Copyright
©The Author(s) 2025.
World J Gastroenterol. Jul 28, 2025; 31(28): 108297
Published online Jul 28, 2025. doi: 10.3748/wjg.v31.i28.108297
Published online Jul 28, 2025. doi: 10.3748/wjg.v31.i28.108297
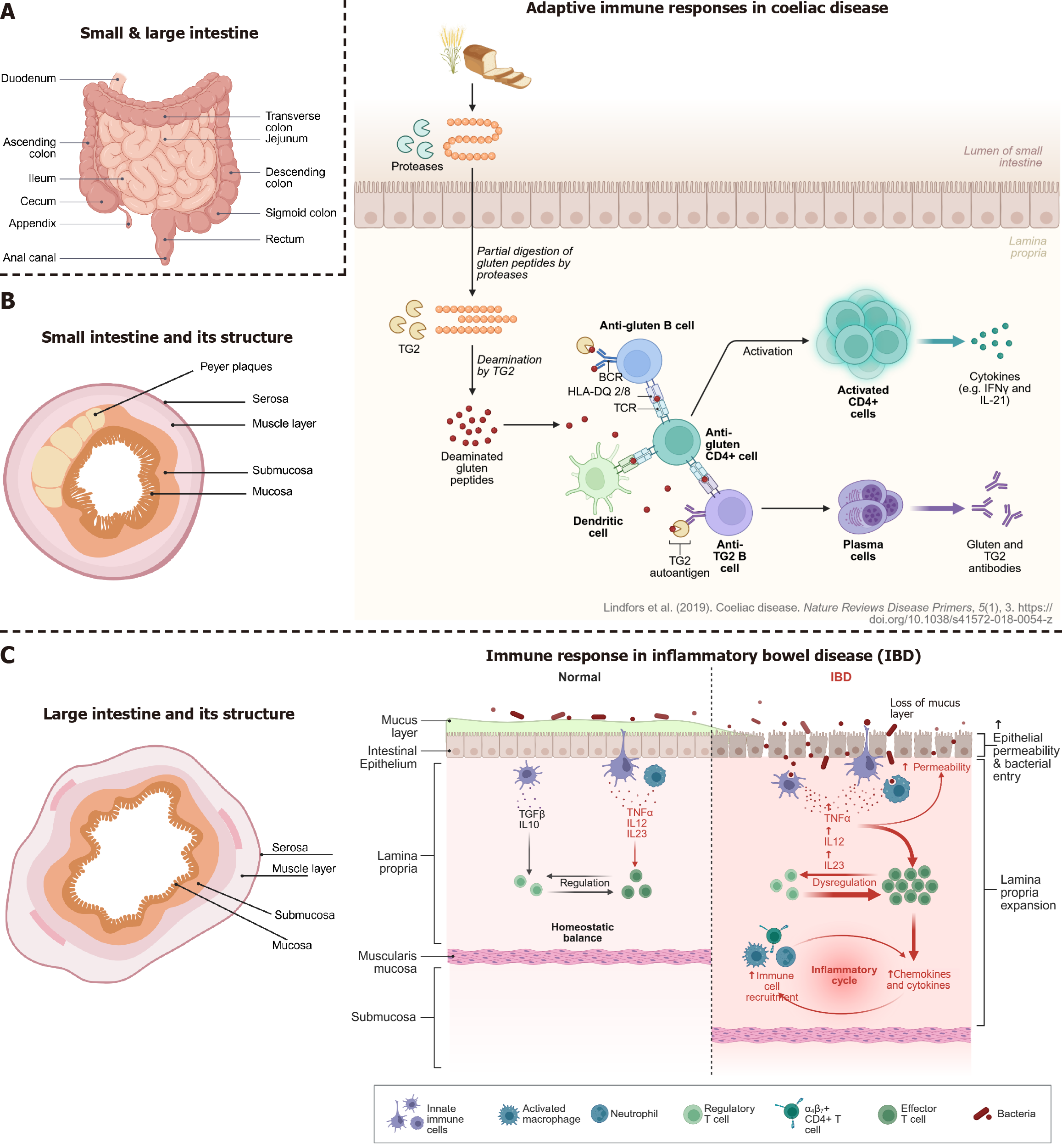
Figure 3 The small and large intestine, their anatomy and diseases overview of intestinal structure and immune responses in coeliac disease and inflammatory bowel disease.
A: Anatomical overview of the small and large intestine; B: Cross-sectional structure of the small intestine, highlighting key layers (left part): Mucosa, submucosa, muscle layer, and serosa, which play roles in barrier function and immune signaling. Peyer’s patches in the small intestine are important sites for immune activation (right part). In coeliac disease, gluten peptides are incompletely digested and deamidated by tissue transglutaminase (TG2), forming neoantigens that are presented to cluster of differentiation 4 + T cells by human leucocyte antigen-DQ2/8 molecules. This leads to T cell activation, B cell maturation, and production of anti-gluten and anti-TG2 antibodies, contributing to tissue damage in the small intestine (left); C: Cross-sectional structure of the large intestine, highlighting key layers: Mucosa, submucosa, muscle layer, and serosa, which play roles in barrier function and immune signaling (middle panel). Under normal conditions, a balanced immune environment in the intestinal mucosa is maintained by regulatory immune cells and intact epithelial and mucus barriers (rightmost panel). In inflammatory bowel disease, disruption of the mucus layer and epithelial barrier allows bacterial translocation, triggering immune dysregulation, recruitment of effector immune cells, and release of proinflammatory cytokines, leading to chronic inflammation.
- Citation: Skok K, Vihar B, Maver U, Gradišnik L, Bräutigam K, Trapecar M, Skok P. Gastrointestinal tract, its pathophysiology and in-vitro models: A “quick” reference guide to translational studies. World J Gastroenterol 2025; 31(28): 108297
- URL: https://www.wjgnet.com/1007-9327/full/v31/i28/108297.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i28.108297