Copyright
©The Author(s) 2025.
World J Hepatol. May 27, 2025; 17(5): 104724
Published online May 27, 2025. doi: 10.4254/wjh.v17.i5.104724
Published online May 27, 2025. doi: 10.4254/wjh.v17.i5.104724
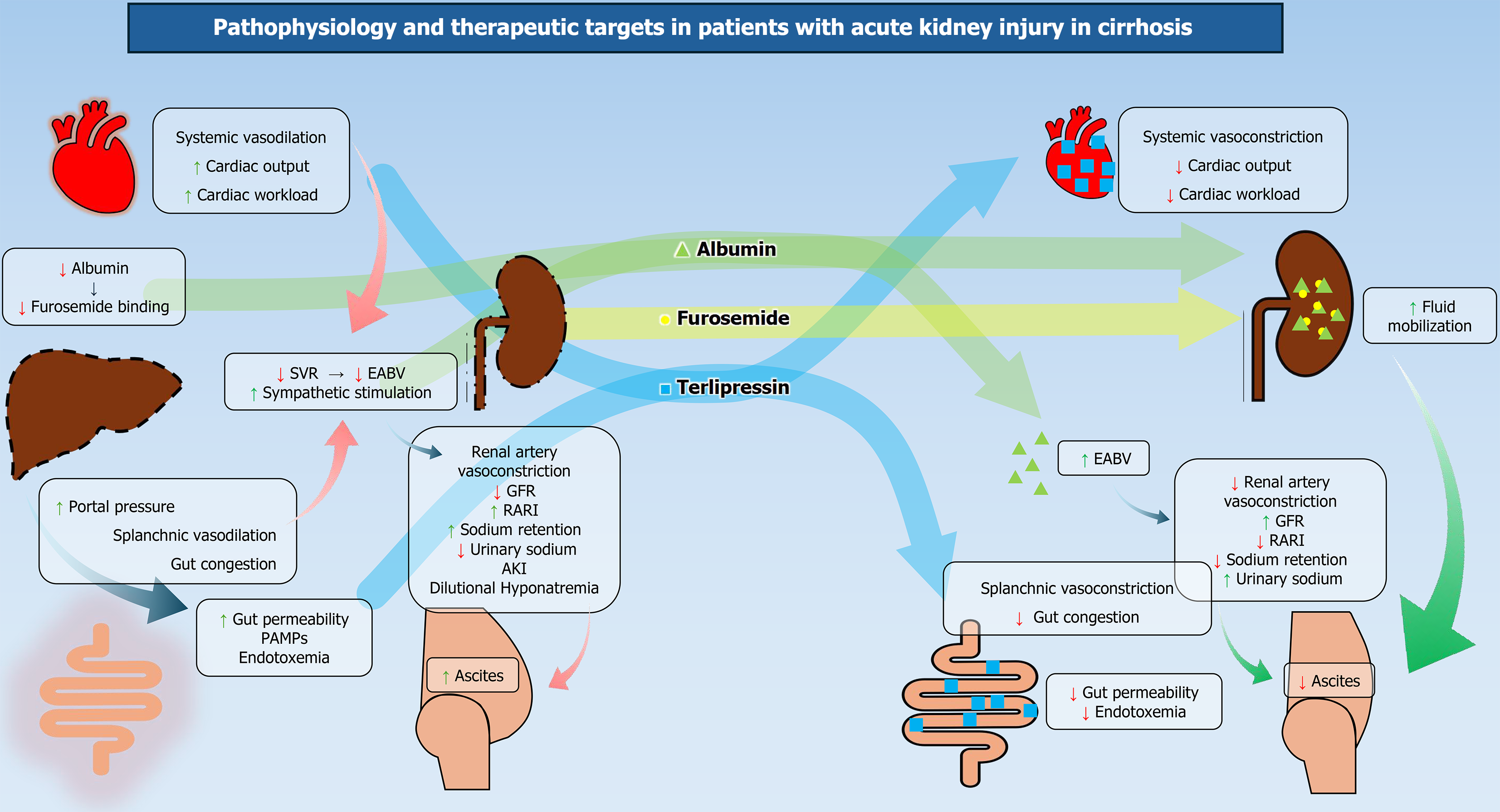
Figure 1 Altered hemodynamic and targets of therapy in patients with acute kidney injury in cirrhosis.
Increased intestinal permeability allows gut-derived lipopolysaccharides to enter the systemic circulation. Overwhelming systemic vasodilatation leads to a decrease in systemic vascular resistance and effective blood volume. Underfilling of the renal vasculature activates the renin-angiotensin-aldosterone system (RAAS) axis. RAAS activation leads to sodium retention, reduced glomerular filtration rate, and ascites. The quantitative defects in albumin contribute to decreased oncotic pressure and further worsen hemodynamics. Hence, albumin, along with splanchnic vasoconstrictors, is the mainstay of treatment in patients with hepatorenal syndrome. AKI: Acute kidney injury; EABV: Effective arterial blood volume; GFR: Glomerular filtration rate; PAMPs: Pathogen-associated molecular patterns; RARI: Renal artery resistive index; SVR: Systemic vascular resistance.
- Citation: Malakar S, Rungta S, Samanta A, Shamsul Hoda U, Mishra P, Pande G, Roy A, Giri S, Rai P, Mohindra S, Ghoshal UC. Understanding acute kidney injury in cirrhosis: Current perspective. World J Hepatol 2025; 17(5): 104724
- URL: https://www.wjgnet.com/1948-5182/full/v17/i5/104724.htm
- DOI: https://dx.doi.org/10.4254/wjh.v17.i5.104724