Copyright
©The Author(s) 2023.
World J Stem Cells. Dec 26, 2023; 15(12): 1035-1062
Published online Dec 26, 2023. doi: 10.4252/wjsc.v15.i12.1035
Published online Dec 26, 2023. doi: 10.4252/wjsc.v15.i12.1035
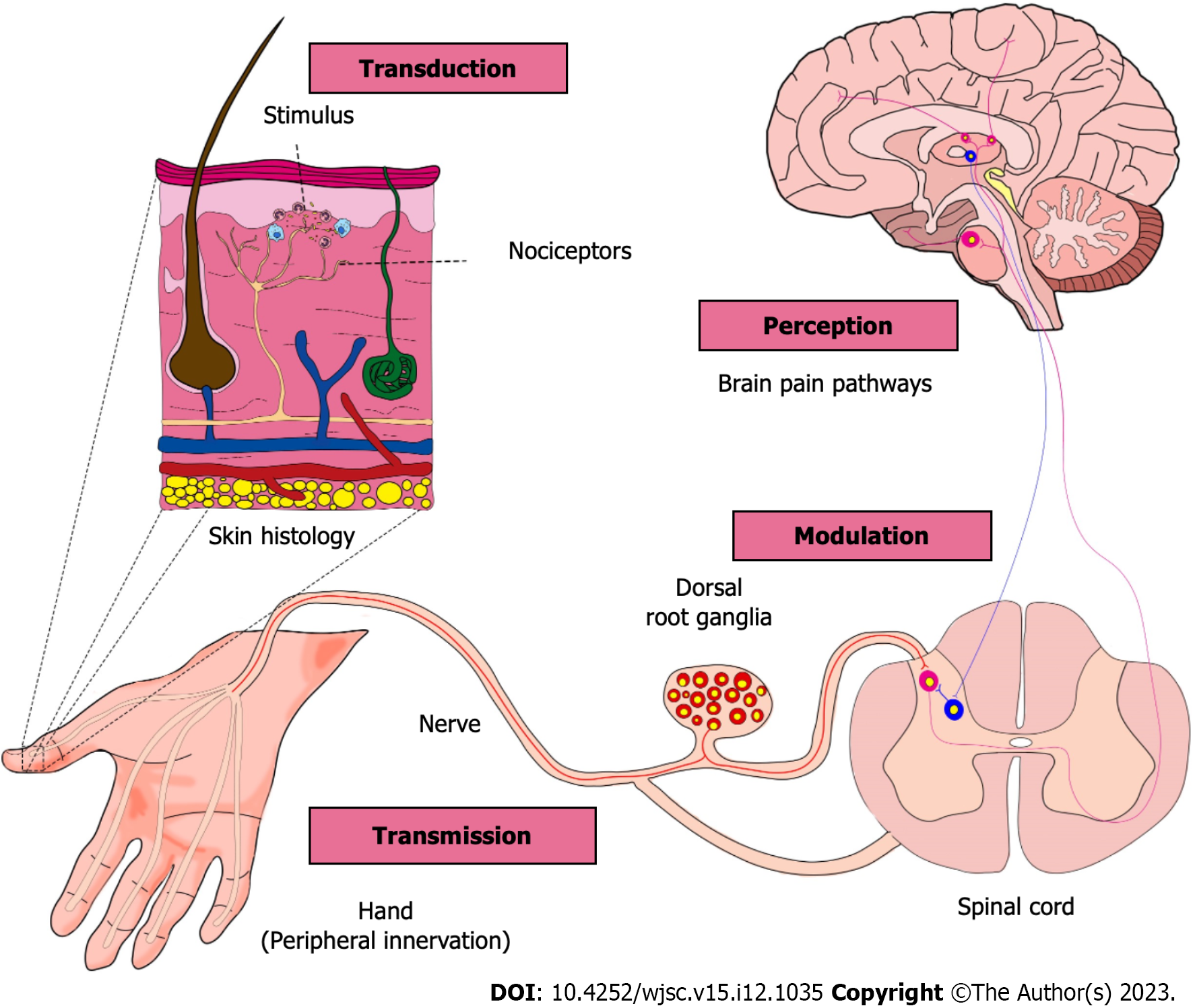
Figure 1 Pain mechanism.
Representative diagram of anatomical levels involved in the steps of pain from detection of stimulus up to its interpretation and modulation. Starting from the left to the right sides of the figure. The initiation of pain processing starts with the sensing of a noxius stimulus on the skin. This stimulus is detected by nociceptors (whose cellular bodies are in dorsal root ganglia and axons that project to the peripheral tissues and spinal cord) and then relayed to the spinal cord before ultimately reaching the brain (depicted by the ascending pathways in pink). In the brain, the stimulus is interpreted and converted into the sensation of pain. Subsequently, descending pathways (represented in blue) become active, limiting nociceptive input at the spinal cord level. It is crucial to emphasize that glial cells play a significant role in the transmission and modulation of pain. They are activated by neuropeptides released by neurons as well as inflammatory molecules released by immune cells. The recognition of these molecules, whether they are pro-nociceptive or anti-nociceptive, can stimulate glial cells to alter their behavior and contribute to the persistence of the stimulus by releasing nociceptive molecules. Nociceptive neurons can also interact with immune cells that release molecules capable of activating and sensitizing these neurons as well as cause neurogenic inflammation. Varied pathogens (e.g., bacteria, parasites, virus) present virulence factors that can activate nociceptor neurons. For a further in-depth understanding of pain mechanisms in varied conditions we recommend the following review articles[125,174-177].
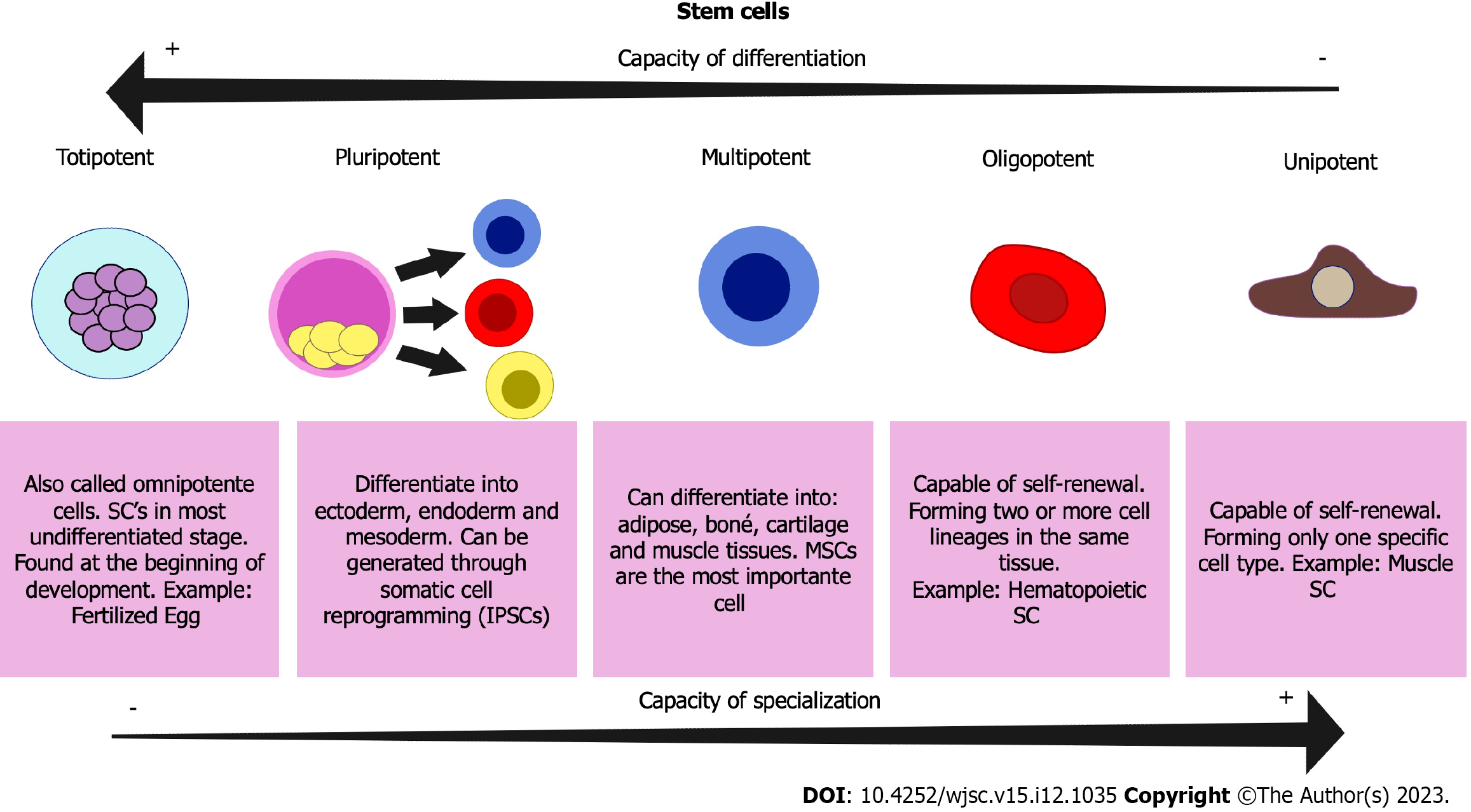
Figure 2 Types of stem cells: Different types and characteristics.
Representative scheme of the different subtypes of stem cells and their main characteristics. SC: Stem cells; MSC: Mesenchymal stem cell; iPSC: Induced pluripotent stem cell.
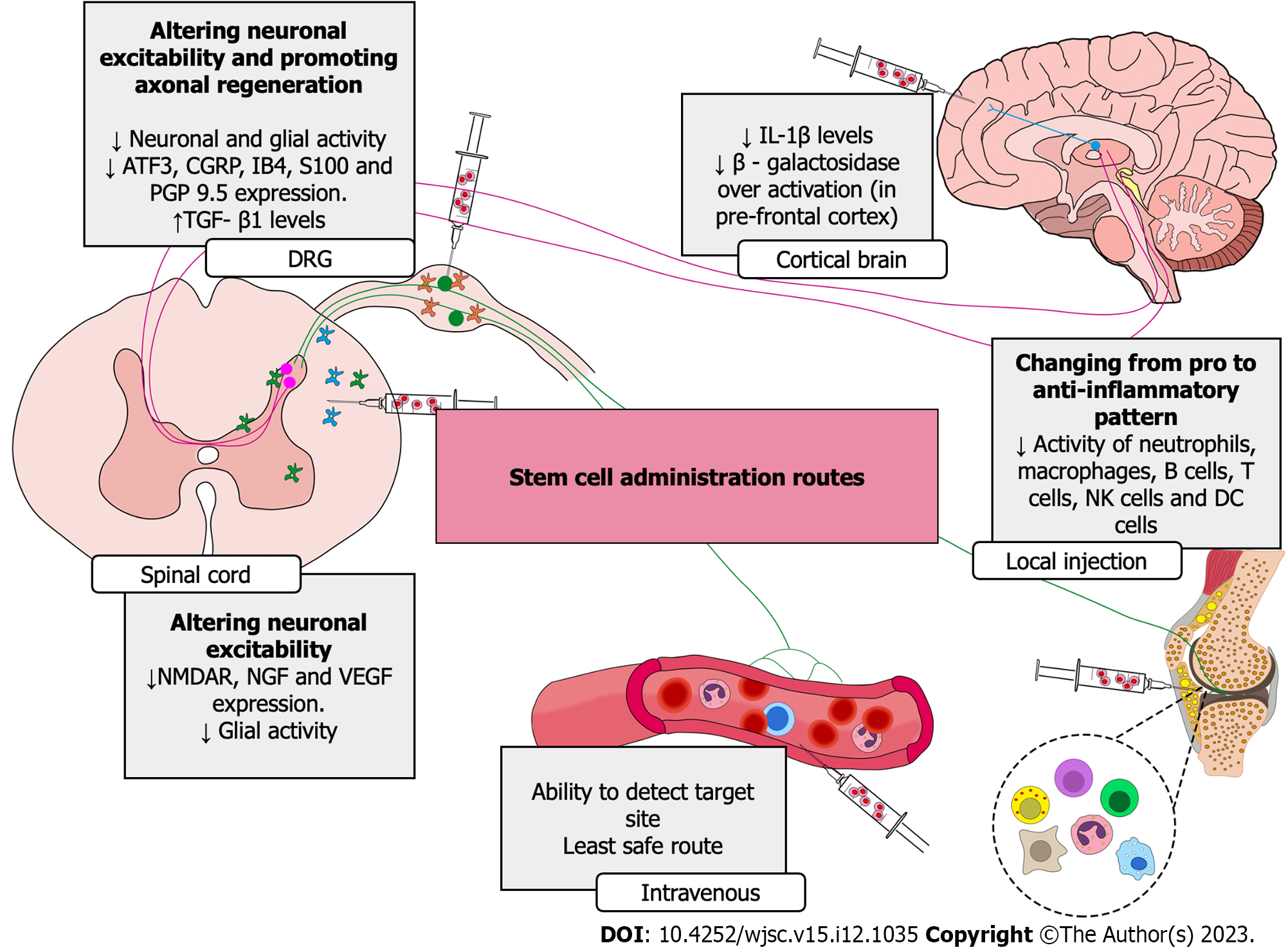
Figure 3 Analgesic mechanisms of stem cells depending on the route of administration and targets/tissues.
This scheme summarizes the mechanistic changes caused by stem cell (SC) treatment that resulted in analgesia. The explanation of analgesic mechanisms of SC treatments in the cerebral cortex, spinal cord, dorsal root ganglia, intravenous and local treatment (intra articulary) (indicated by the syringes) can be observed by up and down arrows plus the changed parameter. ATF3: Activating transcription factor 3; CGRP: Calcitonin gene-related peptide; IB4: Isolectin B4; NMDAR: N-methyl-D-aspartate receptor; NGF: Nerve growth factor; PGP9.5: Protein gene product 9.5; VEGF: Vascular endothelial growth factor; TGF: Transforming growth factor; IL: Interleukin.
- Citation: Silva MDVD, Piva M, Martelossi-Cebinelli G, Stinglin Rosa Ribas M, Hoffmann Salles Bianchini B, K Heintz O, Casagrande R, Verri Jr WA. Stem cells and pain. World J Stem Cells 2023; 15(12): 1035-1062
- URL: https://www.wjgnet.com/1948-0210/full/v15/i12/1035.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v15.i12.1035