Published online Mar 28, 2024. doi: 10.4329/wjr.v16.i3.49
Peer-review started: November 20, 2023
First decision: December 19, 2023
Revised: January 18, 2024
Accepted: March 12, 2024
Article in press: March 12, 2024
Published online: March 28, 2024
Ureteropelvic junction obstruction (UPJO) is a common congenital urinary tract disorder in children. It can be diagnosed as early as in utero due to the presence of hydronephrosis or later in life due to symptomatic occurrence.
To evaluate the discrepancy between dynamic contrast-enhanced magnetic resonance urography (dMRU) and scintigraphy 99m-technetium mercaptoacetyltriglycine (MAG-3) for the functional evaluation of UPJO.
Between 2016 and 2020, 126 patients with UPJO underwent surgery at Robert Debré Hospital. Of these, 83 received a prenatal diagnosis, and 43 were diagnosed during childhood. Four of the 126 patients underwent surgery based on the clinical situation and postnatal ultrasound findings without undergoing functional imaging evaluation. Split renal function was evaluated preoperatively using scintigraphy MAG-3 (n = 28), dMRU (n = 53), or both (n = 40). In this study, we included patients who underwent surgery for UPJO and scintigraphy MAG-3 + dMRU but excluded those who underwent only scintigraphy MAG-3 or dMRU. The patients were divided into groups A (< 10% discrepancy) and B (> 10% discrepancy). We examined the discrepancy in split renal function between the two modalities and investigated the possible risk factors.
The split renal function between the two kidneys was compared in 40 patients (28 boys and 12 girls) using scintigraphy MAG-3 and dMRU. Differential renal function, as determined using both modalities, showed a difference of < 10% in 31 children and > 10% in 9 children. Calculation of the relative renal function using dMRU revealed an excellent correlation coefficient with renal scintigraphy MAG-3 for both kidneys.
Our findings demonstrated that dMRU is equivalent to scintigraphy MAG-3 for evaluating split renal function in patients with UPJO.
Core Tip: This study aimed to evaluate the discrepancy between dynamic contrast-enhanced magnetic resonance urography (MRU) and scintigraphy 99m-technetium mercaptoacetyltriglycine (MAG-3) in the functional evaluation of ureteropelvic junction obstruction (UPJO). The results show that dynamic contrast-enhanced MRU is equivalent to scintigraphy MAG-3 for evaluating split renal function in cases of UPJO in all pediatric age groups. Moreover, it is safe and accurate and does not require ionizing radiation.
- Citation: Al-Shaqsi Y, Peycelon M, Paye-Jaouen A, Carricaburu E, Tanase A, Grapin-Dagorno C, El-Ghoneimi A. Evaluating pediatric ureteropelvic junction obstruction: Dynamic magnetic resonance urography vs renal scintigraphy 99m-technetium mercaptoacetyltriglycine. World J Radiol 2024; 16(3): 49-57
- URL: https://www.wjgnet.com/1949-8470/full/v16/i3/49.htm
- DOI: https://dx.doi.org/10.4329/wjr.v16.i3.49
Ureteropelvic junction obstruction (UPJO), the most common urinary tract disorder among children, is observed in all pediatric age groups[1,2]. It can be diagnosed during the neonatal period due to the presence of prenatal dilation of the upper urinary tract or later in life due to symptomatic occurrence. However, most cases are detected during the perinatal period[1,3].
Renal ultrasound is generally used to detect and follow up hydronephrosis, whereas renal scintigraphy using dimercaptosuccinic acid or 99m-technetium mercaptoacetyltriglycine (MAG-3) evaluates renal function and obstruction, respectively[4,5]. Computed tomography can be an option for adolescents and young adults to assess obstruction and identify any aberrant vessels as a cause of UPJO or for postoperative follow-up[4]. Although these techniques can clearly assess obstructions, they cannot predict the progressive loss of renal function or determine which patients will benefit from surgery.
The decision for surgical intervention to correct UPJO is controversial; while some surgeons suggest early intervention, others promote a wait-and-see approach[5,6]. Many urologists follow the sonographic diagnosis of hydronephrotic kidney and use declining renal function in functional imaging studies as an indication for surgery[6]. Asymptomatic patients with UPJO should only be treated if there is evidence of asymmetric function, functional deterioration, or hydronephrosis[4-7]. Identifying and surgically correcting UPJO in these patients before the occurrence of nephron loss is essential.
Renal scintigraphy is considered the gold standard technique for evaluating anatomical obstruction and measuring split renal function in children and adults, driving therapeutic decisions[8-10]. However, dynamic contrast-enhanced magnetic resonance urography (dMRU) has recently been proposed as an alternative technique for evaluating the drainage curve and split renal function in obstructive uropathy, without requiring ionizing radiation[11-13]. The use of dMRU to obtain both anatomical and functional information in a single examination without radiation is beneficial, especially in the follow-up of young patients[14,15].
This study aimed to evaluate the discrepancies between dMRU and renal scintigraphy MAG-3 for the functional evaluation of UPJO in children. We hypothesized that dMRU and renal scintigraphy MAG-3 would provide similar information regarding renal function.
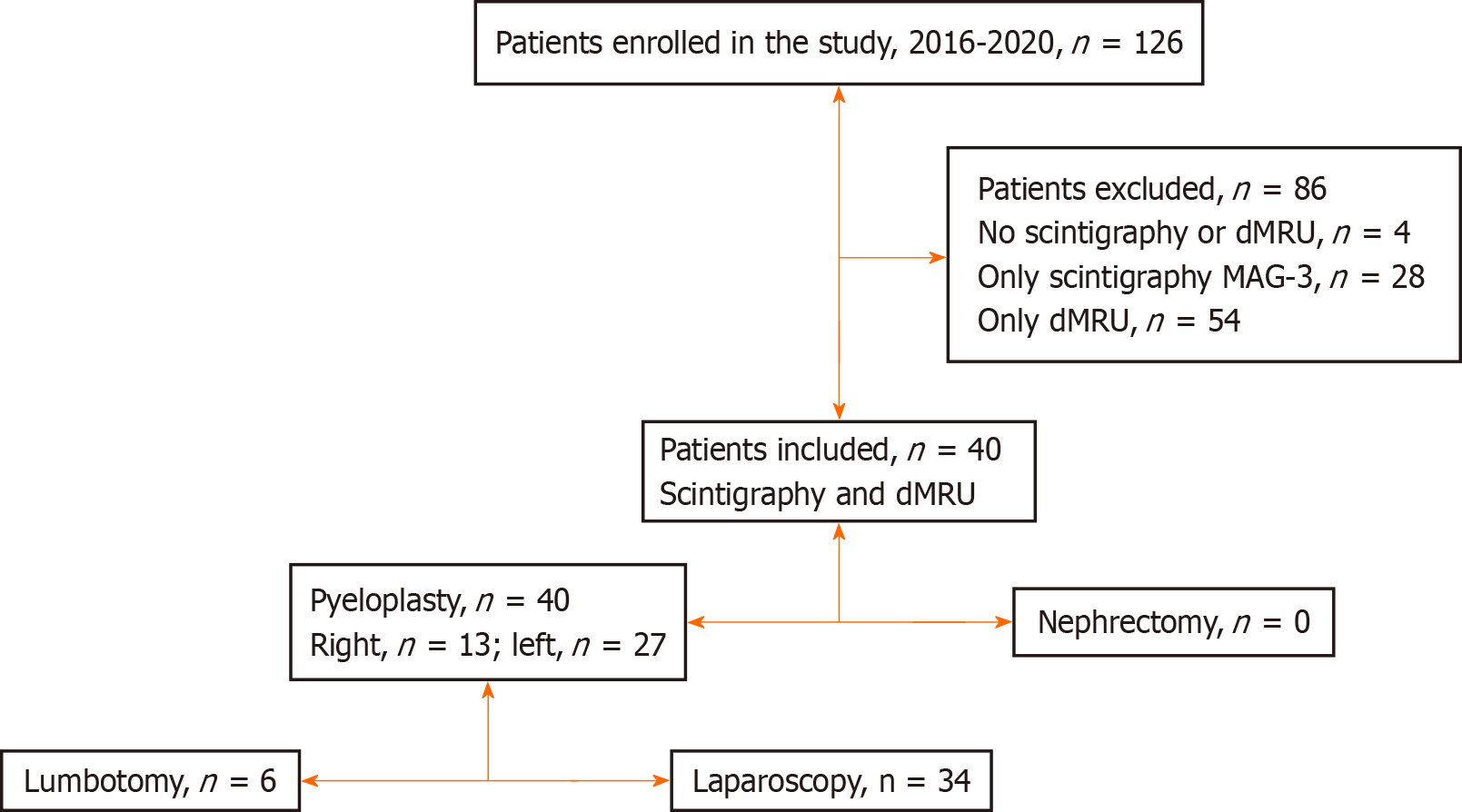
This retrospective cohort study included patients with UPJO who underwent surgery and renal scintigraphy MAG-3 + dMRU at Roberts Debré Children University Hospital between January 2016 and March 2020 but excluded those who underwent only renal scintigraphy MAG-3 or dMRU (Figure 1). This retrospective study was conducted in accordance with the ethical principles outlined in the Helsinki Declaration. Due to the nature of the study involving analysis of de-identified data from existing medical records, formal ethical approval from an institutional review board was not sought. However, efforts were made to ensure patient confidentiality and respect for individual privacy throughout the study process.
First, all patients underwent renal ultrasonography for the initial radiological evaluation of renal pelvic dilatation (Table 1). Those suspected of UPJO were then subjected to further renal function evaluations using scintigraphy MAG-3 or dMRU based on the available modality and the radiologist’s experience. As these patients did not require surgical correction of the UPJO, they were followed up in the clinic with renal ultrasonography. However, in situations where the patients had major dilatation of the renal pelvis on ultrasound findings during follow-up, we requested another modality for comparison i.e., if the patient had initially underwent scintigraphy MAG-3, we requested dMRU, and vice versa (Table 2).
| Entire cohort, n = 126 | Scintigraphy MAG-3 only, n = 28 | DMRU only, n = 54 | Scintigraphy MAG-3 + dMRU, n = 40 | P valuea | |
| Sex | 0.837 | ||||
| M | 88 (70) | 18 (64) | 38(70) | 28 (70) | |
| F | 38 (30) | 10 (36) | 16 (30) | 12 (30) | |
| Age at diagnosis, months | 22 (8-112) | 8 (4-70) | 29 (8-119) | 30 (14-127) | 0.0471 |
| Diagnosis | |||||
| Prenatal | 83 (66) | 18 (64) | 30 (55.5) | 31 (77) | 0.146 |
| Postnatal | 43 (34) | 10 (36) | 24 (44.5) | 9 (21.5) | |
| Associated anomalies | 0.0476 | ||||
| Duplication of urinary system | 3 (2.4) | 0 | 3 (5.5) | 0 | |
| Ureterocele | 0 | 0 | 0 | 0 | |
| Single kidney | 2 (1.6) | 0 | 1 (2) | 1 (2.5) | |
| Horseshoe kidney | 1 (0.8) | 0 | 1 (2) | 0 | |
| Vesicoureteral reflux | 3 (2.4) | 0 | 0 | 3 (7.5) | |
| Pyelonephritis | 21 (17) | 2 (7) | 12 (22) | 7 (17.5) | 0.241 |
| Urinary stones | 3 (2.4) | 1 (4) | 1 (2) | 1 (2.5) | 0.999 |
| Follow-up, months | 11 (3-23) | 8 (3-27) | 11 (4-19) | 12 (5-20) | 0.966 |
| MAG-3 primary, n = 30 (75) | DMRU secondary, n = 30 (75) | DMRU primary, n = 10 (25) | MAG-3 secondary, n = 10 (25) | |
| Affected kidney | 42 (28-48) | 42 (22-50) | 22 (15-40) | 38 (31-45) |
| Age, months | 13 (4-48) | 29 (9-109) | 41 (11-129) | 12 (4-116) |
| Affected renal size, mm | ||||
| RUS | 28 (24-35) | XY | 28.5 (13) | XY |
| MRI | 28 (21-35) | |||
| Before furosemide | 30 (24-38) | 26 (11) | ||
| After furosemide | 30 (17) | |||
| Surgical decision | No | Yes | No | Yes |
We then examined the discrepancies in split renal function assessments between the two radiological modalities. To assess split renal function in both kidneys, functional dMRU results were correlated with the reference standard of MAG-3 scintigraphy. The patients were divided into two groups: Group A, the discrepancy between renal scintigraphy MAG-3 and dMRU was < 10% (n = 31), and Group B, the discrepancy was > 10% (n = 9). In addition, we investigated the potential risk factors for these discrepancies, including sex, age at diagnosis, preoperative febrile urinary tract infection, presence of vesicoureteral reflux, and associated anomalies of the urinary tract, such as duplication of the urinary system, single kidney, and horseshoe kidney (Table 3).
| Scintigraphy MAG-3 + dMRU, n = 40 | Group A < 10% discrepancy, n = 31 | Group B > 10% discrepancy, n = 9 | P valuea | |
| Sex | 0.697 | |||
| M | 28 (70) | 21 (75) | 7 (25) | |
| F | 12 (30) | 10 (83) | 2 (17) | |
| Age at surgery, months | 30 (14-127) | 37 (14-134) | 27 (13-76) | 0.641 |
| Diagnosis | 0.0897 | |||
| Prenatal | 31 (77.5) | 22 (71) | 9 (29) | |
| Postnatal | 9 (22.5) | 9 (29) | 0 | |
| Associated anomalies | 0.999 | |||
| Duplication of urinary system | 0 | 0 | 0 | |
| Ureterocele | 0 | 0 | 0 | |
| Single kidney | 1 (2.5) | 1 (3) | 0 | |
| Horseshoe kidney | 0 | 0 | 0 | |
| Vesicoureteral reflux | 3 (7.5) | 1 (3) | 2 (22) | 0.999 |
| Pyelonephritis | 7 (17.5) | 6 (19) | 1 (11) | 0.999 |
| Urinary stones | 1 (2.5) | 1 (3) | 0 | 0.999 |
| Follow-up, months | 12 (5-20) | 10 (3-16) | 19 (10-26) | 0.05 |
dMRU is performed as an outpatient study or in the day care unit, depending on the child’s age and the need for sedation. Children < 7 years of age required sedation and observation during daycare for a few hours before discharge from the hospital. Chloral hydrate 50–75 mg/kg PO was administered to children < 1 year of age 30–60 min before the procedure and repeated for 30 min if necessary. In older children, we administered intrarectal pentobarbital (5 mg/kg) and alimemazine (2 mg/kg) 1–2 h before the procedure.
Sedation was induced and monitored by a trained pediatric sedation nurse. The patients were continuously monitored for oxygen saturation and pulse rate. All children were hydrated before the study with Ringer’s lactate solution (10 mL/kg) and premedicated with phenobarbitone (5 mg/kg) administered intrarectally 30 min before the procedure. First, T2-weighted imaging sequences [static magnetic resonance urography (MRU)] were performed to evaluate the entire urinary tract system. Next, furosemide (1 mg/kg) was administered intravenously 1 min after the injection of gadolinium-DTPA 0.05 mmol/kg. Then, routine T1 imaging (excretory MRU) of the kidneys, ureters, and bladder was performed 10 min after furosemide injection. Sequential dynamic contrast-enhanced imaging with a time resolution of 15 s was performed using the volumetric gradient echo technique covering the entire urinary tract. This volumetric sequence was repeated continuously for the initial 3 min following a bolus injection of gadolinium-DTPA 0.05 mmol/kg. Datasets were then obtained at 1 min intervals for a total of 20 min. Renal and ureteral transition times were measured, and the split renal function between the two kidneys was calculated using ImageJ software.
A urinary catheter was placed, and the children were orally hydrated with 10–20 mL/kg of water 30–40 min before the study. Posterior dynamic acquisition was performed after intravenous injection of MAG-3 3.7 MBq/kg and furosemide (1 mg/kg). The patients were placed in the supine position with their backs facing the camera. Serial 15–30 s images were acquired for 30–60 min, depending on the technique chosen. In the dynamic renal study, careful evaluation of the parenchymal phase using the Patlak–Rutland method revealed split renal function. Cortical transit time and collection system dilatation were examined during the excretory phase (initial 2–4 min). Baseline images of the diuretic phase were used to assess the diuretic effects.
Descriptive statistics were performed using Fisher’s exact test or the χ2 tests for categorical variables, Student’s t-test for parametric continuous data (presented as mean and standard deviation), and the Mann–Whitney test for nonparametric continuous data [presented as median and interquartile range (IQR)]. A positive correlation coefficient was observed at r > 0. Potential risk factors for discrepancies in renal function between renal scintigraphy MAG-3 and dMRU were analyzed using univariate analysis, with P < 0.05 considered statistically significant. On exploratory analysis, all variables with values of P < 0.20 on univariate analysis were assessed for a possible association with the discrepancy in renal function between renal scintigraphy MAG-3 and dMRU on multivariate Cox regression.
A total of 126 patients were included in the study. Of these patients, 83 were diagnosed prenatally, and 43 (34%) were diagnosed later during childhood (median age, 9 years). Four (3%) of 126 patients underwent surgery based on clinical evaluation and postnatal ultrasound findings, without undergoing any functional imaging evaluation. Split renal function was evaluated preoperatively using an isotope renal scan [n = 28 (22%)], dynamic MRI [n = 54 (43%)], or both [n = 40 (32%)]. The most common presentation of UPJO was prenatal hydronephrosis in 83 (66%) patients, followed by lumbar pain in 22 (17%) and urinary tract infections in 21 (16%) (P > 0.05). Of the 126 patients, 4 (3%) had duplex systems, 1 had UPJO in a horseshoe kidney, 3 (2%) had vesicoureteral reflux, and 3 (3%) had urinary calculi (P < 0.05; Table 1).
Split renal function was compared in 40 patients [28 boys and 12 girls (P > 0.05)] using scintigraphy MAG-3 and dMRU. Of these, 31 (77%) received a prenatal diagnosis, and 9 (23%) were diagnosed during later childhood (P > 0.05). Differential renal function, as determined by scintigraphy MAG-3 and dMRU, differed by < 10% in 31 children and > 10% in 9 children (P > 0.05; Table 3).
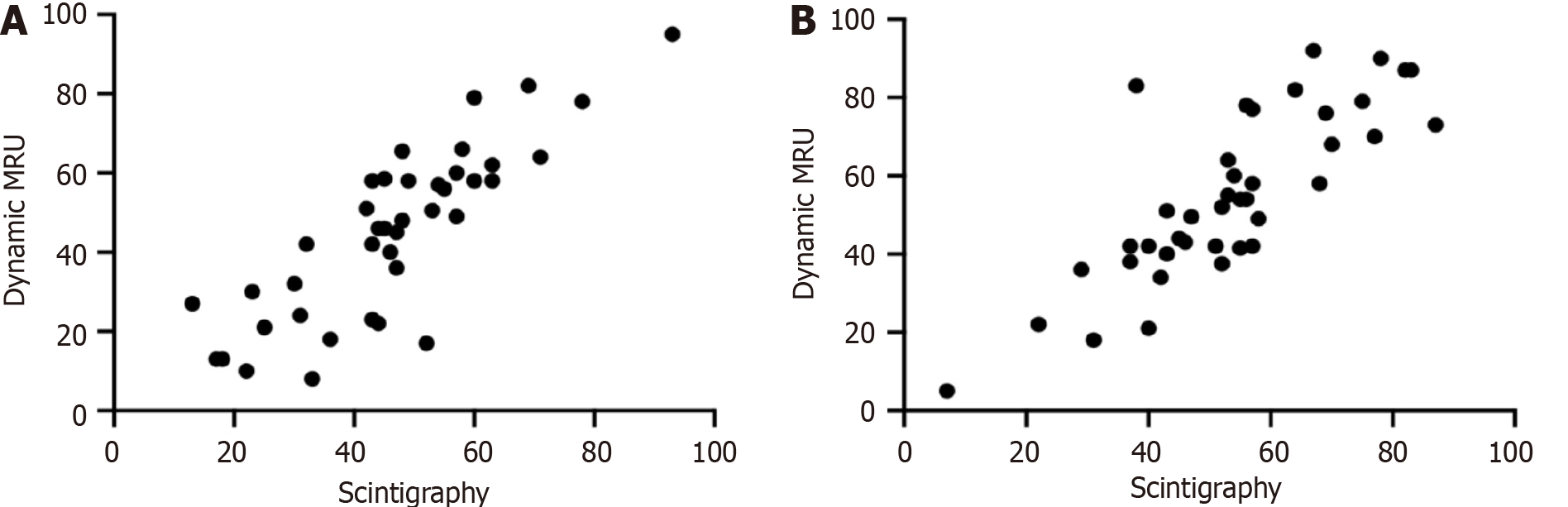
All patients underwent pyeloplasty [right side (n = 13) and left side (n = 27); P > 0.05] at a median age of 30 months (IQR, 14–127 months). Thirty-four patients underwent laparoscopy (retroperitoneoscopy or robot-assisted retroperitoneoscopy) while the other six underwent lumbotomy. Most patients (95%) had good clinical outcomes and satisfactory results on ultrasonography during follow-up [median, 12 months (IQR, 5–20 months)], and there were two cases (5%) of persistent renal pelvic dilatation without renal function degradation. Calculation of relative renal function by dMRU revealed an excellent correlation coefficient with renal scintigraphy MAG-3 for both kidneys (r = 0.84 and r = 0.82, respectively; Figure 2).
Congenital uropathy is a wide-spectrum entity that varies from asymptomatic to self-resolving and life-threatening conditions. Hydronephrosis is the most common congenital anomaly detected using ultrasonography during the prenatal period. While most cases of grade 1 and grade 2 hydronephrosis (96%) spontaneously resolve in the first year of life, a minority of patients develop UPJO[16]. Dynamic renal scintigraphy MAG-3 is considered the gold standard for estimating differential renal function and diagnosing obstructions in children. However, in recent times, dMRU has emerged as an alternative technique for evaluating the drainage curve and split renal function in obstructive uropathy[11-13]. dMRU provides excellent anatomical information on the urinary tract and enables the precise exclusion of urinary tract obstruction, without requiring ionizing radiation[16]. It produces high-resolution images arising from the accumulation of bright contrast content in the collection system and ureter, which enables identification of the ureter distal to the obstruction site[15]. Since 2000, dMRU has been the main modality for evaluating renal function at the Robertson Debré Children University Hospital. However, despite its benefits, dMRU is not widely used because it is expensive and there is a lack of trained pediatric radiologists.
Few studies have investigated the diagnostic value of dMRU for obstructive uropathy. For instance, Perez-Brayfield et al[13] reported that dMRU provides superior anatomical details compared with sonography and nuclear scintigraphy. Although the procedure requires sedation in all cases, it delivers no ionizing radiation to the infant or child. In this study, we examined the discrepancy in functional evaluation between dynamic contrast-enhanced MRU and renal scintigraphy MAG-3 in patients with UPJO who underwent surgery at our hospital over the last 4 years. From a total of 126 patients in the study, only 40 were included in the final analysis. We found a positive correlation coefficient in the relative differential of split renal function between the two modalities. Similarly, El-Nahas et al[12] reported that dMRU analysis of renal function had comparable results to those obtained with renal scintigraphy but superior spatial and contrast resolution. dMRU may be more sensitive than renal scintigraphy for analyzing poorly functional renal collecting systems. In addition to the earlier advantages of dMRU, we found that it is equivalent to nuclear medicine in evaluating split renal function and obstruction (Table 4). Thus, dMRU is a feasible radiological modality for the functional and anatomical evaluation of UPJO. Moreover, it is safe, accurate, and does not require exposure to ionizing radiation. However, the procedure requires sedation and short-term hospitalization. The limitations of this study include a small sample size from a single institution. The requirement for sedation during dMRU presents a practical challenge. Future implications emphasize the need for larger multicenter studies to confirm these findings, while advancements in imaging technology hold promise for enhancing the accessibility and viability of dMRU as a gold standard diagnostic tool for UPJO.
| Scintigraphy MAG-3 + dMRU, n = 40 | Group A < 10% discrepancy, n = 31 | Group B > 10% discrepancy, n = 9 | P value | |
| Number of discrepancies | 6.5 (2-9.8) | 4 (2-8) | 18 (12-24) | < 0.0001 |
| Side | 0.999 | |||
| Right | 13 (33) | 10 (32) | 3 (33) | |
| Left | 27 (67) | 21 (68) | 6 (67) | |
| Renal transit (affected), s | 100 (67-120) | 100 (60-120) | 100 (70-180) | 0.359 |
| Ureteral transit (affected), s | 240 (180-511) | 240 (180-520) | 406 (300-511) | 0.285 |
| Affected renal size, mm | ||||
| RUS | 28 (23-36) | 29 (24-36) | 24 (22-32) | 0.381 |
| MRI | ||||
| Before furosemide | 28 (22-35) | 31 (21-35) | 25 (23-31) | 0.652 |
| After furosemide | 30 (24-40) | 29 (24-42) | 32.5 (25-36) | 0.966 |
| Follow-up, months | 12 (5-20) | 10 (3-16) | 19 (10-26) | 0.05 |
dMRU is equivalent to scintigraphy MAG-3 for evaluating split renal function in UPJO cases of all pediatric age groups. We found that the discrepancies and similarities in renal function were not significantly related to age at diagnosis, sex, or pyelonephritis. We believe that dMRU is an excellent alternative modality for the anatomical and functional evaluation of children with UPJO. However, larger multicenter studies are required to strengthen and consolidate our findings.
Ureteropelvic obstruction is a common pediatric condition, which can be due to congenital internal obstruction or external obstruction secondary to crossing vessels. This study aims to encourage the use of dynamic contrast-enhanced magnetic resonance urography (dMRU) as a modality, measuring renal function as effectively as 99m-technetium mercaptoacetyltriglycine (MAG-3) and providing a good anatomical study in cases of obstruction due to crossing vessels.
dMRU proves advantageous as an alternative modality for ureteropelvic junction obstruction (UPJO). However, enhanced accessibility and cost-effectiveness can be achieved through advancements in magnetic resonance imaging technology.
The optimal imaging modalities for preoperative functional and anatomical assessment of UPJO in pediatric patients.
Analysis of data in patients who underwent surgery for UPJO and had both dMRU and scintigraphy MAG-3 for split renal function assessment.
dMRU is equivalent to scintigraphy MAG-3 for evaluating split renal function in UPJO cases of all pediatric age groups. Future implications emphasize the need for larger multicenter studies to confirm findings, while advancements in imaging technology hold promise for enhancing the accessibility and viability of dMRU as a gold standard diagnostic tool of UPJO.
dMRU is an excellent alternative modality for the anatomical and functional evaluation of children with UPJO. A large sample size is required to confirm this hypothesis.
To enhance the accessibility and viability of dMRU.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: France
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Aydin S, Turkey; Nazir Z, Pakistan S-Editor: Li L L-Editor: Webster JR P-Editor: Zhao S
| 1. | Groth TW, Mitchell ME. Ureteropelvic junction obstruction. In: Coran A, editor. Paediatric Surgery. 7th ed. Philadelphia: Elsevier, 2012: 1411-1425. [DOI] [Cited in This Article: ] |
| 2. | Zderic SA, Lambert SM. Developmental abnormalities of the genitourinary system. In: Gleason CA, Devaskar SU, editor. Avery's Diseases of the Newborn. 9th ed. Philadelphia: Elsevier, 2012: 1191-1204. [DOI] [Cited in This Article: ] |
| 3. | Brown T, Mandell J, Lebowitz RL. Neonatal hydronephrosis in the era of sonography. AJR Am J Roentgenol. 1987;148:959-963. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 157] [Cited by in F6Publishing: 160] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Lawler LP, Jarret TW, Corl FM, Fishman EK. Adult ureteropelvic junction obstruction: insights with three-dimensional multi-detector row CT. Radiographics. 2005;25:121-134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 42] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | González R, Schimke CM. Ureteropelvic junction obstruction in infants and children. Pediatr Clin North Am. 2001;48:1505-1518. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Gopal M, Peycelon M, Caldamone A, Chrzan R, El-Ghoneimi A, Olsen H, Leclair MD, Stillebroer A, MacDonald C, Tonnhofer U, Strasser C, Adam A, Spinoit AF, Haid B. Management of ureteropelvic junction obstruction in children-a roundtable discussion. J Pediatr Urol. 2019;15:322-329. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Metcalfe PD, Assmus M, Kiddoo D. Symptomatic vs asymptomatic pyeloplasties: A single institution review. Can Urol Assoc J. 2014;8:428-431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Atılgan HI, Koca G, Demirel K, Ozyurt S, Yildirim Ş, Orak R, Baskın A, Korkmaz M. Comparative evaluation of differential renal functions and renal parenchymal defects by using the Tc-99m DMSA and Tc-99m MAG3 scintigraphies. Kafkas J Med Sci. 2012;2:43-48. [DOI] [Cited in This Article: ] |
| 9. | O'Reilly PH, Lawson RS, Shields RA, Testa HJ. Idiopathic hydronephrosis--the diuresis renogram: a new non-invasive method of assessing equivocal pelvioureteral junction obstruction. J Urol. 1979;121:153-155. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 111] [Cited by in F6Publishing: 115] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Sharfuddin A. Renal relevant radiology: imaging in kidney transplantation. Clin J Am Soc Nephrol. 2014;9:416-429. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Rohrschneider WK, Hoffend J, Becker K, Clorius JH, Darge K, Kooijman H, Tröger J. Combined static-dynamic MR urography for the simultaneous evaluation of morphology and function in urinary tract obstruction. I. Evaluation of the normal status in an animal model. Pediatr Radiol. 2000;30:511-522. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 70] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | El-Nahas AR, Abou El-Ghar ME, Refae HF, Gad HM, El-Diasty TA. Magnetic resonance imaging in the evaluation of pelvi-ureteric junction obstruction: an all-in-one approach. BJU Int. 2007;99:641-645. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Perez-Brayfield MR, Kirsch AJ, Jones RA, Grattan-Smith JD. A prospective study comparing ultrasound, nuclear scintigraphy and dynamic contrast enhanced magnetic resonance imaging in the evaluation of hydronephrosis. J Urol. 2003;170:1330-1334. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 101] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 14. | El-Diasty T, Mansour O, Farouk A. Diuretic contrast-enhanced magnetic resonance urography vs intravenous urography for depiction of nondilated urinary tracts. Abdom Imaging. 2003;28:135-145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Sidhu G, Beyene J, Rosenblum ND. Outcome of isolated antenatal hydronephrosis: a systematic review and meta-analysis. Pediatr Nephrol. 2006;21:218-224. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 149] [Cited by in F6Publishing: 121] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 16. | Rodigas J, Kirsch H, John U, Seifert P, Winkens T, Stenzel M, Mentzel HJ. Static and Functional MR Urography to Assess Congenital Anomalies of the Kidney and Urinary Tract in Infants and Children: Comparison With MAG3 Renal Scintigraphy and Sonography. AJR Am J Roentgenol. 2018;211:193-203. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |