Copyright
©The Author(s) 2025.
World J Gastroenterol. May 28, 2025; 31(20): 100192
Published online May 28, 2025. doi: 10.3748/wjg.v31.i20.100192
Published online May 28, 2025. doi: 10.3748/wjg.v31.i20.100192
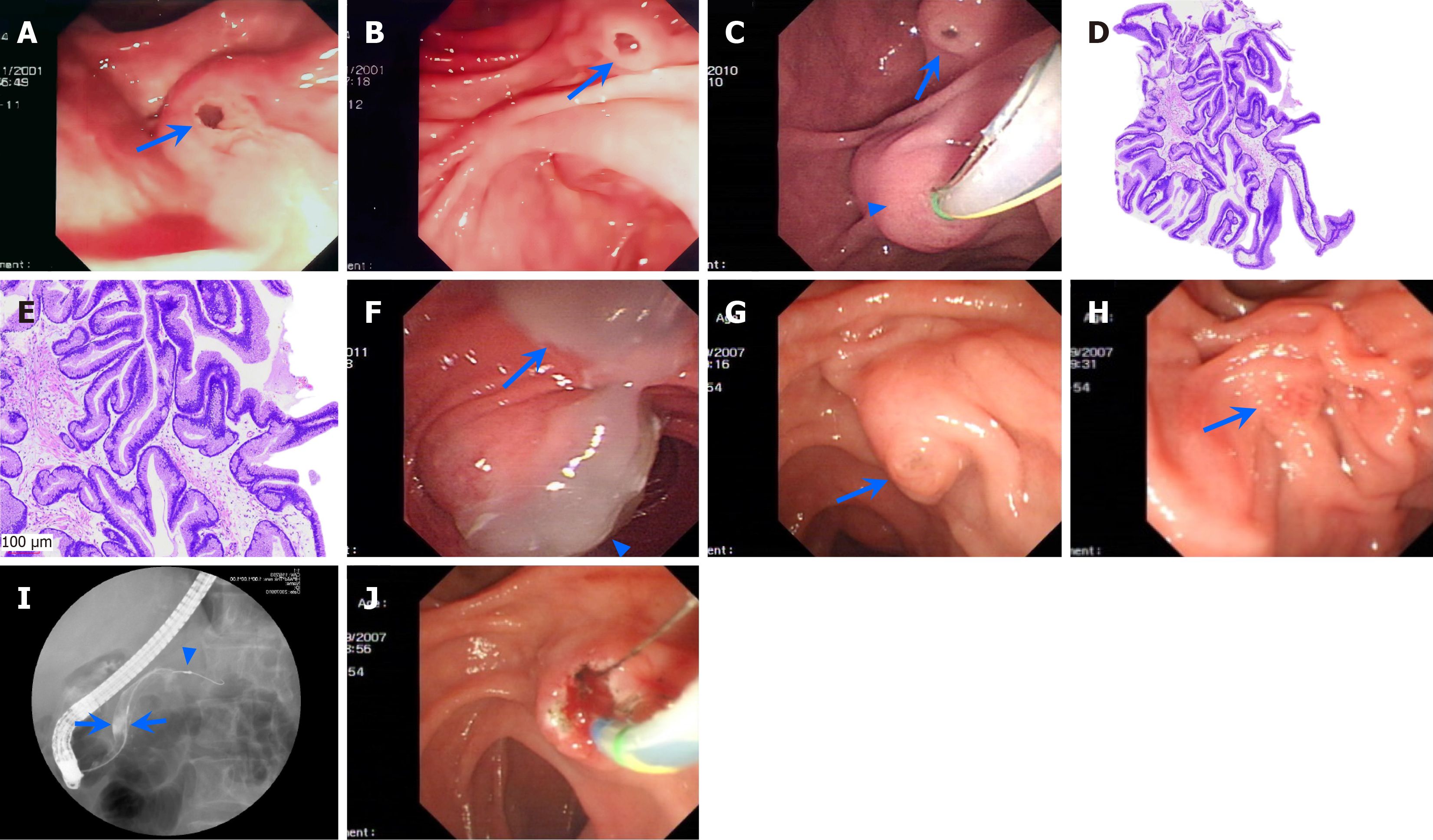
Figure 5 Illustrations of the branch duct-type and main duct-type intraductal papillary mucinous neoplasms in 3 patients.
A and B: Patient 1 with branch duct-type intraductal papillary mucinous neoplasm (IPMN): Duodenoscopy shows the patulous orifice of the major papilla with a fish eye-like appearance (arrow; A), and the patulous orifice of the minor papilla with a fish eye-like appearance (arrow) and mucus flowing out from the orifice before the patient underwent ultra-thin pancreatoscopy via the minor papilla (B); C-F: Patient 2 with main duct-type IPMN: Duodenoscopy shows the enlarged major papilla (arrowhead) with doing deep cannulation (but unsuccessful), and the patulous orifice of the minor papilla (arrow; C), histological examination shows villous papillary architecture composed of pseudostratified tall columnar cells with cigar-shaped enlarged nuclei and basophilic cytoplasm with a large amount of apical mucin, and low-grade and intestinal-type IPMN (hematoxylin and eosin staining, 40 × and 100 ×, respectively; D and E), and a large amount of gelatinous mucous flowing out from both the major (arrowhead) and minor papilla (arrow) 10 months after an endoscopic minor papilla intervention procedure (F); G-J: Patient 3 with main duct-type IPMN: Duodenoscopy shows the enlarged minor papilla (arrow), with mucus visible at the opening (G), the major papilla (arrow) of normal size, with a narrower opening (failed deep cannulation (H), and pancreatic ductography reveals notably dilated (13 mm) dorsal duct (arrows) without filling defects (arrowhead) in the dorsal ducts of the pancreatic body and tail, and the ventral duct (I), and endoscopic minor papillotomy is being performed by using a pull-type papillotome (J).
- Citation: Ren X, Qu YP, Xia T, Tang XF. Technical success, clinical efficacy, and safety of endoscopic minor papilla interventions for symptomatic pancreatic diseases. World J Gastroenterol 2025; 31(20): 100192
- URL: https://www.wjgnet.com/1007-9327/full/v31/i20/100192.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i20.100192