Copyright
©The Author(s) 2025.
World J Gastroenterol. Aug 28, 2025; 31(32): 108827
Published online Aug 28, 2025. doi: 10.3748/wjg.v31.i32.108827
Published online Aug 28, 2025. doi: 10.3748/wjg.v31.i32.108827
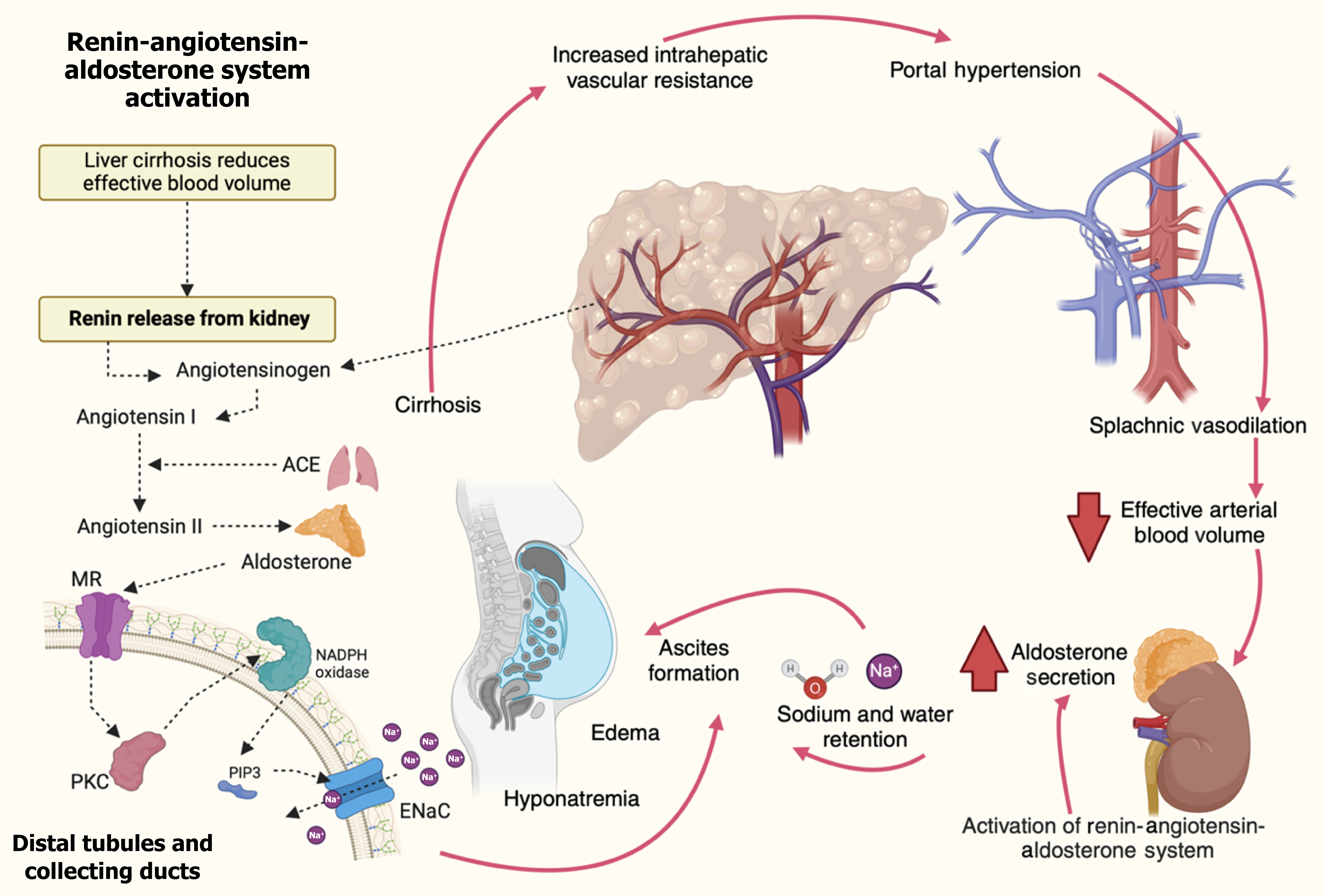
Figure 4 Pathophysiology of secondary hyperaldosteronism in cirrhosis.
Molecular mechanisms drive secondary hyperaldosteronism in cirrhosis. Liver fibrosis increases intrahepatic vascular resistance, causing portal hypertension and splanchnic vasodilation. This reduces adequate arterial blood volume despite normal or increased total blood volume. The kidneys respond by activating the renin-angiotensin-aldosterone system (RAAS), triggering renin release, which converts angiotensinogen to angiotensin I. Angiotensin-converting enzyme converts angiotensin I to angiotensin II, stimulating the adrenal glands to secrete aldosterone. Aldosterone promotes sodium and water retention by activating mineralocorticoid receptors in the distal tubules and collecting ducts. This leads to upregulating the epithelial sodium channels (ENaC) and the sodium ion/potassium ion adenosine triphosphate pump. At the molecular level, aldosterone-induced activation of protein kinase C and phosphatidylinositol-3,4,5-trisphosphate (PIP3) enhances ENaC activity. PIP3 serves as a secondary messenger that facilitates the insertion of ENaC into the cell membrane, promoting sodium reabsorption. Oxidative stress via nicotinamide adenine dinucleotide phosphate oxidase also potentiates ENaC activation and fluid retention. This cascade leads to ascites formation, edema, and hyponatremia. The cycle of portal hypertension, RAAS activation, and sodium retention perpetuates the development of ascites and exacerbates the complications of cirrhosis. ACE: Angiotensin-converting enzyme; ENaC: Epithelial sodium channels; Na: Sodium; MR: Mineralocorticoid receptor; PIP3: Phosphatidylinositol-3,4,5-trisphosphate; PKC: Protein kinase C.
- Citation: Vargas-Beltran AM, Armendariz-Pineda SM, Martínez-Sánchez FD, Martinez-Perez C, Torre A, Cordova-Gallardo J. Interplay between endocrine disorders and liver dysfunction: Mechanisms of damage and therapeutic approaches. World J Gastroenterol 2025; 31(32): 108827
- URL: https://www.wjgnet.com/1007-9327/full/v31/i32/108827.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i32.108827