Copyright
©The Author(s) 2016.
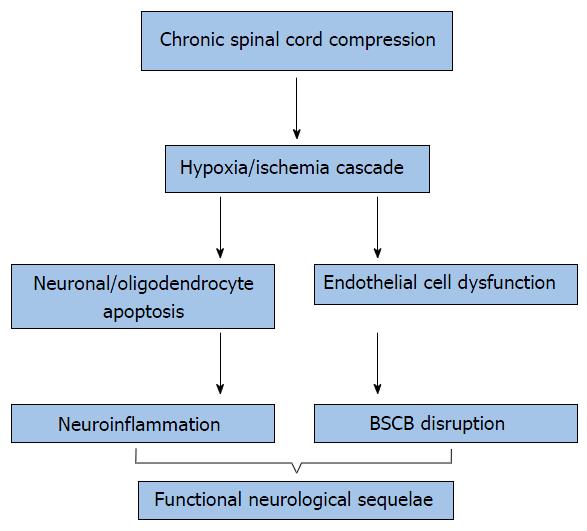
Figure 3 Cellular mechanisms involved in cervical myelopathy.
The hypoxia/ischemia cascade results from chronic progressive compression of the cervical spinal cord. This induces extracellular (TNF-α) and intracellular pro-apoptotic pathways (p-53, JNK), induces neuroinflammation and ultimately, neuronal and oligodendrocyte destruction. Additionally, compromise of the BSCB results from ischemia-induced endothelial cell loss. Increased BSCB permeability alters the cellularity of the spinal cord microenvironment and is thought to further potentiate neuroinflammation. These mechanisms contribute to the upper limb dysfunction, spasticity, and gait disturbances observed in human cervical spondylotic myelopathy. BSCB: Blood-spinal cord barrier; TNF-α: Tumor necrosis factor-α.
- Citation: Dolan RT, Butler JS, O’Byrne JM, Poynton AR. Mechanical and cellular processes driving cervical myelopathy. World J Orthop 2016; 7(1): 20-29
- URL: https://www.wjgnet.com/2218-5836/full/v7/i1/20.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i1.20