Copyright
©The Author(s) 2025.
World J Gastroenterol. Aug 28, 2025; 31(32): 108827
Published online Aug 28, 2025. doi: 10.3748/wjg.v31.i32.108827
Published online Aug 28, 2025. doi: 10.3748/wjg.v31.i32.108827
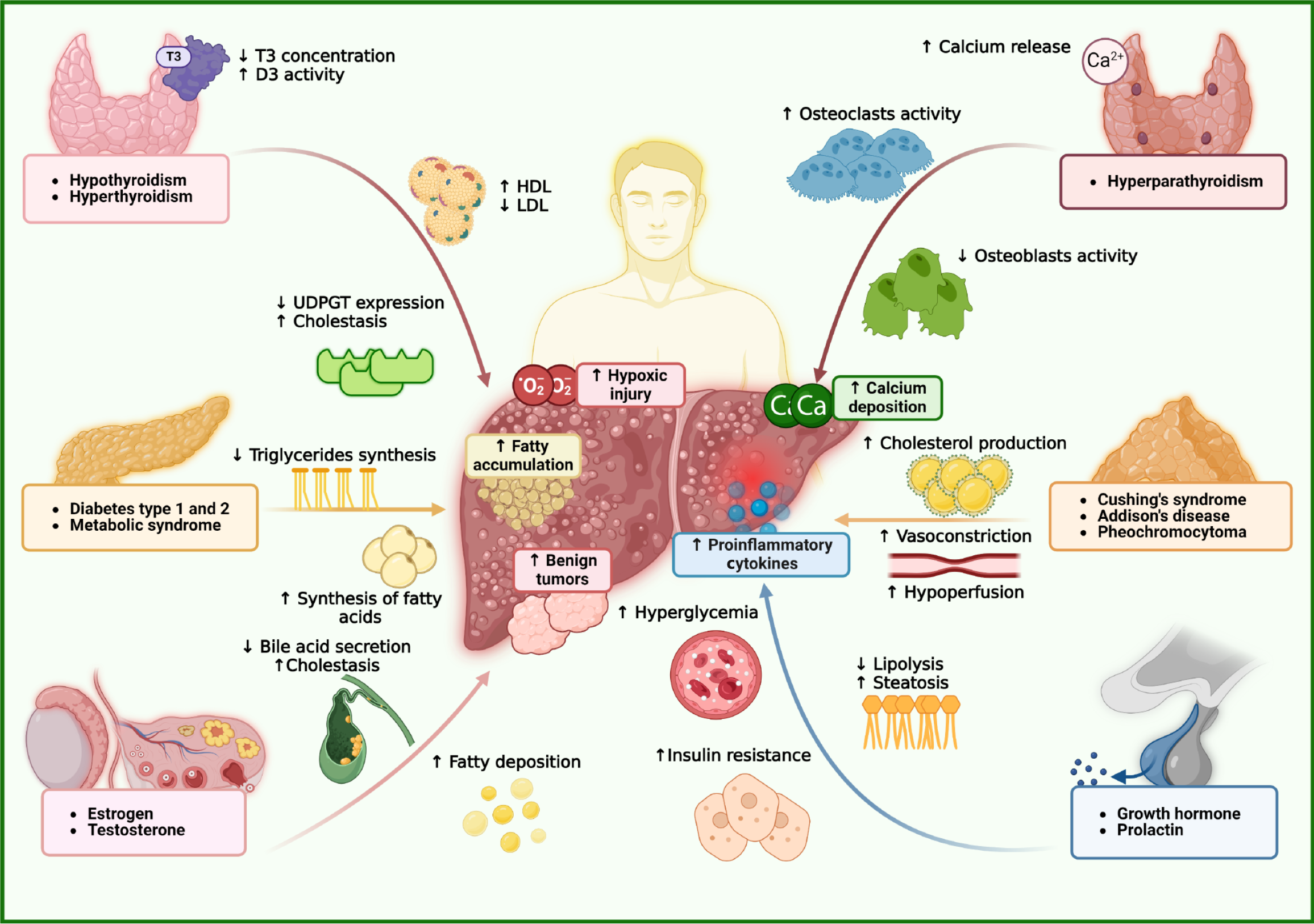
Figure 1 Interactions between endocrine organs and hepatic function.
In hypothyroidism, reduced triiodothyronine levels impair β-oxidation and downregulate uridine diphosphate-glucuronosyltransferase, leading to lipid accumulation and defective bilirubin conjugation, which contribute to cholestasis. Elevated tumor necrosis factor-α and decreased deiodinase activity further exacerbate liver dysfunction. In contrast, hyperthyroidism increases metabolic rate and hepatic oxygen demand, accelerating lipid turnover but inducing hepatocellular injury through oxidative stress and hypoxia. This results in reduced low-density lipoprotein levels and paradoxically elevated high-density lipoprotein, possibly due to increased apolipoprotein A1 synthesis. In adrenal dysfunction, hyperaldosteronism activates mineralocorticoid receptor and epithelial sodium channel, causing sodium retention, ascites, and edema compounded by oxidative stress. Hypercortisolism enhances gluconeogenesis and hepatic lipid accumulation, raising the risk of metabolic dysfunction-associated steatotic liver disease, while adrenal insufficiency impairs anti-inflammatory responses, promoting inflammation. Sex hormones also modulate hepatic physiology. Low testosterone decreases glucose transporter type 4 activity, contributing to insulin resistance and sarcopenia. Increased aromatase activity converts testosterone to estradiol, leading to hyperestrogenism, cholestasis, and benign hepatic tumors. Estrogen signaling through estrogen receptor α offers protective effects by reducing oxidative stress and inflammation, thereby mitigating steatosis and fibrosis. In contrast, growth hormone and prolactin have been associated with increased hepatic steatosis. D3: Type 3 deiodinase; Ca: Calcium; O2: Oxygen; T3: Triiodothyronine; UDPGT: Uridine diphosphate-glucuronosyltransferase; HDL: High-density lipoprotein; LDL: Low-density lipoprotein.
- Citation: Vargas-Beltran AM, Armendariz-Pineda SM, Martínez-Sánchez FD, Martinez-Perez C, Torre A, Cordova-Gallardo J. Interplay between endocrine disorders and liver dysfunction: Mechanisms of damage and therapeutic approaches. World J Gastroenterol 2025; 31(32): 108827
- URL: https://www.wjgnet.com/1007-9327/full/v31/i32/108827.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i32.108827