Published online Apr 15, 2024. doi: 10.4251/wjgo.v16.i4.1227
Peer-review started: October 1, 2023
First decision: January 2, 2024
Revised: January 12, 2024
Accepted: February 20, 2024
Article in press: February 20, 2024
Published online: April 15, 2024
Postoperative delirium, particularly prevalent in elderly patients after abdominal cancer surgery, presents significant challenges in clinical management.
To develop a synthetic minority oversampling technique (SMOTE)-based model for predicting postoperative delirium in elderly abdominal cancer patients.
In this retrospective cohort study, we analyzed data from 611 elderly patients who underwent abdominal malignant tumor surgery at our hospital between September 2020 and October 2022. The incidence of postoperative delirium was recorded for 7 d post-surgery. Patients were divided into delirium and non-delirium groups based on the occurrence of postoperative delirium or not. A multivariate logistic regression model was used to identify risk factors and develop a predictive model for postoperative delirium. The SMOTE technique was applied to enhance the model by oversampling the delirium cases. The model’s predictive accuracy was then validated.
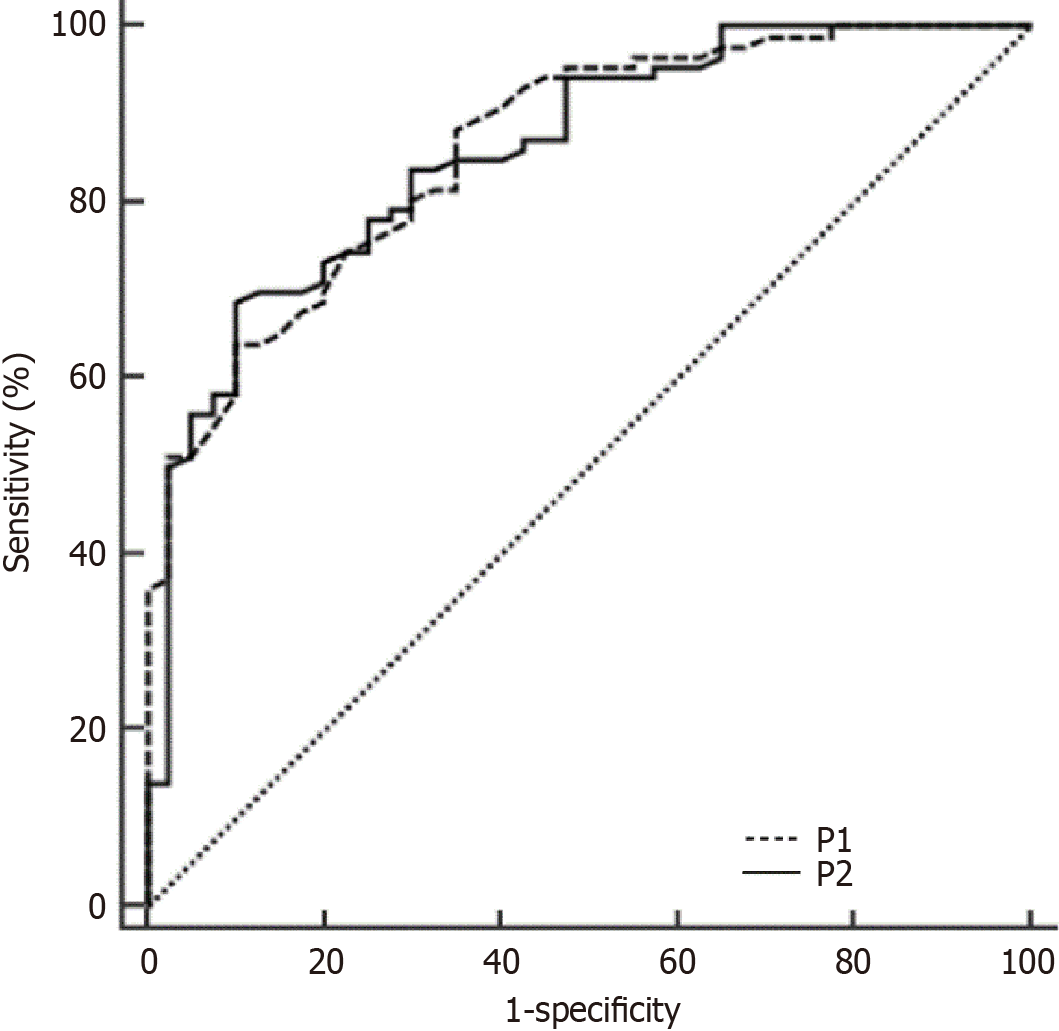
In our study involving 611 elderly patients with abdominal malignant tumors, multivariate logistic regression analysis identified significant risk factors for postoperative delirium. These included the Charlson comorbidity index, American Society of Anesthesiologists classification, history of cerebrovascular disease, surgical duration, perioperative blood transfusion, and postoperative pain score. The incidence rate of postoperative delirium in our study was 22.91%. The original predictive model (P1) exhibited an area under the receiver operating characteristic curve of 0.862. In comparison, the SMOTE-based logistic early warning model (P2), which utilized the SMOTE oversampling algorithm, showed a slightly lower but comparable area under the curve of 0.856, suggesting no significant difference in performance between the two predictive approaches.
This study confirms that the SMOTE-enhanced predictive model for postoperative delirium in elderly abdominal tumor patients shows performance equivalent to that of traditional methods, effectively addressing data imbalance.
Core Tip: Our study develops a predictive model for postoperative delirium in elderly patients with abdominal malignancies, using the synthetic minority oversampling technique. This model highlights key risk factors including the Charlson comorbidity index, anesthesia grade, cerebrovascular disease history, surgical duration, perioperative transfusion, and postoperative pain. Its validation demonstrates effectiveness in clinical settings, enhancing care and outcomes for this high-risk group.
- Citation: Hu WJ, Bai G, Wang Y, Hong DM, Jiang JH, Li JX, Hua Y, Wang XY, Chen Y. Predictive modeling for postoperative delirium in elderly patients with abdominal malignancies using synthetic minority oversampling technique. World J Gastrointest Oncol 2024; 16(4): 1227-1235
- URL: https://www.wjgnet.com/1948-5204/full/v16/i4/1227.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v16.i4.1227
In our study involving elderly patients undergoing surgery for abdominal malignant tumors, we observed a significant incidence of postoperative delirium, consistent with previous studies indicating an incidence range between 20% and 40%[1-3]. This condition not only affects patients during the immediate postoperative period but also has long-term implications for their health.
Postoperative delirium is not only a transient complication; within a year of its onset, up to 10% of affected patients may die, and approximately 40% may develop chronic encephalopathy syndrome, severely impacting their prognosis[4]. Therefore, the prevention and management of postoperative delirium in patients with abdominal malignant tumors are vital for improving their overall outcomes.
While pharmacological prevention strategies for postoperative delirium are still under investigation, non-pharmacological methods focus on identifying high-risk factors and implementing targeted interventions to reduce the incidence of delirium. However, traditional methods often struggle with imbalanced data, leading to compromised predictive accuracy[5]. To address this issue, our study employed the synthetic minority oversampling technique (SMOTE), deve
To determine the appropriate sample size for our study, we utilized a predictive equation accounting for 11 factors, with each requiring a minimum of 5-10 cases for validation. Previous studies indicated an incidence rate of postoperative delirium between 20%-40%. Factoring in a 10% follow-up loss rate, we calculated the estimated sample size as follows: (11 × 10/0.2)/0.9 = 611. Therefore, we retrospectively analyzed 611 elderly patients with abdominal malignant tumors who underwent surgery between September 2020 and October 2022, according to the following inclusion criteria.
The inclusion criteria were: (1) Hospitalized patients diagnosed with colorectal cancer per the International Classification of Diseases-10[8]; (2) Age 65-75 years; (3) Patients undergoing surgical treatment; and (4) Informed and willing par
In this study, we conducted a retrospective analysis of 611 elderly patients with abdominal malignant tumors. Surgical procedures were standardized and performed by the same team. Data collection included general information, laboratory examinations, and surgical details through a comprehensive, self-designed questionnaire. The questionnaire utilized semi-structured interviews and expert consultations for formulation. Key indicators encompassed patient demographics, Charlson comorbidity index, tumor stage, American Society of Anesthesiologists (ASA) classification, laboratory values, and surgical details including method, duration, intraoperative blood loss, and postoperative pain assessed using the visual analogue scale.
The SMOTE algorithm was employed as follows: (1) Determine the number of minority class samples as B and set the desired increase in the number of samples by n times; (2) Implement SMOTE processing, randomly selecting one sample
In this study, we monitored 611 elderly patients with abdominal malignant tumors for 7 d post-surgery to identify instances of delirium. These patients were then classified into delirium and non-delirium groups. The diagnosis of postoperative delirium was based on the Ambiguity Assessment Scale, a validated tool for delirium screening[9,10]. This scale assesses acute onset and fluctuating mental state, concentration difficulty, confused thinking, and altered con
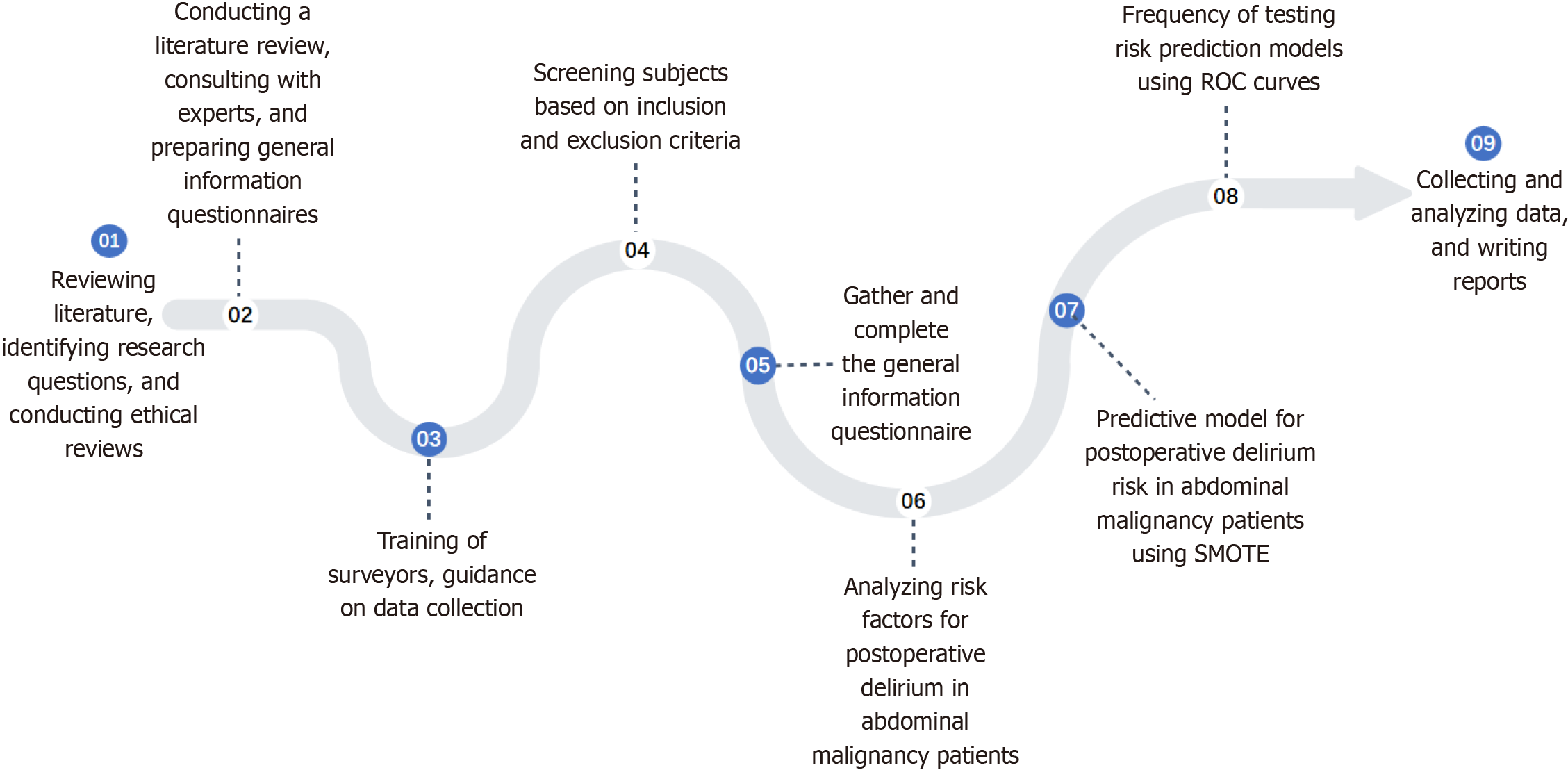
Statistical analyses were performed using SPSS software (version 23.0, IBM Corporation, United States) and R software (version 4.1.0, R Foundation for Statistical Computing, Vienna, Austria). Independent t-tests were applied for inter-group comparisons of normally distributed data. For non-normally distributed data, comparisons were made using the Wilcoxon rank-sum test. Count data were analyzed using the χ2 test. Risk factors for postoperative delirium in elderly patients with abdominal malignant tumors were examined through Fisher’s exact tests, Mann-Whitney U tests, and multivariate logistic regressions. The model’s predictive performance was assessed using receiver operating characteristic (ROC) curve analysis, with a significance level set at P < 0.05. The methodological approach is illustrated in Figure 1.
Of 611 elderly abdominal malignant tumor patients, 140 experienced postoperative delirium, indicating a 22.91% incidence rate. The remaining 471 patients did not develop delirium.
Clinical data between the delirium group (140 patients) and the non-delirium group (471 patients) were compared using independent t-tests for continuous variables and χ2 tests for categorical variables. No significant differences were noted in general demographics such as gender or age (P > 0.05). However, significant differences were found in the Charlson comorbidity index (P = 0.002, χ2 test), ASA classification (P = 0.001, χ2 test), history of cerebrovascular diseases (P = 0.017, χ2 test), duration of surgery (P = 0.023, t-test), perioperative blood transfusion (P = 0.003, χ2 test), and postoperative pain score (P < 0.001, t-test) (Table 1).
| Factor | Delirium group (n = 140) | Non-delirium group (n = 471) | Z/t/χ2 | P value |
| Age (yr) | 71.00 ± 3.32 | 70.37 ± 4.45 | 1.813 | 0.071 |
| Gender (male/female) | 75/65 | 257/214 | 0.043 | 0.836 |
| BMI (kg/m2) | 23.41 ± 3.96 | 24.06 ± 2.34 | 1.849 | 0.066 |
| Charlson comorbidity index, n (%) | 9.497 | 0.002 | ||
| 0-2 | 62 (44.29) | 278 (59.02) | ||
| ≥ 3 | 78 (55.71) | 193 (40.98) | ||
| Tumor TMN stage, n (%) | 3.722 | 0.054 | ||
| I-II | 98 (70.00) | 367 (77.92) | ||
| III-IV | 42 (30.00) | 104 (22.08) | ||
| American Society of Anesthesiologists classification, n (%) | 10.999 | 0.001 | ||
| I-II | 112 (80.00) | 307 (65.18) | ||
| III-IV | 28 (20.00) | 164 (34.82) | ||
| Nutritional risk, n (%) | 0.853 | 0.356 | ||
| < 3 patients | 78 (55.71) | 283 (60.08) | ||
| ≥ 3 patients | 62 (44.29) | 188 (39.92) | ||
| History of cerebrovascular disease, n (%) | 15 (10.71) | 24 (5.10) | 5.702 | 0.017 |
| Postoperative hemoglobin level (g/L) | 116.34 ± 15.85 | 114.91 ± 17.33 | 0.917 | 0.360 |
| Postoperative blood potassium level (mmol/L) | 4.41 ± 0.25 | 4.39 ± 0.24 | 0.839 | 0.403 |
| Postoperative hematocrit (%) | 32.17 ± 2.58 | 32.44 ± 2.17 | 1.126 | 0.262 |
| Postoperative cholesterol level (mg/dL) | 176.52 ± 50.15 | 167.56 ± 42.15 | 1.922 | 0.056 |
| Postoperative serum creatinine value (μmol/L) | 75.43 ± 24.87 | 72.32 ± 22.89 | 1.322 | 0.187 |
| Postoperative alanine transaminase level (U/L) | 43.69 ± 4.33 | 42.94 ± 4.45 | 1.788 | 0.075 |
| Surgical method | 0.040 | 0.842 | ||
| Laparoscopic | 124 (88.57) | 420 (89.17) | ||
| Open | 16 (11.43) | 51 (10.83) | ||
| Surgical duration (min) | 228 (203,251) | 213 (196,231) | 2.293 | 0.023 |
| Intraoperative bleeding volume (mL) | 100 (201,527) | 90 (151,350) | 1.765 | 0.079 |
| Perioperative blood transfusion, n (%) | 28 (20.00) | 49 (10.40) | 9.024 | 0.003 |
| Postoperative pain score | 4.01 ± 1.35 | 3.31 ± 1.10 | 5.607 | < 0.001 |
| Atomization use, n (%) | 56 (40.00) | 173 (36.73) | 0.492 | 0.483 |
| Ventilator use, n (%) | 4 (2.86) | 4 (0.85) | 3.367 | 0.067 |
Multivariate logistic regression analyses revealed that the Charlson comorbidity index (P < 0.001), ASA classification (P < 0.001), history of cerebrovascular diseases (P < 0.001), surgical duration (P = 0.009), perioperative blood transfusion (P < 0.001), and postoperative pain score (P < 0.001) were significant risk factors for postoperative delirium in elderly patients with abdominal malignant tumors, as per Table 2. Based on the identified independent risk factors and their corresponding regression coefficients, we developed an original predictive model, denoted as P1, as follows: P1 = -5.416 + (0.748 × Charlson comorbidity index) + (0.756 × ASA classification) + (1.182 × history of cerebrovascular disease) + (1.174 × surgery duration) + (1.063 × perioperative blood transfusion) + (1.120 × postoperative pain score), where the assessment of postoperative pain was conducted using the Hosmer-Lemeshow test. The results showed a decisive correlation coefficient (R2) of 0.349 (P = 0.784), indicating a good fit of the model.
| Related indicator | β | SE | Wald | P value | OR | 95%CI | |
| Lower | Upper | ||||||
| Charlson comorbidity index | 0.748 | 0.237 | 2.985 | < 0.001 | 2.113 | 1.970 | 5.266 |
| American Society of Anesthesiologists classification | 0.756 | 0.223 | 8.945 | < 0.001 | 2.130 | 1.586 | 4.691 |
| History of cerebrovascular diseases | 1.182 | 0.226 | 5.752 | < 0.001 | 3.261 | 2.293 | 5.681 |
| Duration of surgery | 1.174 | 0.227 | 5.124 | 0.009 | 3.235 | 2.440 | 4.469 |
| Perioperative blood transfusion | 1.063 | 0.219 | 3.754 | < 0.001 | 2.895 | 2.194 | 6.692 |
| Postoperative pain score | 1.120 | 0.379 | 9.421 | < 0.001 | 3.065 | 2.610 | 4.725 |
The logistic warning model based on the SMOTE algorithm was employed to perform 10-fold oversampling, resulting in an approximate postoperative delirium occurrence to non-occurrence ratio in elderly patients with abdominal malignant tumors of 10/19 (471 without postoperative delirium, 462 with postoperative delirium). Subsequently, the data were refit to the logistic regression model (Table 3), and an early warning model (P2) was derived: P2 = -3.492 + (0.527 based on SMOTE oversampling algorithm × Charlson comorbidity index) + (0.544 × ASA classification) + (1.167 × history of cerebrovascular disease) + (1.154 × surgery duration) + (1.007 × perioperative blood transfusion) + (1.132 × postoperative pain score). A Hosmer-Lemeshow test was performed on the model, producing a decisive coefficient of correlation (R2 = 0.355, P = 0.990), indicating a good fit of the model.
| Related indicator | β | SE | Wald | P value | OR | 95%CI | |
| Lower | Upper | ||||||
| Charlson comorbidity index | 0.527 | 0.522 | 6.313 | 0.012 | 1.693 | 1.494 | 5.388 |
| American Society of Anesthesiologists classification | 0.544 | 0.576 | 10.844 | 0.009 | 1.723 | 1.536 | 6.775 |
| History of cerebrovascular diseases | 1.167 | 0.613 | 10.142 | 0.003 | 3.212 | 1.930 | 3.397 |
| Duration of surgery | 1.154 | 0.565 | 5.685 | 0.025 | 3.170 | 2.326 | 7.894 |
| Perioperative blood transfusion | 1.007 | 0.558 | 13.022 | 0.001 | 2.737 | 1.247 | 3.682 |
| Postoperative pain score | 1.132 | 0.822 | 11.912 | 0.001 | 3.101 | 2.092 | 12.064 |
In our study, we compared the effectiveness of the two predictive models, P1 and P2, by analyzing their ROC curves. The ROC curve analysis showed that the area under the curve (AUC) for the early warning model P1 was 0.862 [95% confidence interval (CI): 0.789-0.917], while the AUC for the SMOTE-enhanced model P2 was 0.856 (95%CI: 0.782-0.912; Figure 2). This comparison indicates no significant difference in performance between the predictive model constructed using the SMOTE algorithm (P2) and the original logistic regression model (P1) (P > 0.05).
Abdominal malignant tumors, including stomach, colon, liver, gallbladder, and pancreas malignancies, are highly prevalent cancers, particularly impacting the well-being of the elderly[11,12]. Surgical interventions are crucial in managing these tumors, but they bring significant risks. Factors such as substantial surgical trauma, high anesthesia risk, and the presence of comorbidities, aging, and frailty in elderly patients increase the likelihood of postoperative delirium[13]. This condition leads to adverse outcomes like falls, self-injury, and prolonged hospital stays, thereby intensifying the medical and social burden[14]. Effective prediction, prevention, and management of postoperative delirium in patients with these malignancies are, therefore, of great clinical importance. However, to date, this topic has not been adequately addressed in the clinical field in China.
The challenge in constructing predictive models for postoperative delirium, especially in the context of abdominal malignant tumors, lies in the inadequacy of traditional statistical methods when dealing with imbalanced datasets. Such methods often compromise predictive accuracy, a critical issue highlighted in previous research[15,16]. Addressing this, the SMOTE has been recognized as an effective solution. SMOTE, by generating synthetic minority samples from the existing dataset, helps in balancing the data, thereby enhancing the model’s predictive capabilities[17-19]. Our study embraced this approach, utilizing SMOTE to refine our predictive model for postoperative delirium in elderly patients with abdominal malignant tumors. The findings underscore the enhanced utility and reliability of the SMOTE-enhanced model in clinical settings.
Our univariate and multivariate logistic regression analyses highlight significant risk factors for postoperative delirium in elderly patients with abdominal malignant tumors, including a Charlson comorbidity index ≥ 3, ASA classifications III-IV, and extended surgical duration. These findings align with previous research indicating increased postoperative cognitive impairment and delirium risks associated with higher Charlson comorbidity index scores and anesthesia grades. Such patients often experience diminished physical function and self-regulation, heightening their sensitivity to anesthesia and surgery stress. This leads to a reduced tolerance for narcotics and surgical stimuli[20-22]. Prolonged surgery necessitates extended anesthesia, increasing narcotic usage and risk of narcotic accumulation, thereby elevating postoperative delirium risk[23,24]. Moreover, impaired cholinergic function in patients with higher comorbidity and anesthesia grades further triggers postoperative delirium[25]. Even without surgery, patients with multiple comorbidities face a heightened delirium risk[26]. Thus, for elderly patients with abdominal malignant tumors and high comorbidity and anesthesia grades, enhancing intraoperative vigilance and adjusting anesthesia plans to minimize narcotics, such as fentanyl, is crucial for reducing postoperative delirium risk.
Our study identified that a history of cerebrovascular disease, perioperative blood transfusion, and postoperative pain scores are significant risk factors for postoperative delirium in patients with abdominal malignant tumors. Cere
In the context of big data, addressing data imbalance is crucial to avoid inaccuracies in predictive models. The SMOTE algorithm effectively mitigates this issue by generating synthetic minority samples, thereby reducing the risk of model overfitting[29]. Our study demonstrated no significant difference in performance between models constructed using the SMOTE algorithm and those based on original sample statistics. This finding aligns with prior research, confirming the efficacy of SMOTE in addressing data imbalance[30,31]. Thus, SMOTE is a valuable tool for constructing accurate predictive models, particularly in scenarios with imbalanced data. Our study’s predictive model for postoperative delirium in elderly patients with abdominal malignant tumors, developed using the SMOTE algorithm, showed performance comparable to that of models based on traditional statistical methods.
In summary, our study demonstrated that the predictive model for postoperative delirium in elderly patients with abdominal malignant tumors, developed using the SMOTE technique, achieved predictive performance comparable to that of models based on traditional statistical methods. This highlights the effectiveness of the SMOTE technique in managing imbalanced data and building reliable predictive models. It is crucial to acknowledge the limitations of our study, which include potential biases due to the exclusion of certain risk factors and reliance on limited individual data. Future research should explore alternative data balancing approaches to mitigate such biases.
This study has established that the SMOTE-based predictive model for postoperative delirium in elderly patients with abdominal malignant tumors demonstrates predictive accuracy comparable to that of traditional methods. The findings highlight the efficacy of the SMOTE technique in managing imbalanced datasets, thereby contributing to the development of reliable predictive models in clinical settings.
Postoperative delirium is a serious complication that disproportionately affects elderly patients undergoing surgery for abdominal malignant tumors, including stomach, colon, liver, gallbladder, and pancreas cancers. This condition challenges patient care and leads to adverse outcomes, such as prolonged hospital stays and increased mortality. Our study focused on developing predictive models using advanced techniques like the synthetic minority oversampling technique (SMOTE) to identify patients at risk, aiming to fill a critical gap in this domain.
There is an urgent need for an accurate predictive model for postoperative delirium in elderly patients after abdominal malignant tumor surgeries. With the high incidence and impact of delirium on this demographic, particularly in prognosis and healthcare burden, an effective predictive tool is paramount. This study enhances early detection and intervention, contributing significantly to geriatric oncology and postoperative care knowledge.
Our primary goal was to create a robust predictive model for postoperative delirium in elderly patients undergoing abdominal malignant tumor surgery. We aimed to identify and validate significant risk factors and assess the model’s accuracy and efficacy. A novel aspect of our research was applying SMOTE to enhance predictive accuracy in imbalanced data sets, offering a validated model for early identification and management of postoperative delirium, and demonstrating SMOTE’s potential in medical research.
The study involved a retrospective analysis of 611 elderly patients who underwent surgery for abdominal malignant tumors from September 2020 to October 2022. We used multivariate logistic regression to identify risk factors for postoperative delirium, incorporating SMOTE to address data imbalance. Our validation process ensured the model’s accuracy and reliability.
We analyzed various risk factors for postoperative delirium in our patient cohort. Factors like the Charlson comorbidity index, anesthesia grade, cerebrovascular disease history, surgical duration, perioperative blood transfusion, and postoperative pain score were significant. Our SMOTE-enhanced predictive model showed superior accuracy over traditional methods, indicating a potential leap in clinical management of postoperative delirium.
Our study introduces a novel, SMOTE-augmented predictive model for postoperative delirium in elderly patients undergoing abdominal malignant tumor surgery. This model addresses dataset imbalances common in medical research, improving predictive accuracy and offering methodological advancements in medical analytics. It holds promise for early intervention and improved patient care.
Future research should focus on the prospective validation of this model and its integration into clinical practice. Enhancing predictive accuracy and generalizability is key. Investigations should include larger, more diverse patient cohorts and additional predictive factors to broaden the model’s clinical applicability.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zeng C, United States S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Zhao YQ
| 1. | Evered LA, Chan MTV, Han R, Chu MHM, Cheng BP, Scott DA, Pryor KO, Sessler DI, Veselis R, Frampton C, Sumner M, Ayeni A, Myles PS, Campbell D, Leslie K, Short TG. Anaesthetic depth and delirium after major surgery: a randomised clinical trial. Br J Anaesth. 2021;127:704-712. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 121] [Article Influence: 40.3] [Reference Citation Analysis (0)] |
| 2. | Deng Y, Qin Z, Wu Q, Liu L, Yang X, Ju X, Zhang Y. Efficacy and Safety of Remimazolam Besylate versus Dexmedetomidine for Sedation in Non-Intubated Older Patients with Agitated Delirium After Orthopedic Surgery: A Randomized Controlled Trial. Drug Des Devel Ther. 2022;16:2439-2451. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 3. | Li T, Li J, Yuan L, Wu J, Jiang C, Daniels J, Mehta RL, Wang M, Yeung J, Jackson T, Melody T, Jin S, Yao Y, Chen J, Smith FG, Lian Q; RAGA Study Investigators. Effect of Regional vs General Anesthesia on Incidence of Postoperative Delirium in Older Patients Undergoing Hip Fracture Surgery: The RAGA Randomized Trial. JAMA. 2022;327:50-58. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 123] [Article Influence: 61.5] [Reference Citation Analysis (0)] |
| 4. | Ren A, Zhang N, Zhu H, Zhou K, Cao Y, Liu J. Effects of Preoperative Anxiety on Postoperative Delirium in Elderly Patients Undergoing Elective Orthopedic Surgery: A Prospective Observational Cohort Study. Clin Interv Aging. 2021;16:549-557. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Popoola SI, Adebisi B, Ande R, Hammoudeh M, Anoh K, Atayero AA. SMOTE-DRNN: A Deep Learning Algorithm for Botnet Detection in the Internet-of-Things Networks. Sensors (Basel). 2021;21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 6. | Chang CC, Li YZ, Wu HC, Tseng MH. Melanoma Detection Using XGB Classifier Combined with Feature Extraction and K-Means SMOTE Techniques. Diagnostics (Basel). 2022;12. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 7. | Naseriparsa M, Al-Shammari A, Sheng M, Zhang Y, Zhou R. RSMOTE: improving classification performance over imbalanced medical datasets. Health Inf Sci Syst. 2020;8:22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Fung KW, Xu J, Bodenreider O. The new International Classification of Diseases 11th edition: a comparative analysis with ICD-10 and ICD-10-CM. J Am Med Inform Assoc. 2020;27:738-746. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 9. | Ooms M, Schooß R, Winnand P, Heitzer M, Hölzle F, Bickenbach J, Rieg A, Modabber A. Influence of perioperative blood pressure regulation on postoperative delirium in patients undergoing head and neck free flap reconstruction. Eur J Med Res. 2023;28:365. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 10. | Zhou Y, Wang X, Li Z, Ma Y, Yu C, Chen Y, Ding J, Yu J, Zhou R, Yang N, Liu T, Guo X, Fan T, Shi C. Development of a Brief Cognitive Screening Tool for Predicting Postoperative Delirium in Patients with Parkinson's Disease: A Secondary Analysis. Clin Interv Aging. 2023;18:1555-1564. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 11. | Kamps SE, Otjen JP, Stanescu AL, Mileto A, Lee EY, Phillips GS. Dual-Energy CT of Pediatric Abdominal Oncology Imaging: Private Tour of New Applications of CT Technology. AJR Am J Roentgenol. 2020;214:967-975. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Gagliardi T, Adejolu M, deSouza NM. Diffusion-Weighted Magnetic Resonance Imaging in Ovarian Cancer: Exploiting Strengths and Understanding Limitations. J Clin Med. 2022;11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Liu Q, Li L, Wei J, Xie Y. Correlation and influencing factors of preoperative anxiety, postoperative pain, and delirium in elderly patients undergoing gastrointestinal cancer surgery. BMC Anesthesiol. 2023;23:78. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 14. | Li B, Ju J, Zhao J, Qin Y, Zhang Y. A Nomogram to Predict Delirium after Hip Replacement in Elderly Patients with Femoral Neck Fractures. Orthop Surg. 2022;14:3195-3200. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 15. | Xu Z, Shen D, Kou Y, Nie T. A Synthetic Minority Oversampling Technique Based on Gaussian Mixture Model Filtering for Imbalanced Data Classification. IEEE Trans Neural Netw Learn Syst. 2024;35:3740-3753. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Reference Citation Analysis (0)] |
| 16. | Kosolwattana T, Liu C, Hu R, Han S, Chen H, Lin Y. A self-inspected adaptive SMOTE algorithm (SASMOTE) for highly imbalanced data classification in healthcare. BioData Min. 2023;16:15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 3] [Reference Citation Analysis (0)] |
| 17. | Sohrawordi M, Hossain MA. Prediction of lysine formylation sites using support vector machine based on the sample selection from majority classes and synthetic minority over-sampling techniques. Biochimie. 2022;192:125-135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Ahmed HA, Hameed A, Bawany NZ. Network intrusion detection using oversampling technique and machine learning algorithms. PeerJ Comput Sci. 2022;8:e820. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Shahinfar S, Al-Mamun HA, Park B, Kim S, Gondro C. Prediction of marbling score and carcass traits in Korean Hanwoo beef cattle using machine learning methods and synthetic minority oversampling technique. Meat Sci. 2020;161:107997. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Versloot J, Minotti SC, Amer S, Ali A, Ma J, Peters ML, Saab H, Tang T, Kerr J, Reid R. Effectiveness of a Multi-component Delirium Prevention Program Implemented on General Medicine Hospital Units: an Interrupted Time Series Analysis. J Gen Intern Med. 2023;38:2936-2944. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 21. | Lee SS, Kim JH, Lee JJ, Kwon YS, Seo EM. The Impact of Blood Transfusion in Developing Postoperative Delirium in Patients with Hip Fracture Surgery. J Clin Med. 2023;12. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 22. | Bhushan S, Huang X, Duan Y, Xiao Z. The impact of regional versus general anesthesia on postoperative neurocognitive outcomes in elderly patients undergoing hip fracture surgery: A systematic review and meta-analysis. Int J Surg. 2022;105:106854. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 21] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 23. | Subramaniam B, Shankar P, Shaefi S, Mueller A, O'Gara B, Banner-Goodspeed V, Gallagher J, Gasangwa D, Patxot M, Packiasabapathy S, Mathur P, Eikermann M, Talmor D, Marcantonio ER. Effect of Intravenous Acetaminophen vs Placebo Combined With Propofol or Dexmedetomidine on Postoperative Delirium Among Older Patients Following Cardiac Surgery: The DEXACET Randomized Clinical Trial. JAMA. 2019;321:686-696. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 175] [Cited by in F6Publishing: 169] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 24. | Wang HY, Chen TY, Li DJ, Lin PY, Su KP, Chiang MH, Carvalho AF, Stubbs B, Tu YK, Wu YC, Roerecke M, Smith L, Tseng PT, Hung KC. Association of pharmacological prophylaxis with the risk of pediatric emergence delirium after sevoflurane anesthesia: An updated network meta-analysis. J Clin Anesth. 2021;75:110488. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 25. | Lawson RA, Richardson SJ, Kershaw D, Davis D, Stephan BCM, Robinson L, Brayne C, Barnes L, Burn DJ, Yarnall AJ, Taylor JP, Parker S, Allan LM. Evaluation of Bedside Tests of Attention and Arousal Assessing Delirium in Parkinson's Disease, Dementia, and Older Adults. J Parkinsons Dis. 2022;12:655-665. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 26. | Song Y, Liu Y, Yuan Y, Jia X, Zhang W, Wang G, Jia Y, Wang X, Liu L, Li W, Li X, Cai N, Liu C, Li Y, Han Y, Zhou Y, Mi X, Shi C, Wang JQ, Vuylsteke A, Guo X, Li Z. Effects of general versus subarachnoid anaesthesia on circadian melatonin rhythm and postoperative delirium in elderly patients undergoing hip fracture surgery: A prospective cohort clinical trial. EBioMedicine. 2021;70:103490. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 27. | Forner D, Hueniken K, Yoannidis T, Witterick I, Monteiro E, Zadeh G, Gullane P, Snyderman C, Wang E, Gardner P, Valappil B, Fliss DM, Ringel B, Gil Z, Na'ara S, Ooi EH, Goldstein DP, Muhanna N, Gentili F, de Almeida JR. Psychometric testing of the Skull Base Inventory health-related quality of life questionnaire in a multi-institutional study of patients undergoing open and endoscopic surgery. Qual Life Res. 2021;30:293-301. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 28. | Ren S, Zang C, Yuan F, Yan X, Zhang Y, Yuan S, Sun Z, Lang B. Correlation between burst suppression and postoperative delirium in elderly patients: a prospective study. Aging Clin Exp Res. 2023;35:1873-1879. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 29. | Duan F, Zhang S, Yan Y, Cai Z. An Oversampling Method of Unbalanced Data for Mechanical Fault Diagnosis Based on MeanRadius-SMOTE. Sensors (Basel). 2022;22. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 30. | Delgado R, Núñez-González JD. Bayesian network-based over-sampling method (BOSME) with application to indirect cost-sensitive learning. Sci Rep. 2022;12:8724. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 31. | Wang S, Dai Y, Shen J, Xuan J. Research on expansion and classification of imbalanced data based on SMOTE algorithm. Sci Rep. 2021;11:24039. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |