Published online May 18, 2017. doi: 10.5312/wjo.v8.i5.431
Peer-review started: November 10, 2016
First decision: February 15, 2017
Revised: March 4, 2017
Accepted: March 16, 2017
Article in press: March 17, 2017
Published online: May 18, 2017
Processing time: 186 Days and 11.8 Hours
To review and study the effect of lengthening along the anatomical axis of long bones and its relation to the mechanical axis deviation.
We try in this review to calculate and discuss the exact clinical impact of lengthening along the anatomical axis of the femur on affecting the limb alignment. Also we used a trigonometric formula to predict the change of the femoral distal anatomical mechanical angle (AMA) after lengthening along the anatomical axis.
Lengthening along the anatomical axis of the femur by 10% of its original length results in reduction in the distal femoral AMA by 0.57 degrees. There is no objective experimental scientific data to prove that the Mechanical axis is passing via the center of the hip to the center of the knee. There is wide variation in normal anatomical axis for different populations. In deformity correction, surgeons try to reproduce the normal usual bone shape to regain normal function, which is mainly anatomical axis.
Lengthening of the femur along its anatomical axis results in mild reduction of the distal femoral AMA. This may partially compensate for the expected mechanical axis lateralisation and hence justify its minimal clinical impact.
Core tip: In deformity correction the aim is to reproduce the normal anatomical shape of the bone to regain normal function. There is no experimental data to prove the passage of the imaginary mechanical axis and load distribution of the body via the center of the hip to the center of the knee. Lengthening along anatomical axis of the bone is expected to cause minimal or no clinical effect on mechanical axis and load distribution on joints.
- Citation: Emara KM, Mahmoud AN, Emara AK, Emara MK. Effect of lengthening along the anatomical axis of the femur and its clinical impact. World J Orthop 2017; 8(5): 431-435
- URL: https://www.wjgnet.com/2218-5836/full/v8/i5/431.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i5.431
The goal of recent advances in the field of limb lengthening is to increase the patient acceptance and comfort and avoid the common complications of the classic external fixators. One important achievement is the use of totally implantable intramedullary distracting nails for tibia and femur. Among them, the Albizzia nail (DePuy, Villeurbanne, France), Fitbone (Wittenstein, Igersheim, Germany), Intramedullary Skeletal Kinetic Distractor (ISKD, OrthofixInc., McKinney, TX, United States) and Precise nail (Ellipse Technologies Inc., Irvine, California) were used successfully[1,2]. These are self-lengthening telescopic intramedullary rods, which could be fully motorized or un-motorized and depend on external apparatus or limb movement to make them extend[1]. Intramedullary lengthening utilizes the anatomical axis of the bone, in contrast to lengthening with external fixators which occurs along the mechanical axis. In the tibia, no difference would be detected after either ways of lengthening since the anatomical and mechanical axes of the tibia are almost the same[3]. However, in normal femora, the mechanical and anatomic femoral axes diverge by approximately 5°-9°. This angle is known as the anatomic-mechanical angle (AMA)[2-4]. When using intramedullary lengthening in femora, lateralization of the overall limb alignment has been observed both theoretically and radiologically[2-7]. The amount of mechanical axis lateralization has been documented by Burghardt et al[2], who concluded that each 1 cm lengthening of the femur results in about 1 mm lateralization of the mechanical axis radiologically. However, the exact clinical outcome of such mechanical axis lateralization has not been presented clearly in literature. The purpose of this study is to review the exact effect of lengthening along the anatomical axis on disturbing the normal mechanical alignment of the limb and hence distribution of load along the joint surface. We have reviewed the trigonometric formula to predict the change of the femoral AMA after lengthening along the anatomical axis, and reflected the results on the clinical outcome of mechanical axis deviation.
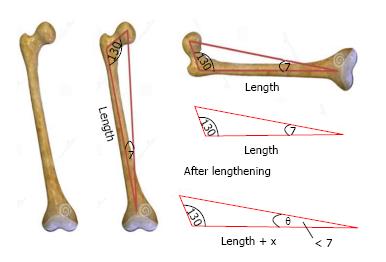
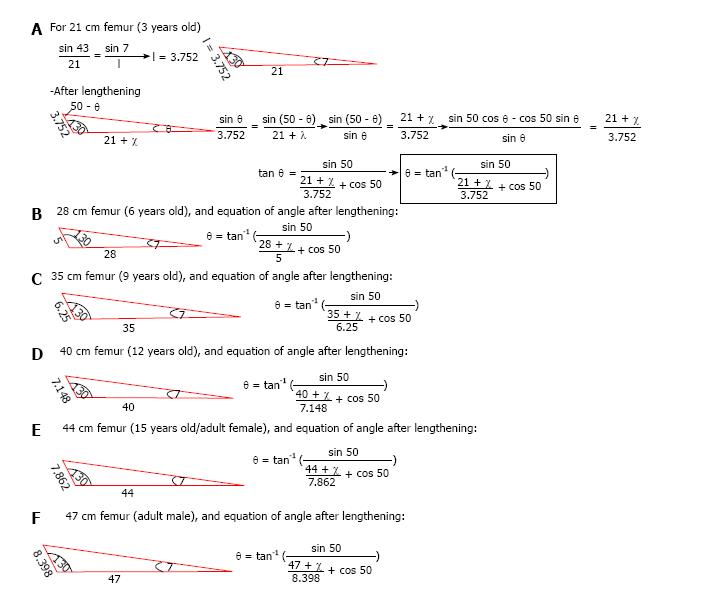
Trigonometry was used to calculate the change in the angle between the femoral mechanical and anatomical axes resulting from lengthening along the anatomical axis. The original angle is assumed to be 7°, where “θ” is the angle after lengthening the femur a distance of “x” cm (Figure 1).
The angle θ was calculated for different original bone lengths and different lengthening distances. Original bone lengths used in our calculations are average lengths that vary from 21 cm for a 3 years old, up to 44 cm for an adult female and 47 cm for an adult male[6]. Femur lengths were considered for different ages with a step of 3 years of age, and so 3, 6, 9, 12, 15 years old, adults’ femurs were considered. Lengthening distances that were considered to vary from 3 to 18 cm, adding 3 cm each step (3, 6, 9, 12, 15, and 18) (Figure 2).
Results of the change of the femoral AMA after lengthening were expressed in Table 1. From the calculations, it was deduced that increasing the bone length by 10% its original length results in reduction of the angle between the mechanical and anatomic axes by 0.57°, and increasing the length by 20% reduces the angle by 1.05° approximately.
| Femur length (cm) | X | P | θ | Δθ |
| 21 | 3 | 14 | 6.21 | 0.79 |
| 6 | 28 | 5.58 | 1.42 | |
| 9 | 42 | 5.06 | 1.94 | |
| 12 | 57 | 4.64 | 2.36 | |
| 15 | 71 | 4.28 | 2.72 | |
| 18 | 85 | 3.97 | 3.03 | |
| 28 | 3 | 10 | 6.38 | 0.62 |
| 6 | 21 | 5.87 | 1.13 | |
| 9 | 32 | 5.44 | 1.56 | |
| 12 | 42 | 5.06 | 1.94 | |
| 15 | 53 | 4.73 | 2.27 | |
| 18 | 64 | 4.45 | 2.55 | |
| 35 | 3 | 8 | 6.5 | 0.5 |
| 6 | 17 | 6.07 | 0.93 | |
| 9 | 25 | 5.69 | 1.31 | |
| 12 | 34 | 5.36 | 1.64 | |
| 15 | 42 | 5.06 | 1.94 | |
| 18 | 51 | 4.8 | 2.2 | |
| 40 | 3 | 7 | 6.56 | 0.44 |
| 6 | 15 | 6.17 | 0.83 | |
| 9 | 22 | 5.83 | 1.17 | |
| 12 | 30 | 5.52 | 1.48 | |
| 15 | 37 | 5.25 | 1.75 | |
| 18 | 45 | 5 | 2 | |
| 44 | 3 | 7 | 6.6 | 0.4 |
| 6 | 13 | 6.24 | 0.76 | |
| 9 | 20 | 5.92 | 1.08 | |
| 12 | 27 | 5.63 | 1.37 | |
| 15 | 34 | 5.37 | 1.63 | |
| 18 | 41 | 5.13 | 1.87 | |
| 47 | 3 | 6 | 6.62 | 0.38 |
| 6 | 12 | 6.28 | 0.72 | |
| 9 | 19 | 5.98 | 1.02 | |
| 12 | 25 | 5.7 | 1.3 | |
| 15 | 32 | 5.45 | 1.55 | |
| 18 | 38 | 5.22 | 1.78 |
Our hypothesis was that the femoral lengthening along the anatomical axis with a telescopic intramedullary nail induces reduction of the femoral anatomical mechanical angle (AMA) which is normally around 7°. This may compensate for the limb mechanical axis that lateralization that was proven both theoretically and radiologically[2-4,6], and hence could partially justify the minimal clinical impact of such mechanical angle lateralization after intramedullary lengthening.
A shift of the mechanical axis of the limb has been reported differently in studies about lengthening with a telescopic intramedullary nails[2,8-11]. Theoretically, Burghardt et al[4] found lateralization of the limb mechanical axis after lengthening along the anatomical axis using trigonometry. Radiologically, Bughdart et al[2] found that 26 of 27 limbs which had intramedullary lengthening with the Precise nail, had a lateral shift of the mechanical axis, and concluded that lengthening of the femur by 1 cm causes lateral shift of the limb mechanical axis by 1 mm. In a similar study about femoral lengthening with the Albizzia nail, Guichet et al[12] found that a lateral shift of the mechanical axis of the limb was seen in all the study cases, with a mean increase in the genu valgum angle by 1.04 degrees, however they could not find a constant correlation between the amount of mechanical axis deviation and the gain in femoral length. Similarly, Baumgart et al[8] found a maximal mechanical axis deviation of 2 mm after using fully motorized intramedullary nails in femoral lengthening, and hence they recommended shifting the distal fragment laterally before reaming, in order to achieve normal mechanical alignment. Other similar studies about intramedullary femoral lengthening either have not commented on the mechanical axis deviation[9], noticed very rare occurrence of mechanical axis deviation[5,10] or did not find any mechanical axis alteration nor angular deformities after lengthening[11].
On the other hand, all the studies which found a radiological mechanical axis deviation after femoral lengthening with intramedullary nails did not comment on the isolated femoral axes relation changes, which in our case represented by the distal femoral AMA. Clinically, all these studies have described that mechanical axis lateral shift to be inconsequent or clinically insignificant[2,5,7,9-12]. This might support our hypothesis, that such mechanical axis shift could be partially compensated by reduction in the distal femoral AMA concluded in our study, and hence no clinical consequences could be observed. Also this might be attributed due to the wide variation of the mechanical limb alignment in (normal) individuals. In the study of Ekhoff et al[13], only 2% of normal limbs included in the study have a neutral mechanical axis, and as many as 76% deviate from neutral by > 3° varus when measured using CT. Also, Bellemans et al[14] found that limb alignment differs between males and females as studied by using full-length lower limb radiographs. In this study, 32% of male and 17.2% female knees were in > 3° of constitutional varus. Similarly, Yaniv et al[15] found that varus knee axis deviation is normally present in football players older than 13 years old.
The mechanical axis is supposed to be the line of body weight loading the joints to the ground, and since the body centre of gravity could be affected greatly by postural abnormalities that may be present in different patients, marked differences in the limb mechanical axes could be seen in different individuals. The situation is further complicated by differences in the alignment of the limb when measured in a lying position (which is non-weight bearing) and in a weight-bearing standing position[16]. In a study by Deep et al[17], they found the limb alignment to be dynamic process that differs according to different postures, and also varies between males and females in normal knees. Deep et al[17] found also a greater tendency into varus malalignment in the study group with normal non-arthritic knees, that go into more varus when changing the position from supine to standing. Walcox et al[16] found similar changes in arthritic knees. Again, the presence of nutritional abnormalities in Calcium and vitamin D metabolism could lead high prevalence of mechanical axes varus malalignment in normally looking adolescents[18]. Again, in general population and different races, there is a range of varus and valgus deformation that has no clinical effect, and there is no fixed number for the normal anatomical shape of human bone. Some mild change during lengthening can stay in most of the cases within this range. The assumption of fixed normal passage of mechanical loading on the limb is not exactly compatible with reality due to the different positions the normal human body use along the day in normal life. Also there is no objective Empirical data to prove where is the normal passage of mechanical axis in relation to the human joints. Since the aim of deformity correction surgery is to reproduce the near normal anatomical shape of bones to improve function, anatomical axis should be the main guide for surgeons in deformity correction and limb reconstruction.
All these data, beside the fact that even the documented amount of mechanical axis lateralization, 1 mm for each 1 cm lengthening, remains very little, this may further justify that the actual implementation of the mechanical axis deviation on the clinical outcome could be very mild or even non significant.
In conclusion, although mechanical axis lateralization after lengthening along the anatomical axis was documented theoretically and radiologically in literature, we found that lengthening of the femur along the anatomical axis theoretically reduce the distal femur AMA by around 0.57 degrees approximately for lengthening by 10% of the original bone length. This change, along with the high variation of population mechanical limb alignment could justify the minimal clinical effect seen with of such mechanical axis deviation after femoral lengthening along the anatomical axis.
Bone lengthening and deformity correction surgery consider the mechanical and anatomical axes during the surgical planning and treatment. This review article aim to stimulate critical thinking to some fixed ideas in the community of orthopaedic surgeons, specially pediatric orthopedics and limb reconstruction.
There are objective data about anatomical shape of bone and the range of normal variation but there is no sufficient data regarding the normal mechanical axis and its variation between normal population.
The authors recommend considering anatomical axis as the main guide for lengthening, and not to over emphasize on mechanical axis, and mild variations in anatomical axis during lengthening.
Lengthening along anatomical axis is safe and effective.
Anatomical and mechanical axis are terms used in deformity correction and bone lengthening.
The authors present a review article about the effects of lengthening along the anatomical axis, using a trigonometric approach. They refer to the topic of mechanical axis lateralisation in intramedullary limb lengthening and check the clinical relevance.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Egypt
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Schiedel FM, Zak L S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | Mahmoud AN, Amgad M, Abdelmohsen MT, Nagy AY, Abuelhadid M, Aref AI, Abdulrahim AF, Al Abdullah MA, Emara K. Is the Intramedullary Skeletal Kinetic Distractor a Safe Measure for Bone Lengthening? A Systematic Review. JOTR. 2014;18:69-78. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Burghardt RD, Paley D, Specht SC, Herzenberg JE. The effect on mechanical axis deviation of femoral lengthening with an intramedullary telescopic nail. J Bone Joint Surg Br. 2012;94:1241-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Paley D. Principles of deformity correction. Berlin: Springer-Verlag 2002; . |
| 4. | Burghardt RD, Herzenberg JE, Burghardt MH. Trigonometric analysis of the mechanical axis deviation induced by telescopic intramedullary femoral lengthening nails. J Appl Biomech. 2011;27:385-391. [PubMed] |
| 5. | Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79:1464-1480. [PubMed] |
| 6. | Muthusamy S, Rozbruch SR, Fragomen AT. The use of blocking screws with internal lengthening nail and reverse rule of thumb for blocking screws in limb lengthening and deformity correction surgery. Strategies Trauma Limb Reconstr. 2016;11:199-205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 7. | Robert N. Hensinger. Standards in pediatric orthopedics: tables, charts, and graphs illustrating growth. New York: Raven Press 1986; . |
| 8. | Baumgart R, Betz A, Schweiberer L. A fully implantable motorized intramedullary nail for limb lengthening and bone transport. Clin Orthop Relat Res. 1997;343:135-143. [PubMed] |
| 9. | Cole JD, Justin D, Kasparis T, DeVlught D, Knobloch C. The intramedullary skeletal kinetic distractor (ISKD): first clinical results of a new intramedullary nail for lengthening of the femur and tibia. Injury. 2001;32 Suppl 4:SD129-SD139. [PubMed] |
| 10. | García-Cimbrelo E, Curto de la Mano A, García-Rey E, Cordero J, Marti-Ciruelos R. The intramedullary elongation nail for femoral lengthening. J Bone Joint Surg Br. 2002;84:971-977. [PubMed] |
| 11. | Singh S, Lahiri A, Iqbal M. The results of limb lengthening by callus distraction using an extending intramedullary nail (Fitbone) in non-traumatic disorders. J Bone Joint Surg Br. 2006;88:938-942. [PubMed] |
| 12. | Guichet JM, Deromedis B, Donnan LT, Peretti G, Lascombes P, Bado F. Gradual femoral lengthening with the Albizzia intramedullary nail. J Bone Joint Surg Am. 2003;85-A:838-848. [PubMed] |
| 13. | Eckhoff DG, Bach JM, Spitzer VM, Reinig KD, Bagur MM, Baldini TH, Flannery NM. Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg Am. 2005;87 Suppl 2:71-80. [PubMed] |
| 14. | Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res. 2012;470:45-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Yaniv M, Becker T, Goldwirt M, Khamis S, Steinberg DM, Weintroub S. Prevalence of bowlegs among child and adolescent soccer players. Clin J Sport Med. 2006;16:392-396. [PubMed] |
| 16. | Willcox NM, Clarke JV, Smith BR, Deakin AH, Deep K. A comparison of radiological and computer navigation measurements of lower limb coronal alignment before and after total knee replacement. J Bone Joint Surg Br. 2012;94:1234-1240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 17. | Deep K, Eachempati KK, Apsingi S. The dynamic nature of alignment and variations in normal knees. Bone Joint J. 2015;97-B:498-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Voloc A, Esterle L, Nguyen TM, Walrant-Debray O, Colofitchi A, Jehan F, Garabedian M. High prevalence of genu varum/valgum in European children with low vitamin D status and insufficient dairy products/calcium intakes. Eur J Endocrinol. 2010;163:811-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |