Published online Mar 18, 2020. doi: 10.5312/wjo.v11.i3.184
Peer-review started: September 28, 2019
First decision: December 24, 2019
Revised: December 24, 2019
Accepted: January 19, 2020
Article in press: January 19, 2020
Published online: March 18, 2020
Processing time: 170 Days and 4.7 Hours
Total knee arthroplasty is one of the most successful operations performed worldwide today. Patellar clunk syndrome (PCS) is a postoperative complication that arises due to the development of a fibrous nodule along the undersurface of the quadriceps tendon. The current literature on PCS has not yet come to a consensus regarding its etiology. To date, this is the first study that analyzes the existing literature on PCS in order to generate a conclusion regarding its etiology. It is hypothesized that prosthesis design is the main component behind the development of PCS.
To determine the etiology of PCS and its association with pre and post-operative characteristics of the prosthesis and native knee.
We conducted a systematic review according to the PRISMA guidelines by searching through PubMed, Cochrane, and Google Scholar from May-July 2018 for cases of PCS using search MeSH terms “patella OR patellar” AND “clunk” OR “catch” OR “crepitus”. The search included case series and clinical trials and excluded review articles, yielding 30 articles from the original search and 3 additional articles from reference lists. We extracted data upon the outcomes in patients afflicted with PCS to determine the etiology of PCS. We performed additional bias assessments to validate our search algorithm and results.
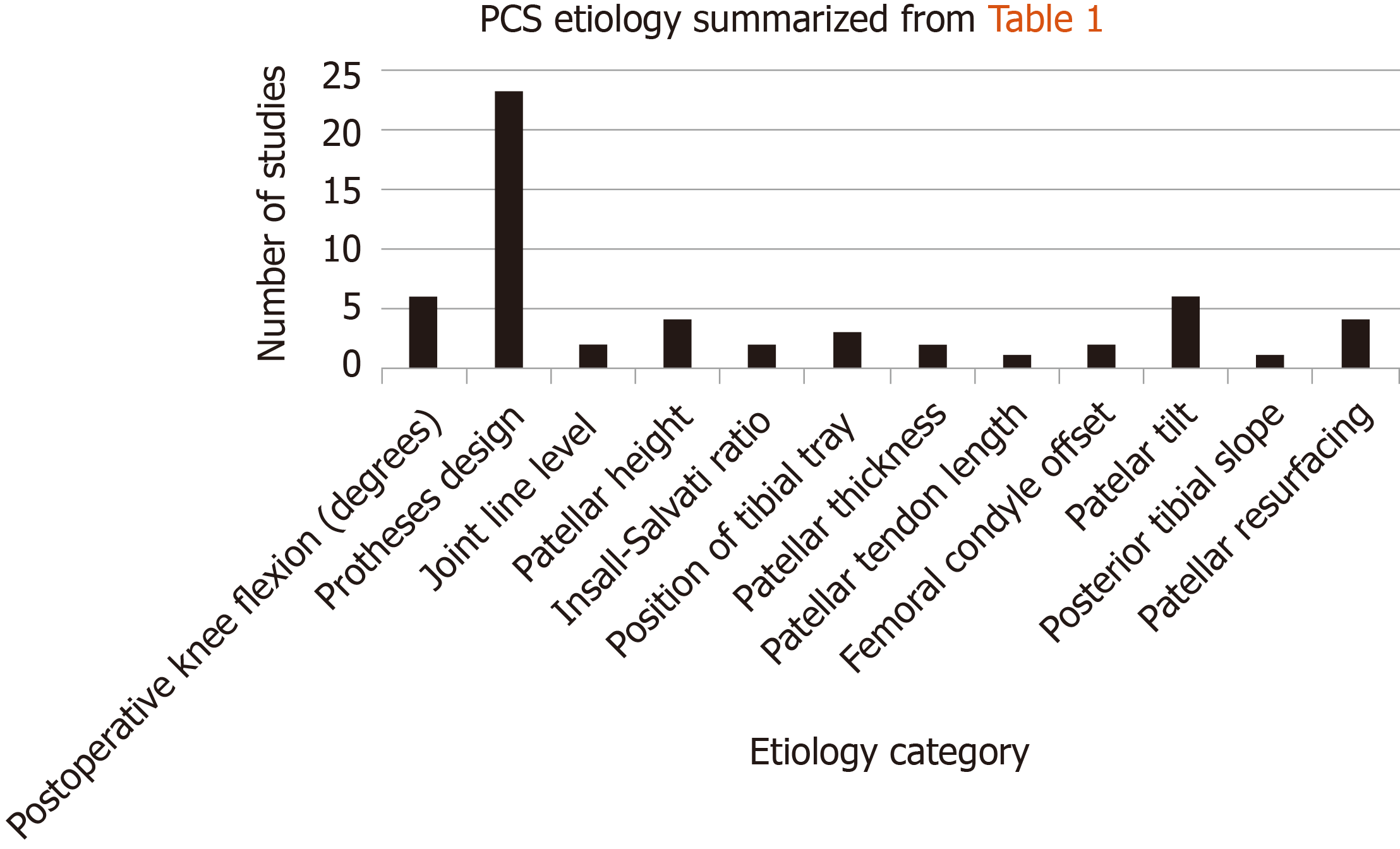
Prosthesis design was the metric most frequently implicated in the incidence of PCS, though several other metrics were contributory toward its pathogenesis. Later prosthetic designs incorporate a reduced intercondylar box ratio and box width to reduce contact between the proximal patellar pole and the intercondylar box, thereby reducing incidence of PCS.
The etiology of PCS is multifactorial, owing to the growing metrics that have associations with its incidence. This conclusion is validated by the significance of prosthesis design as the most likely parameter involved in developing PCS since different prosthesis designs are often the result of different parameters. Future studies should be directed at isolating individual prosthetic parameters of prosthesis designs in order to determine what permutation of parameters is most closely associated with the development of PCS.
Core tip: Patellar clunk syndrome is the development of a fibrous nodule along the undersurface of the quadriceps tendon and proximal to the superior pole of the patella after a posterior-stabilized total knee arthroplasty. It can be diagnosed clinically by its namesake pathognomonic clunk when moving the knee from full flexion to extension with anterior knee pain or by radiograph, ultrasound, or magnetic resonance imaging. Ultimately, the etiology of patellar clunk syndrome is most dependent upon prosthesis design, which is largely dependent upon incorporate a reduced intercondylar box ratio and box width to reduce contact between the proximal patellar pole and the intercondylar box.
- Citation: Sequeira SB, Scott J, Novicoff W, Cui Q. Systematic review of the etiology behind patellar clunk syndrome. World J Orthop 2020; 11(3): 184-196
- URL: https://www.wjgnet.com/2218-5836/full/v11/i3/184.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i3.184
Total knee arthroplasty (TKA) is one of the most successful orthopedic procedures performed today[1-3]. Posterior stabilized TKA has long term survivorship that surpasses 90% at a 10 year minimum follow-up in several studies, but is occasionally complicated by a post-operative pathology called patellar clunk syndrome (PCS)[1]. PCS is an uncommon complication following TKA that was first described by some researcher and is associated almost exclusively associated with posterior stabilized designs[2,3]. It has an estimated incidence of 0% to 20% in all primary total knee replacements, depending on design[4-7]. The symptoms of patellar clunk can range from painless catching of the knee to painful locking, leading to dissatisfaction of the knee replacement[2,3]. With appropriate identification of the problem, this condition can be relatively easy to treat with high levels of satisfaction[8].
PCS typically presents within, on average, the first 7.4 postoperative months[8]. Symptomatic patella clunk is characterized by anterior knee pain secondary to painful locking of the knee when going from full flexion to extension, followed by a painful clunk as the knee fully straightens[3]. The pathoanatomy of patella clunk involves an accumulation of scar tissue along the undersurface of the quadriceps tendon, proximal to the superior pole of the patella and patellar button[2]. As the knee flexes, the patella engages the trochlea of the implant. As the knee then extends, the knot of scar tissue can become trapped in the femoral box, leading to locking of the knee mid-flexion. Additionally, the scar tissue nodule can impinge upon the intercondylar notch, producing pain on extension. Forceful extension of the knee leads to the scar tissue painfully disengaging from the box followed by an audible “clunk” or painful snap, typically visualized at 30-45 degrees from full extension[9].
The diagnosis is one that is made clinically and occasionally via imaging. The patella can be seen catching and releasing as the patient is asked to extend the knee from flexion (video sees https://vimeo.com/148540681). In addition to physical exam and plain radiographs, magnetic resonance imaging and ultrasound can aid in the diagnosis and help guide treatment. magnetic resonance imaging has been used to demonstrate a fibrous soft tissue nodule proximal to the patella in 75% (9/12) of patients with suspected patellar clunk[10]. Plain radiographs can also help with the identification of any loose bodies causing crepitus, and evaluate the position of the patellar component. Ultrasound imaging has also been used in the evaluation and diagnosis of PCS[11].
Under the PICOS algorithm, we conducted a systematic review and meta-analysis of articles published on PCS after TKA to (1) characterize the etiology of PCS; (2) understand the outcomes and prevention of PCS; (3) clarify strengths and weaknesses of the current evidence; and (4) outline guidelines for future research.
For the systematic review, we used the following inclusion criteria: (1) All patients were above 18 years of age; (2) TKA as a primary procedure; and (3) PCS incidence was evaluated as an outcome. These studies were restricted according to the following study characteristics: (1) English language only; and (2) Original research. Exclusion criteria were review articles, studies less than 5 participants, double publication of data. We did not include a date limitation as we wanted to survey the comprehensive breadth of existing PCS literature rather than confine our search to modern, contemporary PCS literature.
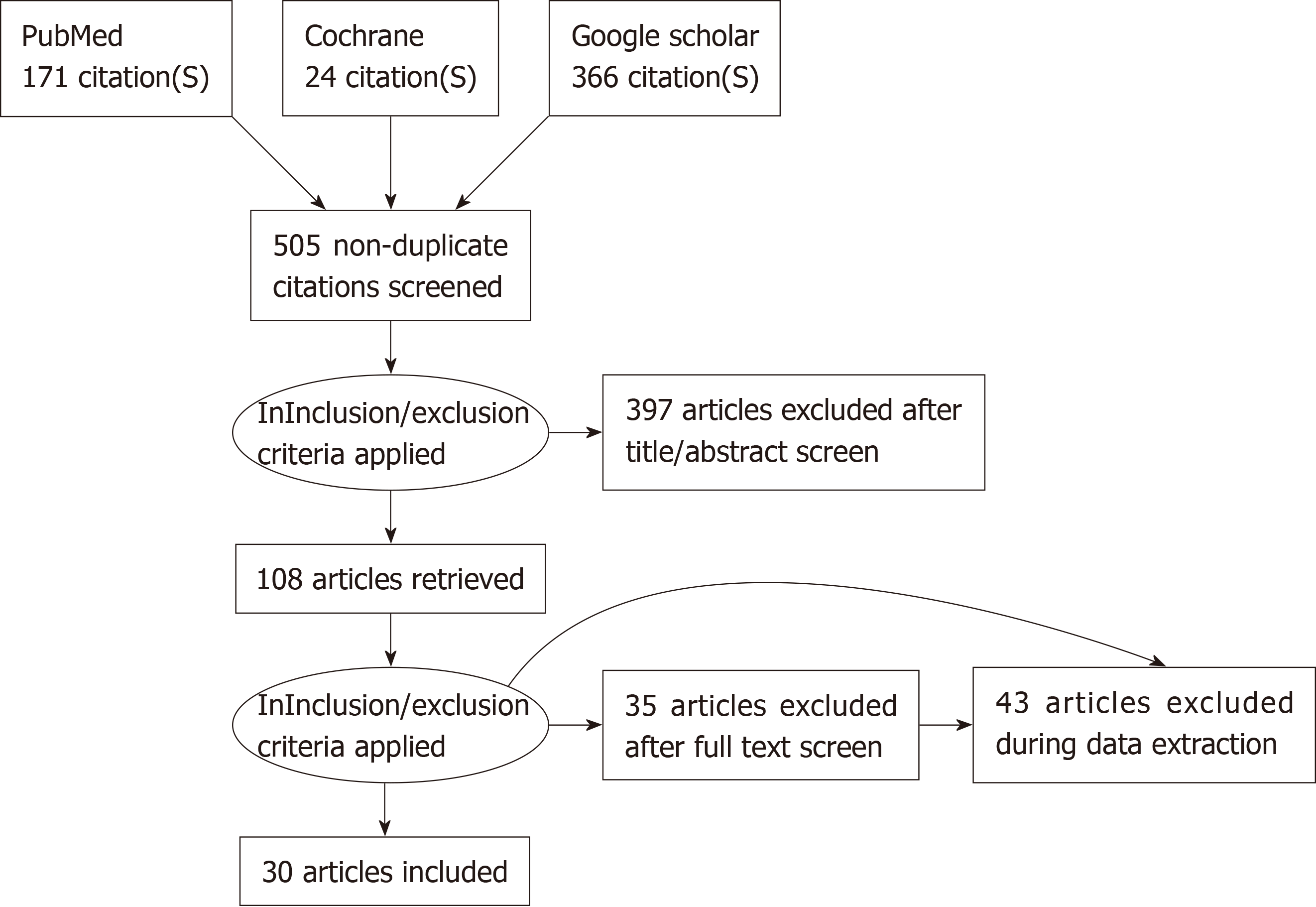
Our literature search strategy included PubMed (MEDLINE), Google Scholar, and Cochrane for peer-reviewed full-length articles on PCS. The last search was performed in July, 2018. On-line literature search was conducted using MeSH keyword search on PubMed (MEDLINE), Google Scholar, and Cochrane “(patella OR patellar) AND (clunk OR catch OR crepitation)”. We also used the “relevant articles” feature to locate any potentially relevant studies. Using this search technique resulted in 505 non-duplicated articles (Figure 1).
Following the research, two reviewers (SBS and QC) independently reviewed all articles to evaluate their contribution to this study using the aforementioned eligibility criteria. We then excluded any articles not relevant to the characterization of PCS based upon their content. Using eligibility criteria, we obtained 30 articles (Table 1, 1-30). Two articles were excluded because they were not in English. If necessary information was not specified in the abstract, an additional screen was executed after data collection to evaluate the study’s contribution to this investigation. We obtained the full text if at least one of the reviewers judged a study to be eligible. We reviewed reference lists of included studies to identify additional studies. Reference lists yielded 3 additional studies (Table 1, 31-33). Definitions of pertinent metrics were compiled in Table 2. Disagreements on inclusion were resolved by consensus. Neither reviewer was blinded to any study characteristics including journal, contributing authors, or affiliated institution (Figure 2).
| Ref. | Postope-rative Knee Flexion (degrees) | Prothes-es Design | Joint Line Level | Patellar Height | Insall- Salvati Ratio | Position of Tibial Tray | Patellar thickne-ss | Patellar tendon length | Femoral condyle offset | Patellar tilt | Posterior tibial slope | Resurfac-ing |
| Beight et al[40] | Not significant | N/A | Significant | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Anderson et al[22] | N/A | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Significant | N/A | N/A |
| Pollock et al[20] | N/A | Significant | Not significant | Not significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Maloney et al[27] | N/A | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Yau et al[15] | N/A | N/A | Not significant | Significant | Significant | Significant | N/A | N/A | N/A | Significant | N/A | N/A |
| Ip et al[23] | N/A | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Schroer et al[28] | Significant | Significant | N/A | Not significant | Not significant | N/A | N/A | N/A | N/A | Not significant | Not significant | N/A |
| Fukunaga et al[14] | Significant | Significant | N/A | Not significant | Not significant | Not significant | N/A | N/A | N/A | Significant | N/A | N/A |
| Dennis et al[5] | Not significant | N/A | Not significant | Significant | Significant | Significant | N/A | Significant | Significant | Not significant | Not significant | N/A |
| Frye et al[4] | Significant | Significant | Not significant | Not significant | Not significant | N/A | N/A | N/A | N/A | Significant | N/A | N/A |
| Choi et al[8] | Not significant | Significant | Not significant | N/A | Not significant | N/A | Not significant | N/A | Not significant | Not significant | Not significant | Significant |
| Costanzo et al[1] | N/A | N/A | N/A | Not significant | N/A | N/A | Significant | N/A | Significant | N/A | N/A | N/A |
| Gholson et al[32] | Not significant | N/A | Not significant | Not significant | Not significant | Not significant | Not significant | Not significant | Not significant | Not significant | Significant | N/A |
| Peralta-Molero et al[29] | Significant | N/A | Not significant | Not significant | Not significant | Not significant | Not significant | N/A | N/A | Not significant | Not significant | N/A |
| Bae et al[41] | N/A | Significant | Not significant | N/A | Not significant | N/A | N/A | N/A | N/A | Significant | N/A | N/A |
| Toomey et al[42] | N/A | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Martin et al[19] | Significant | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Snir et al[43] | N/A | Significant | N/A | N/A | N/a | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Tang et al[21] | N/A | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/a | N/A | N/A | N/A |
| Rajshekha-r et al[44] | N/A | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/a | N/A | N/A |
| Figgie et al[9] | N/A | N/A | Significant | Significant | N/A | Significant | N/A | N/A | N/A | N/A | N/A | N/A |
| Ip et al[45] | N/A | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Lonner et al[17] | N/A | Significant | Not significant | N/A | Not significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Shoji et al[25] | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Not significant |
| Ogawa et al[34] | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Significant | N/A | Significant |
| Hamilton et al[31] | N/A | N/A | N/A | N/A | N/A | N/A | Significant | N/A | N/A | N/A | N/A | N/A |
| Martin et al[19] | Significant | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Agarwala et al[2] | N/A | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Shilling-ton et al[33] | N/A | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Significant |
| McNabb et al[46] | N/A | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Clarke et al[18] | N/A | Significant | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Ranawat et al[26] | N/A | Significant | N/A | Not significant | Not significant | N/A | Not significant | N/A | N/A | N/A | N/A | N/A |
| Aglietti et al[16] | Not significant | Significant | N/A | Not significant | N/A | N/A | N/A | N/A | N/A | Not significant | N/A | Significant |
| Postoperative knee flexion | After surgery, the degree to which the knee can flex |
| Prosthesis design | Several prosthesis designs can be implanted in a TKA |
| Joint line height | Shortest distance between the fibular head and lateral femoral condyle on AP radiograph |
| Patellar height | Measured as the perpendicular distance from the inferior pole of the patellar implant to the joint line of the prosthesis |
| Insall-Salvati ratio | Ratio of the length of the patellar tendon to the length of the patella |
| Position of tibial tray | Measured as the perpendicular distance of the tibial tray from the patellar tendon |
| Patella thickness | The width of the patella (medial to lateral) |
| Patellar tendon length | Length of the patellar tendon superior to inferior |
| Posterior tibial slope | The degree to which the tibia is lateral to the perpendicular line drawn from the prosthesis |
| Patellar tilt | Angle subtended by the equatorial line of the patella and the line connecting the anterior limits of the femoral condyles |
| Femoral condyle offset | Distance between the lateral condyle and the vertical line parallel to the lateral edge of the femur |
Once studies were chosen, one reviewer (SBS) went through each article independently and consolidated the data in Table 1. Study quality was evaluated using sample size, study design, follow-up consistency, and analysis methods. Three other reviewers (QC, WN, JS) verified the data collection and consolidation independently. Data was collected on May 18th, 2018.
The risk of bias in the selection of individual studies for inclusion in this investigation was assessed by qualitative review initially based upon study quality and availability of existing studies pertaining to PCS from Table 1. After data consolidation, individual studies were evaluated through ROBIS, the risk of bias assessment tool for systematic reviews. Results indicate that this systematic review has a low risk of bias (Table 3)[12].
| Study eligibility criteria | Identification and selection of studies | Data collection and study appraisal | Synthesis findings | Risk of bias in the review | |
| PCS etiology | Yes | Yes | Yes | Yes | A. Yes |
| Systematic review | B. Yes | ||||
| C. No | |||||
| Overall: Low |
The search for studies on factors that influence incidence of PCS post-TKA yielded 861 citations; after screening for duplicates, 505 citations were included. After inclusion and exclusion criteria were applied to abstracts, 397 articles were excluded from the review. 108 full-length manuscripts were obtained, at which point inclusion and exclusion criteria were applied, yielding 30 total articles for the review. Each reference list of the final 30 articles were reviewed for robust inclusion of pertinent literature which yielded an additional three articles. The pertinent findings, as they apply to this systematic review, of these 33 manuscripts are found in Table 1. Risk of bias was performed using the ROBIS tool and the results indicated that the techniques and results of the literature search qualified for a low risk of bias (Table 3).
The abundance of scar tissue that forms on the undersurface of the quadriceps tendon leading to PCS is due to several factors (Table 1). Originally, theories suggested it was due to inadequate resection of synovium at the time of total knee arthroplasty[2,3]. However, there is no data to support this as a leading cause. Other etiologies include components of the native knee and prosthesis like femoral component design, joint line level and postoperative patellar positioning, but generally most researchers have concluded that the pathogenesis of PCS is multifactorial[5,6,8]. Dennis et al[5] notes that risk factors for PCS include shortened patellar length, smaller patellar components, decreased patellar composite thickness, increased patellar offset, smaller and flexed femoral components, and thicker tibial polyethylene inserts. In fact, Hoops et al[6] employed a control-matched computational model to evaluate tendo-femoral contact in patients with posterior-stabilized TKA. Using this model, the authors confirmed clinical findings that an increased patellar ligament length, flexed femoral component, lowered joint line, and larger patellar component all reduced the problematic contact near the intercondylar notch. The most significant contributing factor to tendo-femoral contact was found to be patellar ligament length. Decreasing patellar ligament length by two standard deviations (13 mm) away from the normal resulted in a large increase in contact area with intercondylar notch. Preexisting patella baja, as confirmed by preoperative radiographs, may also increase the risk of postoperative PCS[9].
Surgeons can correct for this by reducing distal femoral resection, which will decrease the tibial bearing thickness required to adequately tension the extension gap and effectively lower the joint line and decrease patella baja. Figgie et al[9] reported that a joint line level of 8 mm or less, a patellar height of 10 to 30 mm, and a neutral/posterior placement of the tibial prosthesis oriented to the center line of the tibia should result in improved outcome and reduced PCS incidence[9,13]. However, these three aforementioned conditions are only sufficient to reduce PCS, not eliminate it[10]. Similar to patellar height, a reduced patellar tendon length also predisposes an individual to PCS, most likely since the reduction in either metric will increase the contact between the quadriceps tendon and the superior intercondylar notch[4]. As such, most studies that concluded patellar height is correlated with PCS would also concomitantly conclude patellar tendon length has the same relationship with PCS. Measurements such as the Insall-Salvati ratio and the location of the tibial tray may induce or prevent the incidence of PCS post-TKA. The Insall-Salvati ratio is defined as the ratio of the patella tendon length to the length of the actual patella. As such, an Insall-Salvati ratio below 0.8 is considered “patellar baja”, whereas above 1.2 is considered patellar alta. Studies have demonstrated that low Insall-Salvati ratios are contributory towards post-operative PCS (Table 1). Similarly, if the tibial tray is placed too anteriorly with respect to the tibia’s center line, PCS is more likely to occur[13,14]. Yau et al[15] determined that PCS inflicted knees had a relative position of 7.74 mm with respect to the patellar tendon as compared to 9.23 mm non-PCS inflicted knees, indicating that a neutral or posterior positioning of the tibial tray may aid in the reduction of PCS.
Certain total knee designs appear more susceptible than others to PCS, most likely due to their underlying differences in metrics (Table 2). First generation Insall-Burnstein prostheses have been adapted to decrease the incidence of PCS by resurfacing the patella and smoothened anterior edge to the trochlea[16]. Even so, the Insall-Burnstein II generated PCS in 4% of treated knees as compared to 0% by the fixed NexGen Legacy Posterior-Stabilized flex design[17]. The NextGen Legacy moved the cam and post mechanism such that the trochlea would have more mobility and oriented the patellar groove obliquely, resulting in minimal to no PCS[18]. Others found the incidence of PCS to be higher (P < 0.001) in patients with the mobile Press-Fit Condylar Sigma Rotating Platform/RotatingPlatform-Flex Knee System (11 of 113 knees, 9.7%), compared to fixed NexGen Legacy Posterior Stabilized-Flex design (6 of 424 knees, 1.4%)[8]. The mobile Press-Fit Condylar has a larger intercondylar box ratio which is more likely to induce the fibrous nodule near the patella, resulting in PCS. The Attune prosthesis also demonstrated low incidence of PCS and is therefore a viable alternative to earlier generations since its smaller anterior flange and concomitant intercondylar box ratio cause less clunk[19].
Furthermore, Pollock et al[20] and Agarwala et al[2] concluded that a significantly higher (P < 0.001) proportion of high-flex mobile bearing joints (15%) compared to fixed bearing joints (0%) develop PCS. Additionally, the incidence of PCS in Anatomic Modular Knee Congruency implant, Anatomic Modular Knee-Posterior Stabilized implants and Press Fit Condylar Sigma-Posterior Stabilized implant was 13.5%, 3.8%, and 0%, respectively, indicating that a proximally positioned or wider femoral box is more likely to induce PCS[20]. Yau et al[15] 2003 determined a significant incidence of PCS (18.3%) when using the AMK posterior stabilized knee potentially due to a shallow femoral trochlea and more proximal and narrower intercondylar notch. Due to the lack of a femoral box needed to accommodate the cam and post mechanism for a posterior stabilized design, cruciate retaining designs are typically not affected by this condition with the exception of a few reports[18,21-23]. Posterior femoral condyle offset may also be partially responsible for an increased incidence of PCS. Gopinathan suggests that such increasing condyle offset may cause an anterior shift of the intercondylar box and cause the intercondylar box to come into contact with the quadriceps tendon[13].
In recent years, the dimensions of the intercondylar box has been implicated in a host of PCS studies as contributory towards the development of PCS. For example, first generation PS designs’ high transition zone from trochlear groove to intercondylar box induced an apposition of the quadriceps tendon to the intercondylar box[9]. As such, post-operative complications such as synovial hyperplasia and patellar clunk and crepitus (PCC) would arise. Second and third generation PS designs attempted to corrected for the large intercondylar box. Frye et al[4] demonstrated that PCS or patella- femoral crepitation was evident in 12% of their 108 patients with a conventional, first- generation design, compared to no complication in the second-generation design with a deeper trochlear groove and smooth transition of the intercondylar box (0/136, P < 0.0001). Fukunaga et al[14] described this difference as the intercondylar box ratio, which is the intercondylar box height versus the anterior-posterior height of the femoral component. Studies suggest that an intercondylar box ratio less than 0.7 has, so far, shown elimination of PCS[24]. Anatomically, the smaller intercondylar box ratio decreases the likelihood the proximal pole of the patella will come into contact with the anterior edge of the intercondylar box during flexion[25]. In addition to the intercondylar box ratio, the medial-lateral geometry of the intercondylar box itself has also been implicated in PCS. Pollock et al[20] determined that the PFC Sigma PS prostheses was more efficient than the AMK Congruency and AMK PS in reducing the width of the intercondylar box and therefore PCS. Similarly, Ranawat et al[26] concluded that by smoothening the sharp ridge of the intercondylar groove while maintaining a 0.85-0.87 intercondylar box ratio, PCS incidence could be reduced to 2%.
Another important component associated with PCS incidence is the degree of the patient’s knee flexion. Some studies on PCS have also evaluated the extent of knee flexion and concluded that each additional degree of knee flexion increased the chance of PCS by 4.2%[26]. Maloney et al[27] capitalized on this association between knee flexion and PCS, stating that this ‘hyperflexion’ leads to the quadriceps tendon being perturbed as it inserts on the patella and the development of the pathognomonic fibrous nodule near the patellar button.
In a study conducted by Schroer et al[28] with 747 TKA, the degree of postoperative knee flexion was significantly associated with the development of patella clunk. The utilization of a Vanguard PS femoral component (which is narrower and has a rounded intercondylar notch transition than the Ascent), eliminated PCS even when using the MIS technique, as compared to the Ascent femoral component and the MIS technique. Mean knee flexion at six weeks postoperatively in patients who developed patella clunk was 124 degrees versus 117 for the knees that did not develop PCS (P = 0.016). They hypothesized that the increased postoperative knee flexion furthered the distance between the patella and femoral component, causing the soft tissue entrapment near the intercondylar notch. More recently, Peralta-Molero et al[29] reviewed 570 primary TKAs using the Genesis II SPC TKA system with 6% of knees developing PCS. The authors found that the likelihood of developing PCS increased by 4.2% with each degree of increased flexion. Other literature that studied Attune posterior-stabilized prosthesis demonstrated a lower incidence of PCS and lower postoperative knee flexion as compared to PFC sigma prosthesis[19]. However, other studies have shown postoperative knee flexion to be an insignificant risk factor in the development of PCS (Table 1)[5,8].
Patellar thickness has also been implicated in the development of PCS. Thinner components have been shown to increase the incidence of PCS by reducing the offset of the quadriceps tendon from the superior portion of the trochlear groove[30]. Additionally, Costanzo et al[1]. determined that patella thickness, preoperatively, does relate to increased incidence of PCS and suggested that it may lead to greater bone/soft tissue resectioning, though this risk factor can be mitigated by improved surgical technique[1]. Hamilton et al[31] demonstrated this significant association by demonstrating an increase in PCS with thinner patellas in 3655 TKAs. In fact, decreasing the thickness by more than 2 mm would increase the risk of developing PCS by 2.5, owing to a smaller distance between the extensor mechanism and femoral component box. The importance of patella thickness is not well understood, however, as several other studies have concluded that patella thickness has minimal association with the incidence of PCS (Table 1)[8,26,29,32].
Increased posterior tibial slope has also been thought to contribute to the development of PCS, most notably since an increase in the flexion gap would increase the level of tension placed on upon the quad mechanism. However, aside from Gholson et al[32], no other study has found a significant correlation between this metric and PCS incidence.
Patellar tilt, defined as the angle subtended by the equatorial line of the patella and the line connecting the anterior limits of the femoral condyles, has also been implicated in the development of PCS[14,15]. Fukunaga et al[14], using logistic regression analysis, determined that incidence of PCS would increase 1.27 for every degree increase in patellar tilt. The prosthesis design is also thought to impact the stability of patellar tracking and therefore can influence PCS development[15].
The relationship between patellar resurfacing and incidence of PCS has not been definitely confirmed in the literature. For example, Shoji et al[25] concluded that in a series of 647 TKAs, there was no difference in incidence of PCS between the patellar resurfaced group and native patella group. Still, some orthopedists recommend patellar resurfacing to reduce PCS due to its ability to create more space between the patella and the femoral box[33]. Ogawa et al[34] studied 84 knees from 69 patients and concluded that PCS was significantly higher in native patellas, owing to the increased patellar tilt and medial positioning of the patella to the femur in resurfaced patellas. While patellar resurfacing/retention was found to significantly increase the incidence of PCS (4/14 vs 56/752 in non-PCS group, P = 0.003), this study only included 14 knees that were resurfaced as compared to 752 that were not resurfaced[8].
Once a diagnosis of patella clunk is established, it can be effectively treated. Since mechanical catching of scar tissue causes pain, non-surgical means are not the most successful at treating the condition. That being said, before surgical intervention, conventional non-surgical intervention is limited to lower extremity quadriceps and hamstring strengthening[1-4].
In surgery, typically the lesion is debrided arthroscopically without needing to open the knee joint. The patient is set up as usual for knee arthroscopy. The patient is placed supine on the operating table without breaking the foot of the bed. A side post or leg holder is not necessary, and a tourniquet may be used at the discretion of the surgeon. The knee is approached with a superolateral inflow/viewing portal, where the undersurface of the quad tendon can be inspected, as well as the patella directly viewed engaging the trochlea. The offending lesion is typically identified as a mass of scar tissue proximal to the superior pole of the patella, near the patellar button. A superomedial working portal is then made under direct visualization via outside-in technique. The synovium and scar can then be debrided with a motorized shaver, taking care to not damage the prosthetic surfaces or underlying quadriceps tendon. Once a thorough debridement has been completed, the knee is then drained of fluid and taken through a range of motion to ensure there are no further mechanical blocks to extension. The knee is wrapped in an ace bandage and allowed to engage in full activity post-op (video sees https://vimeo.com/148540681).
Messieh[35] described surgical treatment of PCS using a limited open arthrotomy under local anesthesia in two patients. The benefits included subjective improved patient satisfaction with patient’s ability to actively move the knee during debridement to ensure adequate resection of the nodule and minimal knee swelling associated with arthroscopic distension leading to faster recovery. This, however, is not the standard of care treatment in PCS, and most patients would prefer to be under general or spinal anesthesia. It is however an option for patients with contraindications to general anesthesia.
Sekiya et al[36] described a more recent surgical intervention for PCS using the conventional arthroscopic debridement procedure to excise the offending fibrous nodule. In 46 separate generally anesthetized patients, anterolateral, anteromedial, and proximal superomedial portals were set up, with the first used as the viewing portal. After the working probe was inserted into the anteromedial compartment, an electric shaver was used to remove any scar tissue on the medial or lateral tibiofemoral joint, patellofemoral joint, intercondylar notch, or posterior aspect of the infrapatellar fat pad. One day post-operation, the patient was allowed to bear full weight.
Arthroscopic treatment of PCS generally has high patient satisfaction rates and improvement of pain and function following surgery for patella clunk. Dajani et al[3] reported on 15 patients with symptomatic patellar clunk treated with arthroscopic debridement. Of this series, there was a significant reduction of pain from 6 to 1 in the immediate post-operative period. At an average of 41 months follow-up (range, 24-75 mo), average Knee Society Score (KSS) increased from 76 to 92, and KSS function increased from 71 to 79. Koh et al[37], also reported a positive response to arthroscopic debridement. Twelve knees were reported with minimum one year follow-up. Average KSS increased from 63.8 to 90.9, with KSS function increasing from 65.4 to 90.4. Of note, there was no significant improvement in rising from a chair or stair climbing in patients with patellar clunk treated with arthroscopic synovectomy. Gholson et al[32] performed a similar study in which they scrutinized the work of one surgeon and concluded that KSS improved to 92.4 and WOMAC to 82.9. All patients in the study were at least moderately satisfied; however, 17% required a repeat arthroscopic debridement, after which, there were no further complications of PCS. Occasionally, arthroscopic debridement to eliminate PCS may not return the patient to normal range of motion. A recent study suggested that even post-PCS, patients can still suffer from PCS; for example, a case of prosthetic loosening of the femoral component, caused noticeable gait disturbance post-PCS[36]. Such a post-operative complication necessitated additional prosthesis revision surgery, after which no complications or symptoms manifested two years thereafter.
Main prevention methods include utilization of femoral components with reduced intercondylar box ratio (such that the trochlear groove is more distal and posterior), avoidance of patella baja, proper surgical technique during TKA with prevention of patella over-resection, and debridement of fibrosynovial tissue at time of TKA[29].
Additionally, by initiating the entry site for the intramedullary distal femoral cutting guide jig more anteriorly, a surgeon can prevent femoral component flexion which may ultimately lead to the fibrous nodule ‘catching’ on extension from a flexed position. Yau et al[15] additionally mentions that excessive surgical trauma and failure to debride the suprapatellar synovium may be an important, but not underlying etiology of the fibrosis in PCS. Therefore, careful surgical technique to avoid excessive trauma and synovial disruption can reduce the possibility of PCS. Fukunaga et al[14] concluded that a femoral component design that includes a raised lateral flange, deepened trochlear groove, and side-specific femoral components can help reduce, but not eliminate, PCS. While posterior-stabilized TKA has been associated with a higher incidence of PCS, both cruciate retaining and substituting TKA should not necessarily be deemed preventative of PCS.
According to Yau et al[15], the neutral or posterior arrangement of the tibial tray may reduce the incidence of PCS as well. Perhaps most logically, the attempted reduction in etiology of PCS should reduce the incidence of the post-operative complication. Conrad et al[38] advised surgeons to avoid overresection of the patella which was then corroborated by Meftah et al[30] who found a reduction of PCS incidence from 40% to 21% by avoiding over-resection and reducing the quantity of components in the patellofemoral joint. Conrad et al[38] also reports that the excision of the fibrosynovial tissue at the superior pole of the patella may also reduce the chance that the same tissue catches when moving from knee flexion to extension – however, as previously noted, this is controversial.
Finally, some evidence suggests that resurfacing of the patella can decrease and prevent the development of PCS. Through resurfacing, the patella will be less likely to come into contact with the proximal edge of the femoral box[33].
This study comprehensively reviews the existing literature on the etiology of PCS. To our knowledge, there are no systematic reviews under PRISMA guidelines that seek to determine the etiology of PCS making this study unique in its approach and conclusions. However, this study does have its limitations. This systematic review used three large databases to extract literature from, though some suggest the use of EMBASE and Web of Science in addition to Google Scholar, MEDLINE, and Cochrane for comprehensive, yet efficient review of the literature[39]. Furthermore, while the ROBIS risk bias assessment tool yielded a low risk of bias, the use of statistical significance in the results of the included literature presents some degree of bias within the conclusions of this systematic review (Table 3).
The literature on the development of PCS presents limitations in terms of pure analysis of etiology and general heterogeneity. Many studies were constructed to evaluate prosthesis design on complication rate and prognosis post-TKA, though only included PCS as a small subset of a series of post-TKA complications. As a result, it is unclear the degree to which these studies emphasized and scrutinized the incidence of PCS as compared to overall outcome following TKA. Additionally, studies on the etiology of PCS are heavily biased towards the study of prosthesis design. While prosthesis design is the product of the more fundamental parameters of Table 1, these studies did not examine the effect of those fundamental parameters on the incidence of PCS. Without isolating each individual parameter, reviews of the current evidence will be limited as it will be difficult to determine if multiple, one or none of the parameters are responsible for the development of PCS.
Patella clunk is an uncommon complication following total knee arthroplasty with a posterior stabilized design. Herein, we have determined that the formation of patellar clunk has a multifactorial etiology, including postoperative knee flexion, joint line level, prosthesis design, patella thickness, tibial tray positioning, patellar tilt, Insall-Salvati ratio, femoral condyle offset, and posterior tibial slope. In spite of a multifactorial etiology, the treatment is relatively straightforward and can provide the patient a high satisfaction rate postoperatively. While diagnosed clinically, any painful total knee replacement should be thoroughly worked up for other causes of pain, including infection, trauma, loosening and instability. Further studies should aim at examining isolated parameters that characterize prosthesis design to more specifically understand what parameters of prosthesis design contribute to development of PCS.
Patellar clunk syndrome (PCS) is a postoperative complication following total knee arthroplasty that clinically presents as anterior knee pain that is particularly painful when going from full flexion to extension. The pathoanatomy of PCS involves the accumulation of scar tissue along the undersurface of the quadriceps tendon, proximal to the superior pole of the patella. The diagnosis of PCS can often be made clinically, but radiographic adjuncts such as ultrasound and magnetic resonance imaging have been used with success. Unfortunately, there is no current literature that evaluates multiple metrics of the native knee and prosthesis to determine what metric is most responsible for the development of PCS.
The main topics of the current study are (1) characterizing and analyzing metrics implicated in the pathogenesis of PCS; and (2) defining contemporary management, treatment, and preventative algorithms for PCS. The current study aims to elucidate how various prosthesis and geometries of native knee can cause PCS or prevent it from occurring, which are poorly summarized and defined in the literature currently.
The main objective of the current study is to evaluate current evidence and characterize a reasonable etiology for the development of PCS. A secondary objective of the current study is to better understand the various treatment and preventative heuristics implemented to manage PCS.
A systematic review of clinical research studies from PubMed, Google Scholar, and Cochrane was conducted, as these databases were felt to be representative of peer-reviewed scholarly work and well encompassed literature surrounding PCS. Each study was analyzed and results were compiled in designated tables with a predetermined list of metrics and its corresponding incidence of PCS. Details regarding prevention, treatment, and management were also extracted at this time.
A total of 30 articles were identified through the primary search, with an additional 3 included from reference lists of the primary search. Results indicate that prosthesis design was the most frequently cited metric as contributory towards PCS. The prosthesis design is often a combination of multiple metrics and, therefore, we conclude that the etiology of PCS is multifactorial. A reduced intercondylar box ratio and box width has been consistently shown to reduce PCS.
Prosthesis design is the main metric associated with the etiology of PCS, though because the prosthesis design incorporates several other metrics included in our analysis, the etiology of PCS is multifactorial. Later prosthesis designs that incorporate a reduced intercondylar box ratio and box width can reduce development of PCS. Preventative strategies involve using later generations of prosthesis especially those that incorporate a reduced intercondylar box ratio.
Overall, this study was able to confirm the etiology of PCS as well as provide insight into treatment methods to prevent this postoperative complication. Nevertheless, future studies should aim to isolate individual metrics of prosthesis design to more specifically determine which metric is most responsible for the development of PCS. Higher level randomized control trials should also be conducted to generate additional evidence to improve knee maneuverability and function post-total knee arthroplasty.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Emara KM, Tangtrakulwanich B S-Editor: Ma YJ L-Editor: A E-Editor: Liu MY
| 1. | Costanzo JA, Aynardi MC, Peters JD, Kopolovich DM, Purtill JJ. Patellar clunk syndrome after total knee arthroplasty; risk factors and functional outcomes of arthroscopic treatment. J Arthroplasty. 2014;29:201-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Agarwala SR, Mohrir GS, Patel AG. Patellar clunk syndrome in a current high flexion total knee design. J Arthroplasty. 2013;28:1846-1850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Dajani KA, Stuart MJ, Dahm DL, Levy BA. Arthroscopic treatment of patellar clunk and synovial hyperplasia after total knee arthroplasty. J Arthroplasty. 2010;25:97-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Frye BM, Floyd MW, Pham DC, Feldman JJ, Hamlin BR. Effect of femoral component design on patellofemoral crepitance and patella clunk syndrome after posterior-stabilized total knee arthroplasty. J Arthroplasty. 2012;27:1166-1170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Dennis DA, Kim RH, Johnson DR, Springer BD, Fehring TK, Sharma A. The John Insall Award: control-matched evaluation of painful patellar Crepitus after total knee arthroplasty. Clin Orthop Relat Res. 2011;469:10-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Hoops HE, Johnson DR, Kim RH, Dennis DA, Baldwin MA, Fitzpatrick CK, Laz PJ, Rullkoetter PJ. Control-matched computational evaluation of tendo-femoral contact in patients with posterior-stabilized total knee arthroplasty. J Orthop Res. 2012;30:1355-1361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Mauerhan DR. Fracture of the polyethylene tibial post in a posterior cruciate-substituting total knee arthroplasty mimicking patellar clunk syndrome: a report of 5 cases. J Arthroplasty. 2003;18:942-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 59] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Choi WC, Ryu KJ, Lee S, Seong SC, Lee MC. Painful patellar clunk or crepitation of contemporary knee prostheses. Clin Orthop Relat Res. 2013;471:1512-1522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Figgie HE 3rd, Goldberg VM, Heiple KG, Moller HS, Gordon NH. The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Joint Surg Am. 1986;68:1035-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 417] [Cited by in RCA: 351] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 10. | Hozack WJ, Rothman RH, Booth RE, Balderston RA. The patellar clunk syndrome. A complication of posterior stabilized total knee arthroplasty. Clin Orthop Relat Res. 1989;(241):203-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Geannette C, Miller T, Saboeiro G, Parks M. Sonographic evaluation of patellar clunk syndrome following total knee arthroplasty. J Clin Ultrasound. 2017;45:105-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, Davies P, Kleijnen J, Churchill R; ROBIS group. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 718] [Cited by in RCA: 1304] [Article Influence: 130.4] [Reference Citation Analysis (0)] |
| 13. | Gopinathan P. Patello-femoral clunk syndrome-current concepts. J Orthop. 2014;11:55-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Fukunaga K, Kobayashi A, Minoda Y, Iwaki H, Hashimoto Y, Takaoka K. The incidence of the patellar clunk syndrome in a recently designed mobile-bearing posteriorly stabilised total knee replacement. J Bone Joint Surg Br. 2009;91:463-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Yau WP, Wong JW, Chiu KY, Ng TP, Tang WM. Patellar clunk syndrome after posterior stabilized total knee arthroplasty. J Arthroplasty. 2003;18:1023-1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 49] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Aglietti P, Baldini A, Buzzi R, Indelli PF. Patella resurfacing in total knee replacement: functional evaluation and complications. Knee Surg Sports Traumatol Arthrosc. 2001;9 Suppl 1:S27-S33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Lonner JH, Jasko JG, Bezwada HP, Nazarian DG, Booth RE. Incidence of patellar clunk with a modern posterior-stabilized knee design. Am J Orthop (Belle Mead NJ). 2007;36:550-553. [PubMed] |
| 18. | Clarke HD, Fuchs R, Scuderi GR, Mills EL, Scott WN, Insall JN. The influence of femoral component design in the elimination of patellar clunk in posterior-stabilized total knee arthroplasty. J Arthroplasty. 2006;21:167-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Martin JR, Jennings JM, Watters TS, Levy DL, McNabb DC, Dennis DA. Femoral Implant Design Modification Decreases the Incidence of Patellar Crepitus in Total Knee Arthroplasty. J Arthroplasty. 2017;32:1310-1313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 20. | Pollock DC, Ammeen DJ, Engh GA. Synovial entrapment: a complication of posterior stabilized total knee arthroplasty. J Bone Joint Surg Am. 2002;84:2174-2178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 41] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Tang YH, Wong WK, Wong HL. Patellar clunk syndrome in fixed-bearing posterior-stabilised versus cruciate-substituting prostheses. J Orthop Surg (Hong Kong). 2014;22:80-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Anderson JA, Baldini A, Sculco TP. Patellofemoral function after total knee arthroplasty: a comparison of 2 posterior-stabilized designs. J Knee Surg. 2008;21:91-96. [PubMed] [DOI] [Full Text] |
| 23. | Ip D, Ko PS, Lee OB, Wu WC, Lam JJ. Natural history and pathogenesis of the patella clunk syndrome. Arch Orthop Trauma Surg. 2004;124:597-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Niikura T, Tsumura N, Tsujimoto K, Yoshiya S, Kurosaka M, Shiba R. Patellar clunk syndrome after TKA with cruciate retaining design: a report of two cases. Orthopedics. 2008;31:90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 25. | Shoji H, Shimozaki E. Patellar clunk syndrome in total knee arthroplasty without patellar resurfacing. J Arthroplasty. 1996;11:198-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 30] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Ranawat AS, Ranawat CS, Slamin JE, Dennis DA. Patellar crepitation in the P.F.C. sigma total knee system. Orthopedics. 2006;29:S68-S70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 27. | Maloney WJ, Schmidt R, Sculco TP. Femoral component design and patellar clunk syndrome. Clin Orthop Relat Res. 2003;(410):199-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Schroer WC, Diesfeld PJ, Reedy ME, LeMarr A. Association of increased knee flexion and patella clunk syndrome after mini-subvastus total knee arthroplasty. J Arthroplasty. 2009;24:281-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Peralta-Molero JV, Gladnick BP, Lee Y, Ferrer AV, Lyman S, González Della Valle A. Patellofemoral Crepitation and Clunk Following Modern, Fixed-Bearing Total Knee Arthroplasty. J Arthroplasty. 2014;29:535-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Meftah M, Ranawat AS, Ranawat CS. The natural history of anterior knee pain in 2 posterior-stabilized, modular total knee arthroplasty designs. J Arthroplasty. 2011;26:1145-1148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 31. | Hamilton WG, Ammeen DJ, Parks NL, Goyal N, Engh GA, Engh CA. Patellar Cut and Composite Thickness: The Influence on Postoperative Motion and Complications in Total Knee Arthroplasty. J Arthroplasty. 2017;32:1803-1807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 32. | Gholson JJ, Goetz DD, Westermann RW, Hart J, Callaghan JJ. Management of Painful Patellar Clunk and Crepitance: Results at a Mean Follow-Up of Five Years. Iowa Orthop J. 2017;37:171-175. [PubMed] |
| 33. | Shillington M, Farmer G. Patellofemoral crepitus following lcs rps total knee arthroplasty without patella resurfacing. Orthop Proceedings. 2012;94-B:19-19. |
| 34. | Ogawa H, Matsumoto K, Akiyama H. Effect of Patellar Resurfacing on Patellofemoral Crepitus in Posterior-Stabilized Total Knee Arthroplasty. J Arthroplasty. 2016;31:1792-1796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 35. | Messieh M. Management of patellar clunk under local anesthesia. J Arthroplasty. 1996;11:202-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 36. | Sekiya H, Takatoku K, Takada H, Kanaya Y, Sasanuma H. Painful knee after total knee arthroplasty is not a frequent complication and could be treated by arthroscopic debridement. Orthop Proceedings. 2016;98-B:152-152. |
| 37. | Koh YG, Kim SJ, Chun YM, Kim YC, Park YS. Arthroscopic treatment of patellofemoral soft tissue impingement after posterior stabilized total knee arthroplasty. Knee. 2008;15:36-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 38. | Conrad DN, Dennis DA. Patellofemoral crepitus after total knee arthroplasty: etiology and preventive measures. Clin Orthop Surg. 2014;6:9-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 39. | Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. 2017;6:245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 867] [Cited by in RCA: 915] [Article Influence: 114.4] [Reference Citation Analysis (0)] |
| 40. | Beight JL, Yao B, Hozack WJ, Hearn SL, Booth RE. The patellar "clunk" syndrome after posterior stabilized total knee arthroplasty. Clin Orthop Relat Res. 1994;(299):139-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 41. | Bae DK, Baek JH, Yoon KT, Son HS, Song SJ. Comparison of patellofemoral outcomes after TKA using two prostheses with different patellofemoral design features. Knee Surg Sports Traumatol Arthrosc. 2017;25:3747-3754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 42. | Toomey SD, Daccach JA, Shah JC, Himden SE, Lesko JP, Hamilton WG. Comparative Incidence of Patellofemoral Complications Between 2 Total Knee Arthroplasty Systems in a Multicenter, Prospective Clinical Study. J Arthroplasty. 2017;32:S187-S192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 43. | Snir N, Schwarzkopf R, Diskin B, Takemoto R, Hamula M, Meere PA. Incidence of patellar clunk syndrome in fixed versus high-flex mobile bearing posterior-stabilized total knee arthroplasty. J Arthroplasty. 2014;29:2021-2024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 44. | Rajshekhar KT, Kumar MN, Venugopal P, Chandy T. Patellar clunk in total knee arthroplasty using modified Sigma posterior stabilized femoral component. J Clin Orthop Trauma. 2014;5:211-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 45. | Ip D, Wu WC, Tsang WL. Comparison of two total knee prostheses on the incidence of patella clunk syndrome. Int Orthop. 2002;26:48-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 46. | McNabb DC, Dennis DA, Jennings JM, Daines B, Laz P, Kim RH. Implant Design and Effects on Patellofemoral Crepitus. J Knee Surg. 2017;30:863-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |