Peer-review started: October 15, 2014
First decision: December 17, 2014
Revised: December 25, 2014
Accepted: January 18, 2015
Article in press: January 20, 2015
Published online: February 28, 2015
AIM: To compare time average maximum mean velocity (TAMV) and peak systolic velocity (PSV) criteria of Trans Cranial Doppler (TCD) in their ability to predict abnormalities on magnetic resonance imaging (MRI)/magnetic resonance angiogram (MRA) in patients with sickle cell disease.
METHODS: A retrospective evaluation was performed of the outcomes in all patients with a Transcranial Doppler examination at our institution since the implementation of the hospital picture archiving and communication system (PACS) system in January 2003 through December 2012. All ultrasound imaging exams were performed by the same technologist with a 3 MHz transducer. Inclusion criteria was based upon the Transcranial Doppler procedure code in our PACS which had an indication of sickle cell disease in the history. The patient’s age and gender along with the vessel with the highest time averaged mean velocity as well as the highest peak systolic velocity was recorded for analysis. A subset of the study cohort also had subsequent MR imaging and Angiograms performed within 6 mo of the TCD examination. MRI results were categorized as having a disease related abnormality (vessel narrowing, collateral formation/moya-moya, or abnormal fluid attenuation inversion recovery signal in parenchyma indicative of prior stroke) or normal. The MRI results formed the comparison standards for TCD exams in evaluating intracranial injury. Sensitivity and specificity for the two TCD criteria (TAMV and PSV) were calculated to determine which could be a better predictor for intracranial vasculopathy /clinically occult strokes.
RESULTS: The study cohort for our institution was 110 patients with a total of 291 TCD examinations. These patients had a mean age of 7.6 years with a range from 2-18 years of age. Sixty-two of the 110 patients (56%) had two or more TCD exams. Thirty-seven patients (34%) had at least one MRI following a TCD examination. Of the 291 TCD examinations, 46 (16%) were conditional or abnormal by TAMV criteria. One hundred and sixteen (40%) were conditional or abnormal by PSV criteria. All studies that were abnormal by TAMV were also abnormal by PSV criteria. Seventy of the 116 (60%) studies which were conditional or abnormal by peak systolic criteria would not have been identified by time averaged mean maximum velocity criteria. The most frequent location of highest velocity measurement was noted to be in the middle cerebral artery regardless of whether it was measured by PSV or TAMV. From the 37 patients having one or more MRIs, 43 MRI exams were performed within 6 mo of a TCD examination. Twenty two (51%) MRIs had a disease related abnormality reported. When evaluating conditional or abnormal exams by PSV criteria against follow-up MRI/MRA, the sensitivity was 73% [16/(16 + 6)] and specificity was 81% [17/(4 + 17)]. When evaluating conditional or abnormal exams by TAMV criteria by follow-up MRI/MRA as the gold standard, the sensitivity was 41% [9/(9 + 13)] and the specificity was 100% [21/(21 + 0)]. In using conditional or abnormal criteria from PSV and TAMV to predict abnormalities on follow-up MRI/MR Angiogram, PSV was more sensitive (73% vs 41%) while TAMV was more specific (100% vs 81%).
CONCLUSION: Based on the data obtained at our institution and using the assumption that the best screening test is the one with the highest sensitivity, the peak systolic velocity could be the measurement of choice for TCD screening.
Core tip: To the best of our knowledge, there has been no direct comparison between peak systolic velocity and time average maximum mean velocity in their ability to predict abnormalities on magnetic resonance imaging (MRI)/magnetic resonance angiogram in children with sickle cell disease. With the growing clinical use of MR Angiography to assess sickle cell patients, the sensitivity of Trans Cranial Doppler (TCD) should be maximized if it is to maintain its role as a screening test in the sickle cell population. Based on the data obtained at our institution and using the assumption that the best screening test is the one with the highest sensitivity, the peak systolic velocity could be the measurement of choice for TCD screening.
- Citation: Naffaa LN, Tandon YK, Irani N. Transcranial Doppler screening in sickle cell disease: The implications of using peak systolic criteria. World J Radiol 2015; 7(2): 52-56
- URL: https://www.wjgnet.com/1949-8470/full/v7/i2/52.htm
- DOI: https://dx.doi.org/10.4329/wjr.v7.i2.52
Over the past 20 years, there has been a significant increase in understanding the cerebrovascular consequences of sickle cell disease. Without treatment, 11% of children with sickle cell disease will have an ischemic stroke by 20 years of age[1]. It is also well documented that children with an ischemic stroke are at high risk for recurrence unless treated with repeated transfusions with a goal of maintaining the level of sickle hemoglobin below 30%[2]. By treating the patients with abnormal time average maximum mean velocity (TAMV) with transfusion, the 10% per year risk of stroke is reduced to less than 1%[3].
The Stroke Prevention Trial in Sickle Cell Anemia (STOP) was a significant advance in screening for this complication of sickle cell disease as it demonstrated the efficacy of Trans Cranial Doppler (TCD) in identifying patients at high risk for ischemic brain injury. The trial involved correlating the TAMV in the internal carotid artery (ICA) and proximal middle cerebral artery (MCA) on an annual Doppler waveform tracing with the clinical outcome of stroke. A TAMV of 200 cm/s was indicative of a 10% stroke risk over the ensuing year, while a level of 170 cm/s was considered conditional, requiring shorter interval follow-up[3].
The thresholds that carried forward into the STOP trial grew from a post hoc analysis of potential cutoff values for TAMV which looked to minimize false positives and yield the highest relative risk. The analysis did not maximize sensitivity as would be assumed if the intent were to utilize this test to screen asymptomatic patients with sickle cell disease. This fundamental oversight in selecting the TAMV criteria ultimately undercuts TCD’s potential as a screening test. The reference standard in evaluating thresholds in the 1992 analysis was cerebral angiography and not MRI; the latter is now the current standard of care for stroke detection. Indeed, in many centers, MRI is now ordered more frequently than TCD for sickle cell patients as reporting of TCD results based upon TAMV criteria do not satisfy the criteria of an optimal screening test. If we look back at the original data, the highest sensitivity for patients with stroke was not at 170 cm/s, but rather, at a much lower level of 140 cm/s. A final consideration in how this cutoff determination process ultimately limits TCD’s applicability is the relatively small cohort of seven patients with clinically evident stroke that was included in the original analysis[4].
In 2005, the results from the STOP trial were revisited to determine if another, equally predictive, criterion for clinically apparent stroke could be found for TCD with imaging acquisition (the more common TCD method utilized in practice for sickle cell patients). Peak systolic velocity (PSV) was one of the measures evaluated as it has long been a metric for determining stenosis in other important vascular distributions[5]. A comparison of PSV and TAMV revealed that the PSV appeared to predict stroke as well as TAMV albeit with different velocity cutoffs. From this analysis, came the recommendation of using a PSV of 250 cm/s being as abnormal (high risk) and a PSV of 200 cm/s or greater considered conditional requiring increased surveillance[6].
Following this analysis, there are now two possible criteria (PSV and TAMV) which validated against the same data set, as being equally predictive of a clinically apparent stroke. In practice, it would seem that the sensitivity of the TCD evaluation in predicting the more proximate cause of sickle cell stroke (intracranial vasculopathy) should depend upon which of these criteria were utilized to identify “normal”. To our knowledge, there has been no comparison of these two criteria in their ability to predict abnormalities on MRI/MRA.
With the growing clinical use of magnetic resonance imaging (MRI)/magnetic resonance angiogram (MRA) to assess sickle cell patients, the sensitivity of TCD should be maximized if it is to maintain its role as a screening test in the sickle cell population. Our retrospective analysis of eight years of TCD data at our institution aims to provide this correlation.
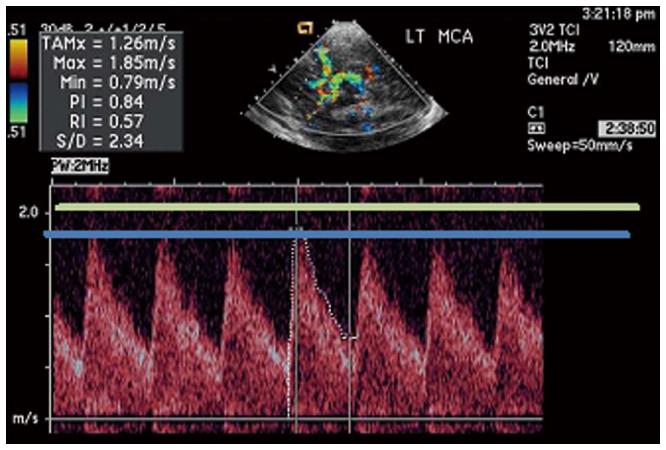
Our Institutional Review Board approved a retrospective evaluation of the outcomes in all patients with a Transcranial Doppler examination at our institution since the implementation of the hospital PACS system in January 2003 through December 2012. All ultrasound imaging exams were performed by the same technologist with a 3 MHz transducer. Inclusion criteria was based upon the Transcranial Doppler procedure code in our PACS which had an indication of sickle cell disease in the history. Indications other than sickle cell disease were excluded (e.g., ancillary brain death evaluation, vasospasm). The patient age and gender along with the vessel with the highest time averaged mean velocity as well as the highest peak systolic velocity was recorded for analysis (Figure 1).
A subset of the study cohort also had subsequent MR imaging and Angiograms performed within 6 mo of the TCD examination on a 1.5 Tesla MRI. MRI results were categorized as having a disease related abnormality (vessel narrowing, collateral formation/moya-moya, or abnormal fluid attenuation inversion recovery signal in parenchyma indicative of prior stroke) or normal. The MRI results formed the comparison standards for TCD exams in evaluating intracranial injury.
Sensitivity and specificity for the two TCD criteria (TAMV and PSV) were calculated to determine which could be a better predictor for intracranial vasculopathy /clinically occult strokes.
The statistics were reviewed and analyzed by the authors. Determinations of sensitivity and specificity were made based upon data collected and public domain information. No biostatistician was involved with this project due to resource constraints.
The study cohort for our institution was 110 patients with a total of 291 TCD examinations. These patients had a mean age of 7.6 years with a range from 2-18 years of age. Sixty-two of the 110 patients (56%) had two or more TCD exams. Thirty-seven patients (34%) had at least one MRI following a TCD examination. The subset of patients with an MRI exam following the TCD exam had a higher age, as expected, with a mean of 8.6 years with a range of 3-18 years.
Of the 291 TCD examinations, 46 (16%) were conditional or abnormal by TAMV criteria. One hundred and sixteen (40%) were conditional or abnormal by PSV criteria. All studies that were abnormal by TAMV were also abnormal by PSV criteria. Seventy of the 116 (60%) studies which were conditional or abnormal by peak systolic criteria would not have been identified by time averaged mean maximum velocity criteria.
The most frequent location of highest velocity measurement was noted to be in the MCA regardless of whether it was measured by PSV or TAMV. This accounted for over 80% of all exams during our study period. For TAMV measurement, the ACA demonstrated the highest velocity in 19% of exams. The highest PSV was found in the ACA in 16% of exams. One exam demonstrated the highest velocity within the PCA, although the TAMV and PSV were both less than 100 cm/s. No exams (using either criteria) found the highest velocity to be within the ICA.
From the 37 patients having one or more MRIs, 43 MRI exams were performed within 6 mo of a TCD examination. Twenty two (51%) MRIs had a disease related abnormality reported. When evaluating conditional or abnormal exams by PSV criteria against follow-up MRI/MRA (Table 1), the sensitivity was 73% [16/(16 + 6)] and specificity was 81% [17/(4 + 17)]. When evaluating conditional or abnormal exams by TAMV criteria by follow-up MRI/MRA as the gold standard (Table 2), the sensitivity was 41% [9/(9 + 9 + 13)] and the specificity was 100% [21/(21 + 0)]. In using conditional or abnormal criteria from PSV and TAMV to predict abnormalities on follow-up MRI/MR Angiogram, PSV was more sensitive (73% vs 41%) while TAMV was more specific (100% vs 81%).
| MRI/MRA | |||
| Condition/abnormal | Normal | ||
| Peak systolic criteria | Conditional/abnormal | 16 | 4 |
| Normal | 6 | 17 | |
| MRI/MRA | |||
| Condition/abnormal | Normal | ||
| Mean velocity criteria | Conditional/abnormal | 9 | 0 |
| Normal | 13 | 21 | |
Since the original STOP trial publication, there has been a significant increase in utilization of TCD with imaging in asymptomatic sickle cell patients to identify increased stroke risk[7]. A finding of elevated velocities requires further monitoring or transfusion intervention. The use of TCD in this manner is that of a screening test. A good screening test is one with maximum sensitivity, so that if the test is negative, the condition is not present. In this case, the condition was “clinically evident stroke”. The threshold for TCD velocities was set in the STOP trial to detect 97% of all patients with clinically evident stroke. The trial did not measure TCD sensitivity against the presence or progression of intracranial vasculopathy, which is a more proximate cause of stroke in these patients. While nearly all patients with an abnormal TCD by STOP criteria will have vasculopathy, not all patients with vasculopathy will have an abnormal TCD by the STOP TAMV criteria.
It has been further documented that clinically silent strokes in sickle cell patients with normal neurologic and TCD exam are detectable by MR Imaging[8]. This observation is also concordant with data indicating that patients with silent infarcts on MRI and normal TCD results by the original STOP criteria are more than twice as likely as the unscreened sickle cell population to develop a clinically apparent stroke[9]. Indeed, even though patients with abnormalities only on MRI frequently have a “normal” neurologic exam, it is becoming more apparent that neuropsychological deficits exist[10].
In order for TCD screening to maintain its role as an adequate screening test, it must perform close to the level of MRI at least in predicting the presence or progression of intracranial vasculopathy. To this purpose, a number of studies have compared TCD velocity measurements with the presence of stenosis at MR Angiography. Lowering the TAMV threshold to 165 cm/s could yield a sensitivity of 92% in predicting stenosis on MRI[11]. Adult studies, however, indicate that the threshold for TAMV would have to be set at 123 cm/s for 100% sensitivity[12].
The restricted availability of the exam with only a single trained technologist ensured uniformity throughout the study period. The limitations of our study include the small sample size given the relative underutilization of sickle cell services and difficulty of follow-up. While the ultrasound technical exam factors remain well controlled, variations in MRI technique over the 10-year time period could have influenced uniformity of the gold standard. We also did not have the ability to correlate clinical outcomes given the relatively recent transition to an electronic medical record (2010) at our institution. A larger prospective study with the ability to correlate TCD TAMV, PSV, MRI and MRA findings, neuropsychological exam results, and clinically apparent stroke could provide a useful follow-up to the STOP trial to update best practice recommendations for what is one of the leading causes of stroke in pediatric patients.
Based on the data obtained at our institution and using the assumption that the best screening test is the one with the highest sensitivity, the peak systolic velocity could be the measurement of choice for TCD screening. A more specific test with MRI or neuropsychological evaluation should follow in those patients who may have suffered clinically silent ischemic brain injury.
Without treatment, 11% of children with sickle cell disease will have an ischemic stroke by 20 years of age. Trans Cranial Doppler (TCD) is used as a screening test to prevent this complication in the sickle cell population. A finding of elevated velocities requires further monitoring or transfusion intervention. Velocities can be measured using the time average maximum mean velocity (TAMV) or the peak systolic velocity (PSV) criteria.
With the growing clinical use of magnetic resonance imaging (MRI)/magnetic resonance angiogram (MRA) to assess sickle cell patients, the sensitivity of TCD should be maximized if it is to maintain its role as a screening test in the sickle cell population.
To the best of our knowledge, there has been no comparison of PSV and TAMV criteria in their ability to predict abnormalities on MRI/MRA.
Based on the data obtained at our institution and using the assumption that the best screening test is the one with the highest sensitivity, the peak systolic velocity could be the measurement of choice for TCD screening.
The STOP trial is the acronym for Stroke Prevention Trial in Sickle Cell Anemia. It was a significant advance in screening for the complication of ischemic stroke in sickle cell disease as it demonstrated the efficacy of TCD in identifying patients at high risk for ischemic brain injury.
It is a very good article.
P- Reviewer: Al-Haggar M S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Ohene-Frempong K, Weiner SJ, Sleeper LA, Miller ST, Embury S, Moohr JW, Wethers DL, Pegelow CH, Gill FM. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood. 1998;91:288-294. [PubMed] [Cited in This Article: ] |
| 2. | Pegelow CH, Adams RJ, McKie V, Abboud M, Berman B, Miller ST, Olivieri N, Vichinsky E, Wang W, Brambilla D. Risk of recurrent stroke in patients with sickle cell disease treated with erythrocyte transfusions. J Pediatr. 1995;126:896-899. [PubMed] [Cited in This Article: ] |
| 3. | Adams RJ, McKie VC, Hsu L, Files B, Vichinsky E, Pegelow C, Abboud M, Gallagher D, Kutlar A, Nichols FT. Prevention of a first stroke by transfusions in children with sickle cell anemia and abnormal results on transcranial Doppler ultrasonography. N Engl J Med. 1998;339:5-11. [PubMed] [Cited in This Article: ] |
| 4. | Adams R, McKie V, Nichols F, Carl E, Zhang DL, McKie K, Figueroa R, Litaker M, Thompson W, Hess D. The use of transcranial ultrasonography to predict stroke in sickle cell disease. N Engl J Med. 1992;326:605-610. [PubMed] [Cited in This Article: ] |
| 5. | Alexandrov AV, Brodie DS, McLean A, Hamilton P, Murphy J, Burns PN. Correlation of peak systolic velocity and angiographic measurement of carotid stenosis revisited. Stroke. 1997;28:339-342. [PubMed] [Cited in This Article: ] |
| 6. | Jones A, Granger S, Brambilla D, Gallagher D, Vichinsky E, Woods G, Berman B, Roach S, Nichols F, Adams RJ. Can peak systolic velocities be used for prediction of stroke in sickle cell anemia? Pediatr Radiol. 2005;35:66-72. [PubMed] [Cited in This Article: ] |
| 7. | Armstrong-Wells J, Grimes B, Sidney S, Kronish D, Shiboski SC, Adams RJ, Fullerton HJ. Utilization of TCD screening for primary stroke prevention in children with sickle cell disease. Neurology. 2009;72:1316-1321. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Siegel MJ, Luker GD, Glauser TA, DeBaun MR. Cerebral infarction in sickle cell disease: transcranial Doppler US versus neurologic examination. Radiology. 1995;197:191-194. [PubMed] [Cited in This Article: ] |
| 9. | Pegelow CH, Macklin EA, Moser FG, Wang WC, Bello JA, Miller ST, Vichinsky EP, DeBaun MR, Guarini L, Zimmerman RA. Longitudinal changes in brain magnetic resonance imaging findings in children with sickle cell disease. Blood. 2002;99:3014-3018. [PubMed] [Cited in This Article: ] |
| 10. | Platt OS. Prevention and management of stroke in sickle cell anemia. Hematology Am Soc Hematol Educ Program. 2006;Abstract:54-57. [PubMed] [Cited in This Article: ] |
| 11. | Arkuszewski M, Krejza J, Chen R, Kwiatkowski JL, Ichord R, Zimmerman R, Ohene-Frempong K, Melhem ER. Sickle cell disease in children: accuracy of imaging transcranial Doppler ultrasonography in detection of intracranial arterial stenosis. Neuroradiol J. 2012;25:402-410. [PubMed] [Cited in This Article: ] |