Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastrointest Pathophysiol. Aug 15, 2014; 5(3): 304-321
Published online Aug 15, 2014. doi: 10.4291/wjgp.v5.i3.304
Published online Aug 15, 2014. doi: 10.4291/wjgp.v5.i3.304
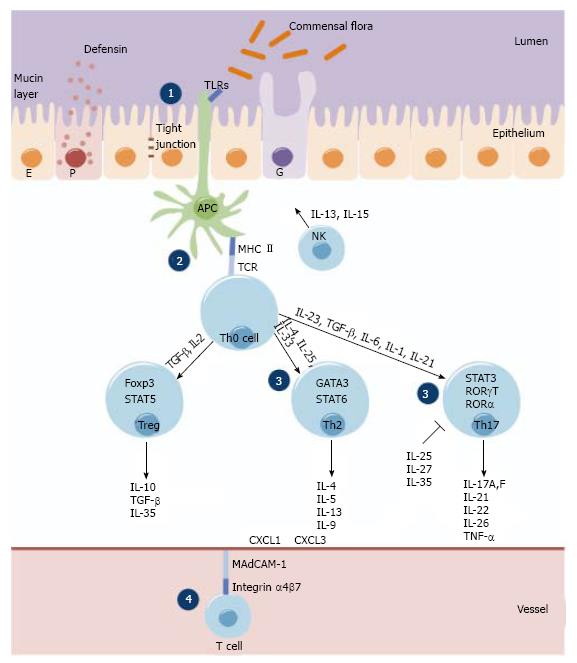
Figure 1 The Ulcerative colitis-associated risk loci.
Damage of the epithelial barrier (E), the mucinous biofilm layer secreted from goblet cells (G), the antibacterial peptides (e.g., defensines) produced by Paneth cells (P) and the tight junctions leads to increased permeability in ulcerative colitis (UC). Antigen presenting cells (APCs) (i.e., macrophages and dendritic cells) in the lamina propria are increased in absolute number in UC, they bind microbial products through detection molecules of the innate immune system, including Toll like receptors (TLRs) on the cell surface and on the cytoplasmatic NOD-like receptors (NLRs). Stimulation of these receptors induces intracellular signaling cascades, resulting in secretion of large number of cytokines, chemokines, and immunomodulatory factors. The development of the Th2, Th17 and Treg subsets from naïve, Th0 cells during primary immune response is mainly determined by cytokines and chemokines, and is under the control of certain transcription factors: T-bet (T-box expressed in T cells), GATA3 (GATA binding protein), RORγt (retinoid-related orphan receptor γt), RORα, STATs (signal transducer and activator of transcription) and FoxP3 (forkhead box P3). Leukocyte migration and recruitment from vessels is mediated by selectins, integrins, ICAMs and chemokines (i.e., c-c motif chemokine ligand, CXCL). The UC-associated loci encode genes involved in: (1) maintenance of epithelial barrier integrity (e.g., ECM1, CDH1, HNF4A, LAMB1, PTGER4, SLC22A4/SLC22A5, MYO9B, MDR1); (2) antigen pattern recognition (e.g., NLRs, TLRs); (3) innate and adaptive immunological responses (e.g., IL-23R, IL-12B, TNFα, IL10R, JAK2, STAT3, HLA-region); and (4) leukocyte recruitment (integrin α4β7, ICAM-1, MAdCAM-1, CXCLs, CCRs).
- Citation: Sarlos P, Kovesdi E, Magyari L, Banfai Z, Szabo A, Javorhazy A, Melegh B. Genetic update on inflammatory factors in ulcerative colitis: Review of the current literature. World J Gastrointest Pathophysiol 2014; 5(3): 304-321
- URL: https://www.wjgnet.com/2150-5330/full/v5/i3/304.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v5.i3.304