Published online May 18, 2015. doi: 10.5312/wjo.v6.i4.400
Peer-review started: January 18, 2015
First decision: February 7, 2015
Revised: February 21, 2015
Accepted: April 10, 2015
Article in press: April 12, 2015
Published online: May 18, 2015
AIM: To systematically evaluate the evidence-based literature on surgical treatment interventions for elite rugby players with anterior shoulder instability.
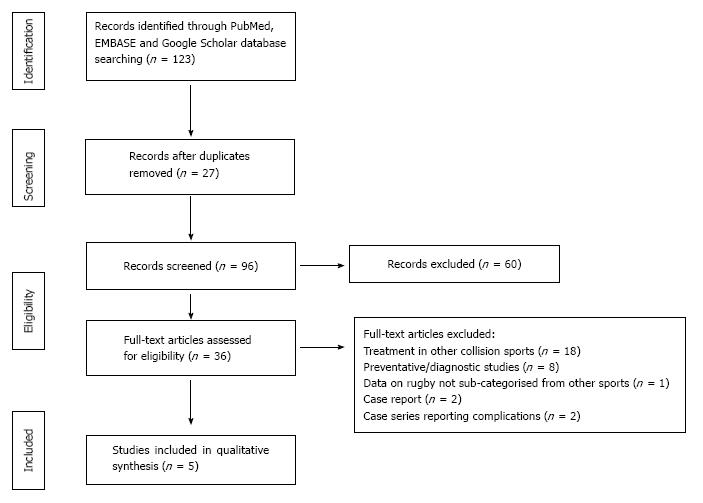
METHODS: We conducted a systematic review according to the PRISMA guidelines. A literature search was performed in PubMed, EMBASE and Google Scholar using the following search terms: “rugby” and “shoulder” in combination with “instability” or “dislocation”. All articles published from inception of the included data sources to January 1st 2014 that evaluated surgical treatment of elite rugby players with anterior shoulder instability were examined.
RESULTS: Only five studies were found that met the eligibility criteria. A total of 379 shoulders in 376 elite rugby union and league players were included. All the studies were retrospective cohort or case series studies. The mean Coleman Methodological Score for the 5 studies was 47.4 (poor). Owing to heterogeneity amongst the studies, quantitative synthesis was not possible, however a detailed qualitative synthesis is reported. The overall recurrence rate of instability after surgery was 8.7%, and the mean return to competitive play, where reported, was 13 mo.
CONCLUSION: Arthroscopic stabilization has been performed successfully in acute anterior instability and there is a preference for open Latarjet-type procedures when instability is associated with osseous defects.
Core tip: Arthroscopic stabilization can be performed successfully for acute anterior instability and an open Latarjet procedure is preferred where there is instability associated with an osseous defect. Interestingly, within the latter group a large proportion of patients do not return to competitive play following their surgery. The evidence base in this field is based on a limited number of studies which lack methodological rigor. As shoulder instability represents a serious musculoskeletal injury within competitive level rugby, there is a need for well-designed trials or sports medicine registries, to better inform orthopaedic surgeons on the management of this cohort of patients.
- Citation: Sabharwal S, Patel NK, Bull AM, Reilly P. Surgical interventions for anterior shoulder instability in rugby players: A systematic review. World J Orthop 2015; 6(4): 400-408
- URL: https://www.wjgnet.com/2218-5836/full/v6/i4/400.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i4.400
The glenohumeral joint is the most mobile joint in the human body owing to its relative lack of osseous constraint[1]. The incidence of shoulder dislocation in the general population is estimated at between 23.9 and 56.3 per 100000 person-years[2,3]. The incidence of instability is double this number in athletes[4]. The largest and most current descriptive epidemiological study in young athletes found that the probability of at least one shoulder instability event per year is 2.8%[5]. Although shoulder instability in professional rugby union accounts for 0.03 injuries per 1000 player-hours, only anterior cruciate ligament injuries cause more days of absence from competitive play[6].
Existing literature on anterior shoulder instability supports primary repair in young and active patients owing to a lower risk of recurrent instability compared to conservative treatment[7]. More recent research demonstrates superiority of open repair over arthroscopic repair in younger male patients in relation to recurrence of instability[8]. Comparative analysis of popularized techniques such as Bristow-Latarjet and Bankart repairs has shown improved clinical outcomes in the former procedure irrespective of the presence of an osseous lesion[9].
Research with a focus on treatment interventions in collision athletes most commonly describes sports such a judo, American football, wrestling and soccer[10,11]. The mechanisms of shoulder instability in elite rugby players have been described as “try scoring” with a hyper-flexed outstretched arm, “tackling” with extension and adduction of the arm, and “direct impact” when there is a compressive force applied to an adducted, internally rotated arm[12]. Although similarities in mechanisms of injury exist with American football[13], the collision forces acting on the shoulder are likely to be different owing to protective equipment worn by football players which are thought to contribute to a significant risk reduction of shoulder injuries when compared to rugby[14]. With the exception of Australian Rules football, the biomechanics of shoulder instability injuries in rugby players is therefore probably distinctive from other collision sports and there is clinical value in research on treatment interventions that specifically focuses on this group of athletes. This study aims to systematically evaluate the evidence-based literature on surgical treatment interventions for elite rugby players with acute and recurrent anterior shoulder instability.
This study was performed in accordance with the guidelines from the preferred reporting items for systematic reviews and meta-analyses (PRIMSA)[15].
A literature search was performed in PubMed, EMBASE and Google Scholar using the following search terms: “rugby” and “shoulder” in combination with “instability” or “dislocation”. The time horizon for search was performed from inception of the databases to January 1st 2014. The last date the search was performed was the 1st July 2014. A summary of the search strategy is shown in Figure 1.
Studies that described a surgical treatment intervention for elite rugby players with anterior shoulder instability were included. Elite rugby players were defined as professional or semi-professionals who participated in both rugby league or rugby union. Studies that described surgical treatment interventions in collision athletes in which there was a sub-group of elite rugby players with their own clinical outcomes specifically reported were also included. Only studies with a minimum follow up of 12 mo were included. Clinical and biomechanical studies were deemed eligible for evaluation. Case reports, expert opinion and personal observations were excluded.
Two investigators (Sabharwal S and Patel NK) independently extracted the following data using a standardized spreadsheet: study title, authorship, year of publication, level of evidence according to the Oxford Centre for Evidence Based Medicine[16], country of origin of research, number of players, type of anterior instability (acute/recurrent), descriptions and frequency of osseous lesions, mean age of surgery, mean time to surgery from injury, surgical stabilization technique, post-operative rehabilitation description, number of players that returned to competition at the same level, mean time for return to full training, mean time for return to competitive match, post-operative evaluation tools and summary, incidence of recurrence of instability, post-operative complications and mean follow up. Patients with acute instability were defined as those who received treatment after a first episode of dislocation. Discrepancies between data extracted by the two investigators were reviewed and corrected. Where there was disagreement on data extracted, consensus was reached after discussion with a senior author (PR).
Study quality was assessed using a modified Coleman Methodology Score (CMS). The CMS is a quality assessment tool that was initially used to grade methodology in patellar tendinopathy studies[17]. It has subsequently been adapted to a wide variety of musculoskeletal research[18,19] and more recently has been used in evaluating methodology of shoulder instability studies[20]. There are 10 criteria that are evaluated giving a total score from 0 to 100 points. A study that scores 100 represents clinical research that largely avoids chance, biases and cofounding factors. Studies can be categorized as excellent (85-100), good (70-84), fair (50-69) and poor (< 50)[20]. Two investigators (SS and NKP) independently scored the included studies using the modified CMS (Table 1).
| Only one score to be given for each of 7 sections | ||
| Study size | < 20 | 0 |
| 20-50 | 4 | |
| 51-100 | 7 | |
| > 100 | 10 | |
| Mean follow up | < 12 mo | 0 |
| 12-36 mo | 4 | |
| 37-60 mo | 7 | |
| > 61 mo | 10 | |
| Surgical or conservative approach | Different approach used and outcome no reported separately | 0 |
| Different approaches used and outcome reported separately | 7 | |
| Single approach used | 10 | |
| Type of study | Retrospective cohort | 0 |
| Prospective cohort | 10 | |
| Randomised controlled trial | 15 | |
| Description of indications/diagnosis | Described without % specified | 0 |
| Described with % specified | 5 | |
| Description of surgical or conservative technique | Inadequate (not stated, unclear) | 0 |
| Fair (technique only stated) | 5 | |
| Adequate (technique stated, details of surgical or conservative procedure given) | 10 | |
| Description of postoperative rehabilitation | Described | 5 |
| Not described | 0 | |
| Scores may be given for each option in each of the 3 sections if applicable | ||
| Outcome criteria | Outcome measures clearly defined | 2 |
| Timing of outcome assessment clearly stated | 2 | |
| Use of outcome criteria that has reported reliability | 3 | |
| General heath measure included | 3 | |
| Procedure of assessing outcomes | Participants recruited | 5 |
| Investigator independent of surgeon | 4 | |
| Written assessment | 3 | |
| Completion of assessment by patients themselves with minimal investigator assistance | 3 | |
| Description of subject selection | Selection criteria reported and unbiased | 5 |
| Recruitment rate reported > 90% | 5 | |
| ≤ 90% | 0 | |
Descriptive statistics were produced and data were analyzed in SPSS 21.0 (SPSS Inc, Chicago, IL). Inter - rater reliability for the modified CMS was assessed with a Pearson’s R coefficient. An average of the two investigators’ scores for each study was presented in the results.
In total only five studies were found that met the eligibility criteria of this systematic review (Table 2).
| Ref. | Journal | Level ofevidence | Country | No. of players (shoulders) | Type ofinstability | Osseous lesion(s) |
| Neyton et al[23] | Journal of shoulder and elbow surgery | IV | France | 34 (37) | Recurrent, anterior | Bony Bankart 18/37, Hills-Sachs 25/37 |
| Bonnevialle et al[21] | Rev Chir Orthop Reparatrice Appar Mot | IV | France | 31 | Recurrent, anterior | None |
| Larrain et al[26] | Arthroscopy | IV | Argentina | 198 | Acute anterior instability (40), recurrent anterior instability (158) | Large bony defect: Bony Bankart 16/198, Hills-Sachs 2/198, Combined 9/198 |
| Small bony defect: Bony Bankart < 25% 36/198, Hills Sachs < 1/4 172/198 | ||||||
| Goldberg et al[24] | British Journal of Sports Medicine | IV | Australia | 6 | Acute anterior instability (1/6), chronic recurrent (5/6), all patients had rotator cuff tears | 1/6 Bony bankart |
| Burkhart et al[25] | Arthroscopy | IV | United States/South Africa | 96 | Anterior instability acute and recurrent | 8/96 Bony Bankart and Hill-Sachs |
Bonnevialle et al[21] reported on 31 rugby players with recurrent shoulder instability and their data formed part of a subsequent study by Fabre et al[22] that examined outcomes in 49 contact athletes[21,22]. To ensure the same patient group was not included twice, the latter group’s article was excluded from our analysis. All the studies were retrospective cohort or case series studies (Level of Evidence IV). A total of 368 shoulders in 365 elite rugby union and rugby league players were included. Overall, the mean age at surgery was 23.2 years, with a range from 16 to 35 years (Table 3). The mean duration of follow up was 72 mo, with a range of 17 mo to 237 mo (Table 4). Return to competitive play was reported in 230 out of 269 patients (85.5%) at a mean time of 13 mo, with a range of 2 to 24 mo. Recurrence of instability occurred in 32 of the 368 cases (8.7%).
| Ref. | Mean age of player at surgery Years (range) | Mean time to surgery Months (range) | Type of stabilization | Post-operative treatment | No. of players that returned to competition after surgery | Mean return to competitive match |
| Neyton et al[23] | 23.4 (17-33) | 40 (3-163) | Latarjet-Patte procedure (Anterior instability) | Sling for 15 d with passive exercises and no limitation on external rotation. Return to rugby advised at 3 mo | 22/34 | 7 mo (3-24) |
| Bonnevialle et al[21] | 21 (16-34) | 4.44 (2-20) | Open Bankart capsular repair | Immobilisation Velpeau bandage for 2-3 wk. No formal physiotherapy | 30/31 | 4.6 mo (2-8) |
| Larrain et al[26] | 22 (16-35) | For acute (all within 3 wk, Recurrent not specified | Arthroscopic acute (39/40) | Not stated | Acute 40/40 | Acute: 5.3 mo (4-7) |
| Mini open acute (conversion from arthroscopic 1/40) | ||||||
| Arthroscopic recurrent (121/158) | Recurrent 133/158 | Recurrent: 7.5 mo (5.5-9) | ||||
| Open recurrent (Latarjet 37/158) | ||||||
| Goldberg et al[24] | 26.5 (23-29) | Not stated: Mean time between presentation and operation 5.9 d (2-15) | 2 Stage Open RC suture repair and approximately 9 wk later open capsular repair/osseous bankart repair | After RC repair: sling immobilisation for 6 wk with passive ROM exercise at 3 d. At 6 wk active exercise programe. After Stabilisation: 6 wk immobiisation then passive ROM exercises and light weights after 4 mo | 5/6 players (1 player retired because of other injuries) | 9 mo |
| Burkhart et al[25] | Not specified for rugby players | Not specified for rugby players | Arthroscopic capsular ± open capsular shift or Latarjet for when osseous lesion present | 3 wk immobilisation in a sling, forward flexion at 3 wk, ER at 6 wk, Strengthening at 8 wk | Not stated | Not stated |
| Ref. | Post-operative evaluation tools | Recurrence of instability | Complications | Mean follow up months (range) | Mean Coleman Methodology Score |
| Neyton et al[23] | Radiographic, Walsh-Duplay score (mean 86), Rowe score (mean 93), VAS score (mean 1.6) | 0/37 | 3/37 (1 glenoid fracture, 1 post op haematoma, 1 pseudoarthrosis of bone block) | 144 (68-237) | 58 |
| Bonnevialle et al[21] | Mean external rotation decreased 6.2 degrees, Rowe (excellent for 86%), Walsh-Duplay (excellent for 80%), patient satisfaction (88%), Samilson radiographic degeneration in 32% | 6/31 | None stated | 82 (60-120) | 48 |
| Larrain et al[26] | Acute: Rowe 33/40 excellent, 4/40 good, 2/40 poor | Arthroscopic acute (2/40) | 1/198 (radial paraesthesia) | 68.4 (39.6-99.6) | 55 |
| Recurrent: Rowe 105/158 excellent, 6/158 good, 10/158 poor) | Recurrent (10/158) | ||||
| Goldberg et al[24] | ROM normal except external rotation 70% and internal rotation 60% compared to contra-lateral side | 0/6 | None | 34.3 (12-50) | 42.5 |
| Burkhart et al[25] | Not stated | Non osseous lesion (6/87 re-dislocated), osseous (8/9 re-dislocated ) | Not specified | Not stated | 35 |
A complete sub-group comparison of all pathology and treatment related recurrence rates was not possible because of lack of specific descriptions within some of the studies. However, where reported recurrent instability after surgery occurred in only 1 out of 41 (2.4%) reported cases of acute instability and 16 out of 231 (6.9%) cases of chronic or recurrent shoulder instability. Furthermore, recurrence of instability after arthroscopic surgery was reported in only 2 out of 39 (5.1%) cases compared to reported recurrences in 14 out of 84 (16.7%) cases after an open surgical technique was performed. Recurrence after soft tissue surgical techniques were adopted occurred in 7 out of 133 (5.2%) cases and recurrence after a Latarjet procedure was performed occurred in 14 out of 77 (18.2%) cases. It was observed that where open procedures were performed instead of arthroscopic procedures, or a Latarjet procedure in preference of soft tissue stabilization, the patients groups were more likely to have osseous defects.
Descriptions of soft tissue and bone defects were found to be incomplete in a majority of the studies[21,23-25]. Soft tissue Bankart lesions were reported in three studies[21,24,26] in which they were identified in 208 (88.5%) out of 235 shoulders. The presence of a boney Bankart and Hills-Sachs lesion was described in two studies that evaluated a total of 235 shoulders[23,26]. Cumulatively, they reported 79 (33.6%) boney Bankarts and 199 (84.7%) Hills-Sachs lesions. One study examined instability in conjunction with rotator cuff injury and reported a supraspinatus tear in all 6 patients included in their case series[24].
A number of different outcome measures were reported in the included studies (Table 4). The most commonly adopted was the Rowe score for shoulder instability that was used in 3 (60%) of the 5 studies. The Walch-Duplay Score was reported in 2 studies. There were two studies that did not adopt any patient reported outcome measures[24,25].
The surgical management of acute anterior instability was described in 3 studies[24-26]. Interpretation of the results of two of these studies is challenging because Burkhart et al[25] did not clearly differentiate their population of rugby players with acute instability from those with recurrence. However, this study did state that of the 87 rugby players that underwent an arthroscopic capsular repair, there were 6 (6.9%) that had a recurrent episode of instability and amongst the 9 players that had an open capsular shift or Latarjet procedure, there were 8 (88.9%) that had recurrent instability. Goldberg et al[24] described a two-stage procedure for management of rotator cuff injury associated with acute anterior instability in 6 players. None of the players were reported to have gone on to re-dislocate their shoulder. Only Larrain et al[26] clearly described the surgical management of acute anterior instability in rugby players in the absence of other significant shoulder pathology. There were 40 patients that underwent acute arthroscopic repair us within 3 wk of the patient’s first dislocation. A modification of the suture anchor technique described by Synder and Strafford was performed by the surgeons in this study[26]. One of the cases was converted to a mini-open procedure intra-operatively for a humeral avulsion of the glenohumeral ligament (HAGL) reinsertion. Post-operative rehabilitation was not described, however all 40 rugby players returned to competitive play 7 mo after their surgery. Within this group of players 2 (5%) had a recurrent dislocation whilst playing rugby within 2 years of surgery.
Surgical intervention for recurrent anterior instability was described in 4 of the studies[21,23,25,26]. Burkhart et al[25] reported on the combined results of both acute and recurrent anterior instability. Neyton et al[23] performed a Latarjet-Patte procedure on 37 shoulders in 34 rugby union players. A boney lesion on the glenoid was present in 27 (73%) cases, of which 18 (48.6%) were reported to be glenoid fractures. Only 22 (64.7%) players returned to play competitive rugby and the mean time of return to match fitness was 7 mo (range 3-24). The authors reported that only 1 of the 12 players stopped competitive rugby because of a problem related to his shoulder. This patient had apprehension to contact. The remaining 11 patients were reported to have retired from competitive rugby because of reasons independent from their operated shoulder. None of the patients had a recurrence of their instability at a mean follow up of 144 mo (range 68-237).
Bonnevialle et al[21] performed an open Bankart repair for recurrent instability in 31 rugby players. The authors reported that none of the players had a major bony Bankart or Hills-Sachs lesion. Thirty (96.8%) of the players returned to competitive match play at a mean time of 4.6 mo (range 2-8). There were 6 (19.4%) cases of recurrence of dislocation whilst playing rugby that occurred on average 3.8 years (range 0.5-6) years after surgery.
Larrain et al[26] reported on the management of 158 shoulders in rugby players with recurrent anterior instability[26]. Players were managed with a modified Latarjet procedure, or an arthroscopic suture anchor technique that they also used for their patients with acute anterior instability. A specific exclusion criteria for arthroscopic reconstruction in their study included; bone loss > 25% on the glenoid, a Hills-Sachs lesion comprising greater than one quarter of articular head, capsular laxity with poor quality tissue and the presence of a HAGL. Of the 121 arthroscopic cases for recurrent anterior instability, there were 10 (8.3%) recurrences of instability which fared slightly worse than the 2 (5%) cases of recurrence in their acute anterior instability cohort. There were no cases of recurrent instability in the group of patients that underwent a modified Latarjet procedure. One hundred thirty-three (84.2%) of the 158 players with recurrent anterior instability returned to competitive match play at a mean time of 7.5 mo (range 5.5-9). The authors did not provide data on how this differed between open and arthroscopic surgery.
Complications were reported in only 4 of the studies[23,24,26] (Table 4). There was an overall complication rate of 1.7% (5 out of 290 patients). In Neyton et al[23]’s study, 3 patients had a fracture of the bone block observed on radiographs taken 3 mo postoperatively and one of these patients required revision surgery. Larrain et al[26] had one case of radial nerve paraesthesia which resolved after 9 mo.
A comparison of each CMS domain scores between the two raters using a Pearson’s correlation was 0.966, indicative of strong inter-rater reliability. The mean CMS score for the 5 studies included in this systematic review was 47.4 (range 35-58) (Table 4). None of the studies had “excellent” (85-100) or “good” (70-84) CMS scores. Two studies had a “fair” CMS score (55-69) and 3 had a “poor” CMS score (< 55).
This systematic review has found that there is a dearth of published evidence that evaluates surgical interventions for shoulder instability in the elite rugby player. The few studies that exist are based on retrospective cohort or case series, and on average their methodological quality is poor. Considerable heterogeneity between the 6 studies means that inference of overall outcomes, instability recurrence rates and complications rates has limitations.
Larrain et al[26] produced the most comprehensive analysis on treatment of acute anterior shoulder instability. Amongst the 40 rugby players that underwent arthroscopic capsular repair there were only 2 (5%) episodes of recurrent instability. These results compare favorably to a cited recurrence rate of 11% in the general population[27] and 14.3% in young athletes[28] treated with arthroscopic stabilization repairs for acute anterior instability. Interestingly, Larraine et al[26] found that that amongst the 121 patients who underwent arthroscopic stabilization for recurrent instability the results were slightly poorer as 10 (8.3%) players sustained a subsequent dislocation. Higher rates of dislocation are reported after arthroscopic surgery for patients with recurrent instability in other collision sports. Mazzoca et al[10] reported on a case series of 13 collision athletes (American football) who underwent arthroscopic stabilization for recurrent anterior shoulder instability and 2 (15%) experienced a recurrent dislocation. Larrain et al[26] described specific criteria for patients undergoing arthroscopic surgery, and therefore it is unlikely that underlying osseous pathology contributed to a higher risk of dislocation in the group with recurrent instability. Existing evidence indicates that there is no difference in recurrence among patients undergoing arthroscopic stabilization after primary dislocation compared with those who have surgery after multiple recurrent episodes[29]. This research is based on general population studies and this limits its applicability to collision athletes or rugby players. Repeated traumatic dislocations in rugby may attenuate anterior soft tissue structures in the shoulder and make delayed arthroscopic surgery more difficult. Furthermore it is possible that there is more disruption to sporting activities from recurrent instability and apprehension that occurs in players treated conservatively after their first dislocation. Such factors lend credence to the hypothesis that early arthroscopic stabilization in rugby players may result in better clinical outcomes and earlier return to competitive play. Future research within this domain should test this hypothesis from a clinical viewpoint as well examine the financial impact on both player and club.
Open anterior stabilization surgery is recommended in young male patients and has been demonstrated to be more favorable than arthroscopic surgery in collision athletes based on a lower incidence of recurrence of instability[8,30]. With the exception of a single mini open procedure performed for a HAGL by Larrain et al[26], only Bonnevialle et al[21] performed open capsular repair on their patients with anterior instability. Their study reported that 19.4% of rugby players had a subsequent dislocation. This is more than twice the recurrence rate Larrain et al[26] presented in their cohort of rugby players treated with arthroscopic capsular repair and considerably higher than the results of an American study that reported a recurrence rate of 3% for open capsular repair fin American football players with recurrent anterior instability[31]. Heterogeneity between the studies in our review and the limitations of their methodological quality underline the need for rugby specific studies to reliably inform clinicians whether a significant difference in outcome exists between open and arthroscopic anterior shoulder stabilization.
Two of the three studies that described a Latarjet type procedure for anterior shoulder instability stated it was performed for specific indications related to bone loss on the glenoid. Although Burkhart et al[25] reported 8 recurrent dislocations out of their 9 patients, there were no subsequent episodes of instability in the 64 shoulders operated on in the other 2 studies[23,26]. Despite the apparent success of restoring shoulder stability, both these studies reported that a large number of players were not able to return to a competitive level. Bony stabilization for anterior shoulder instability is often considered the gold-standard treatment especially in cases where there are osseous defects, however they are associated with a 30% complication rate[32]. More evidence is needed to establish whether it is offers any benefit over capsular repair when osseous defects are not present, and specifically whether it can achieve stability in rugby players and allow them to return to their previous sporting level.
Over the last decade there has been a significant increase in publication of Level I and II evidence in sports medicine and orthopaedic surgery[33,34]. As a result of the potential of serious injury and disability, the management of head and neck injury has been the focus of much of the current clinical research that is ongoing in rugby[35-37]. Research evaluating shoulder instability in rugby players may be lacking because of the perception that the disability that follows such an injury is not common or severe enough to warrant the effort and financial cost of research. Epidemiological research in English professional rugby union has shown that on average, shoulder instability is the second most severe musculoskeletal injury after ACL rupture in terms of absence from competitive play, and results in a mean time of 22.4 wk of absence from training or match play[6]. Furthermore, many of the studies identified in this review have demonstrated that a concerning proportion of players are unable to return to their previous level of sport and are forced to retire soon after surgery. Professional rugby has been transformed over the last 20 years and the revenue of the Rugby Football Union in the 2012/2013 financial year was £153.5 million[38]. Responsible professional bodies have financial and ethical interests in supporting research related to the prevention and management of injuries sustained by their athletes. This is often seen in football, for example, where the Fédération Internationale de Football Association funds clinical research in football players[39].
Prospective randomized trials comparing interventions such as arthroscopic versus open capsular repair in rugby players would be the gold-standard model for future research, however the creation of professional rugby association health databases, similar to the National Basketball Association epidemiological database in the United States[40], would also provide important retrospective data on outcomes of treatment. Furthermore biomechanical laboratory and computer simulation studies that are tailored to the forces exerted on a rugby player’s shoulder[41] and compare stability and function after different surgical procedures would also offer important information on optimal management.
The main weakness in this study relates to a lack of existing research within this field which has limited our ability to draw conclusions on the benefit of different treatment interventions. The 5 studies we identified were heterogeneous in patient selection, pathologies and measurement of outcome measures. Despite this, we adopted recognized methodology to systematically reviewing the evidence in this field[15] and this has allowed us to summarize successful management techniques as well as recurrence rates of instability cited by different studies.
Existing research that evaluates surgical treatment interventions for shoulder instability in elite rugby players is limited. Arthroscopic stabilization has been performed successfully in acute anterior instability and there is a preference for an open Latarjet procedure when instability is associated with osseous defects, however the current evidence base consists of a small number of studies with poor methodological quality. Clinicians are likely to continue to inform their practice using research that is based on other collision sports or general population studies. This paper underlines aspects of treatment that future clinical and basic science research should be directed towards in order to improve management of one of the most severe musculoskeletal injuries in elite rugby players.
Anterior shoulder instability is one of the most severe musculoskeletal injuries in elite-level rugby in terms of days of competitive play lost. The biomechanics of this injury are distinct from other contact sports and therefore research with a focus on rugby players may have more clinical applicability.
To the best of our knowledge, no systematic review evaluating treatment options for anterior shoulder instability in rugby players has been published. The aim of this study was to systematically review all published studies that investigated surgical management for anterior shoulder instability in elite rugby players.
Arthroscopic stabilization for acute anterior instability has been performed successfully in a few clinical studies. A Latarjet-type procedure is performed preferentially when there is an osseous defect associated with the instability, however a large proportion of rugby players with such injuries do not return to competitive level sports.
Although this study can inform clinicians on proven surgical techniques such as arthroscopic stabilization in the case of acute anterior instability, or Latarjet-type procedures where there an osseous defect, the results also provide realistic rehabilitation timeframes and return to match play information based on the current evidence base. Importantly, the limitations in currently available evidence, underlines aspects of treatment that future clinical and basic science research should be directed towards in order to improve management of one of the most severe musculoskeletal injuries in elite rugby players.
A Bankart lesion is an injury of the anterior-inferior glenoid labrum that occurs due to an anterior shoulder dislocation. It predisposes the shoulder to further episodes of anterior instability. A boney Bankart is a fracture of the anterior-inferior glenoid rim that may accompany this injury. A Latarjet procedure is a surgical procedure often used to treat a boney Bankart lesion, in which a section of the coracoid process and its attached tendons are transferred to the anterior aspect of the glenoid to prevent ongoing anterior instability.
This manuscript is well organized and written.
P- Reviewer: Daglar B, Hantes M S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Halder AM, Kuhl SG, Zobitz ME, Larson D, An KN. Effects of the glenoid labrum and glenohumeral abduction on stability of the shoulder joint through concavity-compression: an in vitro study. J Bone Joint Surg Am. 2001;83-A:1062-1069. [PubMed] [Cited in This Article: ] |
| 2. | Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am. 2010;92:542-549. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 434] [Cited by in F6Publishing: 443] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 3. | Liavaag S, Svenningsen S, Reikerås O, Enger M, Fjalestad T, Pripp AH, Brox JI. The epidemiology of shoulder dislocations in Oslo. Scand J Med Sci Sports. 2011;21:e334-e340. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 80] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 4. | Wang RY, Arciero RA. Treating the athlete with anterior shoulder instability. Clin Sports Med. 2008;27:631-648. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med. 2007;35:1168-1173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 304] [Cited by in F6Publishing: 293] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 6. | Brooks JH, Fuller CW, Kemp SP, Reddin DB. Epidemiology of injuries in English professional rugby union: part 2 training Injuries. Br J Sports Med. 2005;39:767-775. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 179] [Cited by in F6Publishing: 180] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 7. | Jakobsen BW, Johannsen HV, Suder P, Søjbjerg JO. Primary repair versus conservative treatment of first-time traumatic anterior dislocation of the shoulder: a randomized study with 10-year follow-up. Arthroscopy. 2007;23:118-123. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 195] [Cited by in F6Publishing: 160] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 8. | Mohtadi NG, Chan DS, Hollinshead RM, Boorman RS, Hiemstra LA, Lo IK, Hannaford HN, Fredine J, Sasyniuk TM, Paolucci EO. A randomized clinical trial comparing open and arthroscopic stabilization for recurrent traumatic anterior shoulder instability: two-year follow-up with disease-specific quality-of-life outcomes. J Bone Joint Surg Am. 2014;96:353-360. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 100] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 9. | Hovelius L, Vikerfors O, Olofsson A, Svensson O, Rahme H. Bristow-Latarjet and Bankart: a comparative study of shoulder stabilization in 185 shoulders during a seventeen-year follow-up. J Shoulder Elbow Surg. 2011;20:1095-1101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 125] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 10. | Mazzocca AD, Brown FM, Carreira DS, Hayden J, Romeo AA. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med. 2005;33:52-60. [PubMed] [Cited in This Article: ] |
| 11. | Cho NS, Hwang JC, Rhee YG. Arthroscopic stabilization in anterior shoulder instability: collision athletes versus noncollision athletes. Arthroscopy. 2006;22:947-953. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 115] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 12. | Crichton J, Jones DR, Funk L. Mechanisms of traumatic shoulder injury in elite rugby players. Br J Sports Med. 2012;46:538-542. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 13. | Kaplan LD, Flanigan DC, Norwig J, Jost P, Bradley J. Prevalence and variance of shoulder injuries in elite collegiate football players. Am J Sports Med. 2005;33:1142-1146. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 223] [Cited by in F6Publishing: 199] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 14. | Marshall SW, Waller AE, Dick RW, Pugh CB, Loomis DP, Chalmers DJ. An ecologic study of protective equipment and injury in two contact sports. Int J Epidemiol. 2002;31:587-592. [PubMed] [Cited in This Article: ] |
| 15. | Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [PubMed] [Cited in This Article: ] |
| 16. | Oxford Centre for Evidence Based Medicine. The Oxford 2011 levels of evidence. 2011; Available from: http: //www.cebm.net/ocebm-levels-of-evidence/. [Cited in This Article: ] |
| 17. | Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2-11. [PubMed] [Cited in This Article: ] |
| 18. | Filardo G, Andriolo L, Kon E, de Caro F, Marcacci M. Meniscal scaffolds: results and indications. A systematic literature review. Int Orthop. 2015;39:35-46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 19. | Wang J, Hua Y, Chen S, Li H, Zhang J, Li Y. Arthroscopic repair of lateral ankle ligament complex by suture anchor. Arthroscopy. 2014;30:766-773. [PubMed] [Cited in This Article: ] |
| 20. | Longo UG, Loppini M, Rizzello G, Ciuffreda M, Maffulli N, Denaro V. Management of primary acute anterior shoulder dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy. 2014;30:506-522. [PubMed] [Cited in This Article: ] |
| 21. | Bonnevialle N, Mansat P, Bellumore Y, Mansat M, Bonnevialle P. [Surgical treatment of anterior shoulder instability in rugby players: clinical and radiographic results with minimum five-year follow-up]. Rev Chir Orthop Reparatrice Appar Mot. 2008;94:635-642. [PubMed] [Cited in This Article: ] |
| 22. | Fabre T, Abi-Chahla ML, Billaud A, Geneste M, Durandeau A. Long-term results with Bankart procedure: a 26-year follow-up study of 50 cases. J Shoulder Elbow Surg. 2010;19:318-323. [PubMed] [Cited in This Article: ] |
| 23. | Neyton L, Young A, Dawidziak B, Visona E, Hager JP, Fournier Y, Walch G. Surgical treatment of anterior instability in rugby union players: clinical and radiographic results of the Latarjet-Patte procedure with minimum 5-year follow-up. J Shoulder Elbow Surg. 2012;21:1721-1727. [PubMed] [Cited in This Article: ] |
| 24. | Goldberg JA, Chan KY, Best JP, Bruce WJ, Walsh W, Parry W. Surgical management of large rotator cuff tears combined with instability in elite rugby football players. Br J Sports Med. 2003;37:179-181; discussion 181. [PubMed] [Cited in This Article: ] |
| 25. | Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677-694. [PubMed] [Cited in This Article: ] |
| 26. | Larrain MV, Montenegro HJ, Mauas DM, Collazo CC, Pavón F. Arthroscopic management of traumatic anterior shoulder instability in collision athletes: analysis of 204 cases with a 4- to 9-year follow-up and results with the suture anchor technique. Arthroscopy. 2006;22:1283-1289. [PubMed] [Cited in This Article: ] |
| 27. | Bottoni CR, Wilckens JH, DeBerardino TM, D’Alleyrand JC, Rooney RC, Harpstrite JK, Arciero RA. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30:576-580. [PubMed] [Cited in This Article: ] |
| 28. | Owens BD, DeBerardino TM, Nelson BJ, Thurman J, Cameron KL, Taylor DC, Uhorchak JM, Arciero RA. Long-term follow-up of acute arthroscopic Bankart repair for initial anterior shoulder dislocations in young athletes. Am J Sports Med. 2009;37:669-673. [PubMed] [Cited in This Article: ] |
| 29. | Grumet RC, Bach BR, Provencher MT. Arthroscopic stabilization for first-time versus recurrent shoulder instability. Arthroscopy. 2010;26:239-248. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 30. | Rhee YG, Ha JH, Cho NS. Anterior shoulder stabilization in collision athletes: arthroscopic versus open Bankart repair. Am J Sports Med. 2006;34:979-985. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 163] [Cited by in F6Publishing: 166] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 31. | Pagnani MJ, Dome DC. Surgical treatment of traumatic anterior shoulder instability in american football players. J Bone Joint Surg Am. 2002;84-A:711-715. [PubMed] [Cited in This Article: ] |
| 32. | Griesser MJ, Harris JD, McCoy BW, Hussain WM, Jones MH, Bishop JY, Miniaci A. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review. J Shoulder Elbow Surg. 2013;22:286-292. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 374] [Cited by in F6Publishing: 384] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 33. | Cvetanovich GL, Fillingham YA, Harris JD, Erickson BJ, Verma NN, Bach BR. Publication and level of evidence trends in the American Journal of Sports Medicine from 1996 to 2011. Am J Sports Med. 2015;43:220-225. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 34. | Zaidi R, Abbassian A, Cro S, Guha A, Cullen N, Singh D, Goldberg A. Levels of evidence in foot and ankle surgery literature: progress from 2000 to 2010? J Bone Joint Surg Am. 2012;94:e1121-e1110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 35. | Gardner A, Iverson GL, Levi CR, Schofield PW, Kay-Lambkin F, Kohler RM, Stanwell P. A systematic review of concussion in rugby league. Br J Sports Med. 2015;49:495-498. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 36. | Cusimano MD, Nassiri F, Chang Y. The effectiveness of interventions to reduce neurological injuries in rugby union: a systematic review. Neurosurgery. 2010;67:1404-1418; discussion 1418. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 37. | Kuster D, Gibson A, Abboud R, Drew T. Mechanisms of cervical spine injury in rugby union: a systematic review of the literature. Br J Sports Med. 2012;46:550-554. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 39. | Drezner JA, Dvorak J, Kramer EB, Mandelbaum B, Patricios J, Pedrinelli LF, Schmied C, Zideman D. The FIFA® 11 Steps to prevent sudden cardiac death during football games. Eur Heart J. 2013;34:3594-3595. [PubMed] [Cited in This Article: ] |
| 40. | Starkey C. Injuries and illnesses in the national basketball association: a 10-year perspective. J Athl Train. 2000;35:161-167. [PubMed] [Cited in This Article: ] |
| 41. | Usman J, McIntosh AS, Fréchède B. An investigation of shoulder forces in active shoulder tackles in rugby union football. J Sci Med Sport. 2011;14:547-552. [PubMed] [Cited in This Article: ] |