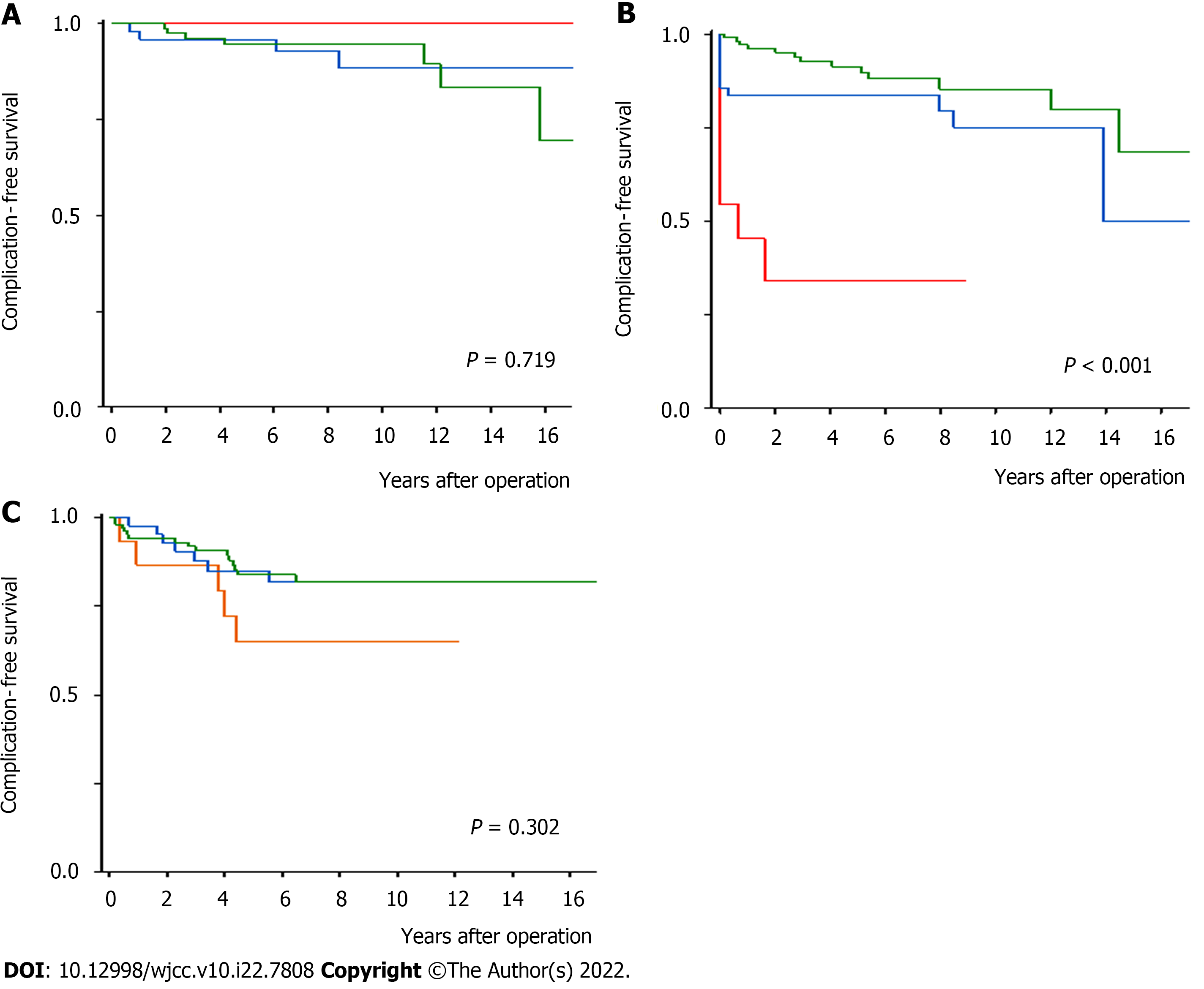
Figure 4 Kaplan-Meier curves of complication-free survival characterizing the impact of the type of surgery on occurrence of the new complications of chronic pancreatitis.
The log-rank test was used to assess differences between the curves. A: Peripancreatic complications (Whipple’s pancreatoduodenal resection–red line, other pancreatic resections–blue line, pancreatic drainage operations–green line); B: Pancreatic exocrine insufficiency (Whipple’s pancreatoduodenal resection–red line, other pancreatic resections–blue line, pancreatic drainage operations–green line); C: Pancreatic endocrine insufficiency (pancreatic distal resection–orange line, other pancreatic resections–blue line, pancreatic drainage operations–green line).
- Citation: Murruste M, Kirsimägi Ü, Kase K, Veršinina T, Talving P, Lepner U. Complications of chronic pancreatitis prior to and following surgical treatment: A proposal for classification. World J Clin Cases 2022; 10(22): 7808-7824
- URL: https://www.wjgnet.com/2307-8960/full/v10/i22/7808.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i22.7808