INTRODUCTION
Tuberculosis (TB) is a potentially systemic disease that can infect any organ and system. It was a prevalent disease in the developing countries about 50 years ago, but its incidence has been controlled with the availability of effective anti-tuberculous drugs. However, the last decade has witnessed a rise in the incidence of tuberculosis even in developed countries. In the United States, the Centers for Disease Control reported that the incidence of TB was significantly greater in 1994 than in 1985[1]. Nowadays, TB is often an acquired immune deficiency syndrome (AIDS)-defining illness in individuals found to be human immunodeficiency virus (HIV) antibody-positive; however, it can still cause a devastating disease in immunocompetent hosts[1,2]. In China, there is a revival trend in the incidence of TB although AIDS remains uncommon nationally.
Abdominal infection with tuberculosis commonly affects the spleen, liver, and ileocecal region[2,3]. Pancreatic tuberculosis is an extremely rare disease, especially when it is isolated in the pancreas. There were a few case reports published before in literature, but its clinical characteristics remain unclear[4-6]. In this retrospective study, we reported 16 patients with TB of the pancreas and peripancreatic lymph nodes, and summarized the clinical features of 58 similar cases in the Chinese language literature where the HIV antibody status of the patients was either negative or not stated. The clinical, radiographical and laboratory findings, diagnostic methods, therapeutic approaches, and outcome in patients in an endemic area were reviewed in this study.
MATERIALS AND METHODS
The records of 16 patients who were admitted to Hepatobiliary Surgery Center, Southwest Hospital, Third Military Medical University, Chongqing, China with TB of the pancreas and peripancreatic lymph nodes between 1983 and 2001 were reviewed. The clinical, radiographic and laboratory findings, diagnostic methods, therapeutic approaches, and outcome in these patients were summarized. Ten patients were screened for anti-HIV antibodies. Criteria for the diagnosis of pancreatic TB were (1) paraffin-embedded tissues with granuloma or (2) the presence of Mycobacterium tuberculosis DNA by polymerase chain reaction (PCR). IS 6110-specific primers, which could amplify all M. tuberculosis complex strains, were used for amplification. In addition, all available bacteriological and histological studies were performed to confirm the diagnosis. The clinical and laboratory features of patients were collected from the casebooks. Details of follow-up were obtained from medical records. In addition, 58 similar cases published in the Chinese literature were also reviewed and summarized.
RESULTS
A total of 16 patients with TB of the pancreas and peripancreatic lymph nodes had been documented. Six patients were male and 10 were female, with a mean age of 37 years (range 18-56 years). Eight patients had predisposing factors. Six patients had a history of pulmonary TB or TB of lymph nodes, one had diabetes mellitus, and one had connective tissue disease.
Presenting symptoms and physical findings
Predominant symptoms consisted of fever, abdominal pain, abdominal nodule, back pain, jaundice, malaise/weakness, anorexia/weight loss and night sweats. In twelve patients with abdominal nodule and pain, eleven had anorexia/weight loss, ten had malaise/weakness, eight had fever and night sweats, six had back pain, and five had jaundice.
Fever, usually the intermittent type, was present in eight patients. The mean duration of fever prior to the diagnosis was 23 d (range 11-35 d).
Radiographic findings
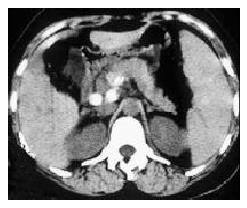
Chest X-rays revealed relic of TB focus in 8 patients, 6 with pneumonitis. All of the patients had been examined with ultrasound and computed tomography (CT) scan. Twelve patients showed swollen head of the pancreas with ultrasound image of heterogeneous attenuation echo. Four patients were demonstrated to have inner heterogeneous attenuation echo in head or body of the pancreas. CT scan showed pancreatic mass with heterogeneous hypodensity focus in all of the patients, with calcification in 9 of 16 patients, and peripancreatic nodules in 6 of 16 patients (Figure 1, Figure 2 and Figure 3). Endoscopic retrograde cholangiopancreatography had been performed for 12 cases, and 2 cases had pancreatic duct dilatation. Magnetic resonance imaging and digital subtraction angiogram had been done for 6 patients, and the results showed pancreatic nodules and/or peripancreatic mass.
Figure 1 Mass with heterogeneous hypodensity located in the head of pancreas.
The body and tail of the pancreas appeared atrophy, and with enlarged main pancreatic duct.
Figure 2 Pancreas appeared swollen diffusely with heterogeneous enhancement and vague margin.
A circle lymph nodes showed enhancement under pancreas.
Figure 3 Calcification of pancreatic TB occurred under the body of the pancreas and retroperitoneal lymph nodes.
Tuberculin skin test
Tuberculin skin test was performed on 9 patients before initiation of therapy. Four in 9 were positive (≥ 10 mm of induration) to 5TU of intradermally purified protein derivative (PPD).
Haematology and biochemistry
In 8 patients, anemia and lymphocytopenia were seen. Pancytopenia occurred in 2 patients. Hypertransaminasemia, elevated alkaline phosphatase (AP) and GGT were seen in 9 patients, respectively. The erythrocyte sedimentation rate (ESR) was elevated in 11 cases.
Results of smears and mycobacterial cultures
Secretions and body fluids were examined microscopically and cultured in 9 patients. Acid-fast bacilli were demonstrated in 1 case, and cultures for M. tuberculosis were positive in 4 out of 9 specimens tested. Anti-TB drug susceptibility was studied in 4 patients, and two M. tuberculosis strains were sensitive to the major anti-TB drugs including isoniazid (INH), rifampin (RMP), pyrazinamide (PZA), streptomycin (SM), and ethambutol (EMB). The other 2 cases were not sensitive to rifampin, isoniazid and streptomycin, respectively.
Biopsy data
Granuloma was found in 12 cases among specimens harvested from the pancreas and peripancreatic nodule by laparotomy (12 of 16) and ultrasound-guided fine needle aspiration (FNA)(10 of 16). Caseous necrosis tissue was found in 6 of 16 cases, and results of smears showed that there were Langhans giant cells, epithelioid cells and lymphocytes. Seven of the 16 patients had combined TB in the liver, bile duct or spleen.
Initial diagnosis
Eleven of 16 patients were initially given a diagnosis of pancreatic tumor. The diagnosis of pancreatic TB had been firstly confirmed for only three of 16 cases. Another three cases were diagnosed with retroperitoneal tumor.
Treatment regimen and outcome
Biopsy and/or FNA were done for all of the patients. Twelve in 16 cases received laparotomy. In one case, cholangiojejunostomy was performed for CBD obstruction, and in another two cases splenectomy was performed for splenic tuberculosis. All 16 patients received treatment with antituberculotics for TB. The most commonly used combinations were INH/RMP/SM (n = 10) and INH/RMP/PZA/SM or EMB (n = 6). The therapeutic duration lasted for a half or one year.
Twelve patients received follow-up from a half to 14 years. No recurrence of TB was found in the pancreas or other organs. In 11 patients, follow-up CT scans in abdomen were available. Resolution was complete in all patients. The mean time to resolution was 132 d (range 78-186 d).
Literature review
A total of 58 cases of pancreatic TB have been described in the Chinese language literature[7-17]. Fifteen of the 58 patients were stated to be HIV antibody-negative, and the HIV status of the other patients was not confirmed. All of the 58 patients were diagnosed by histological appearance being consistent with characteristics of tuberculosis, or positive organisms by acid-fast staining, culture of Mycobacterium tuberculosis or PCR analysis. Twenty patients were male and 36 were female, with a mean age 43.5 years (from 14 to 73). The main symptoms were epigastric pain and discomfort (37 cases), fever (31 cases), weight loss (23 cases) and anorexia (21 cases). The other unusual symptoms included malaise/weakness (11 cases), back pain (9 cases), nausea/vomiting (8 cases), jaundice (6 cases), night sweats (6 cases), upper gastrointestinal bleeding (3 cases), cough (3 cases) and diarrhea (1 case). The duration of symptoms prior to presentation ranged from 5 d to 5 mo (mean 2.6 mo). Thirteen cases gave a past history of TB pneumonia (10 cases) and TB lymph nodes (3 cases). The appearance of the chest X-ray was reported in 49 cases. There was relic of TB focus in 14 patients, 9 with pneumonitis. 34 patients received tuberculin skin testing, of which 21 were positive. Single or multiple modalities of investigation were performed for the patients. Ultrasound revealed pancreatic mass in 38 cases and failed to do so in another 9 cases. Abdominal CT scan was used in 41 cases and reported pancreatic mass and/or peripancreatic nodules in all cases. MRI was performed in 19 cases and also showed a mass in all instances. ERCP found abnormalities with CBD and pancreatic duct in 7 cases. Abdominal X-ray showed focal calcification in 6 cases and DSA located a mass in 4 cases. Ultrasound-guided fine needle aspiration was performed in 21 cases and was successful in diagnosis in 14 cases. Laparoscopic biopsy was performed in 7 cases and confirmed diagnosis in all cases. Fifteen patients had combined TB in other organs.
The initial diagnoses included pancreatic tumor (35), chronic pancreatitis (7), retroperitoneal tumor (5), acute pancreatitis (4) and pancreatic TB (3). Thirty-nine patients underwent laparotomy, 24 for biopsy, 12 for FNA, 5 for pus cavity draining, 4 for choledochojejunostomy, 2 for pancreatoduodenectomy, and 1 for celiac ganglia resection. Pathological report showed granuloma in 27 patients. Acid-fast bacilli were demonstrated in 14 of 27 cases, and cultures for M. tuberculosis were positive in 8 out of 19 specimens tested.
The treatment details were given in 41of 58 cases. The common agents were isoniazid, rifampicin, streptomycin, pyrazinamide and ethambutol. Combinations of 3 or 4 drugs were used for 36 patients. The duration of treatment was recorded in 28 cases, ranging from 3 to 12 mo. 24 patients were reported to have resolution after treatment for 3 to 12 mo. One death was reported among the 58 cases.
DISCUSSION
We have presented a description of a series of 16 cases with tuberculosis of the pancreas and peripancreatic lymph nodes in immunocompetent patients. Having reviewed Chinese literature we found 58 similar cases and summarized their clinical findings. Pancreatic TB is extremely rare. Diagnosis remains difficult for most of the patients, and it is especially difficult to differentiate pancreatic TB from pancreatic tumor. Our series and review of Chinese literature revealed several clinical characteristics as follows: (1) pancreatic TB is mostly suffered by young people, with a predominance of female over male. In contrast, pancreatic tumor is common in old people; (2) some patients have a history of TB in past, and most of them come from areas with high prevalence of active tuberculosis; (3) the patients often present with epigastric pain, fever and weight loss; (4) ultrasound and CT scan show pancreatic mass and peripancreatic nodules, sometimes with focal calcification; (5) FNA and laparoscopic biopsy are the diagnostic procedures of choice for patients with a high suspicion of pancreatic TB. It can lead to confirmed diagnosis and hence avoids laparotomy. Treatment using combination of 3 or 4 antituberculous drugs is effective for most patients. However, attention should be paid to the possibility of drug resistance to some agents that have being used for a long time.
Recently, the incidence of tuberculosis is increasing[1-6]. Cases of pancreatic TB are being reported with increasing frequency, too[18-22]. The reasons may be related to evolutionary changes in the biology of the mycobacterium, drug resistance, and new populations with immunological deficits. Cases related to acquired immunodeficiencies, AIDS or immunosuppression for transplantation have been reported more frequently. Jenney et al[23] had reviewed English language literature before 1998. A total of 37 cases of pancreatic TB in patients not stated to be HIV antibody-positive was found. The authors concluded that it was important to consider the diagnosis of TB when a patient presented with epigastric pain, fever and weight loss and a mass lesion in the pancreas by diagnostic imaging. Three forms of mycobacterial infection of the pancreas have been described as follows: (1) generalized (military) tuberculosis, in which Mycobacterium tuberculosis is the agent; (2) spread to the pancreas from celiac and other retroperitoneal lymph nodes, in which Mycobacterium bovis is the main agent to be considered; (3) primary localized pancreatic tuberculosis due to Mycobacterium tuberculosis, which may reflect a point of origin from the intestinal tract[24-32].
In conclusion, tuberculosis of the pancreas and peripancreatic lymph nodes in immunocompetent patients is rare and could present a diagnostic challenge. However, if doctors are aware of its clinical features and conduct appropriate investigations with multiple modalities including CT scan and ultrasound-guided FNA or laparoscopic biopsy, diagnosis of pancreatic tuberculosis without laparotomy is possible and the disease can be effectively treated with antituberculous drugs.