Copyright
©The Author(s) 2025.
World J Gastroenterol. May 28, 2025; 31(20): 100192
Published online May 28, 2025. doi: 10.3748/wjg.v31.i20.100192
Published online May 28, 2025. doi: 10.3748/wjg.v31.i20.100192
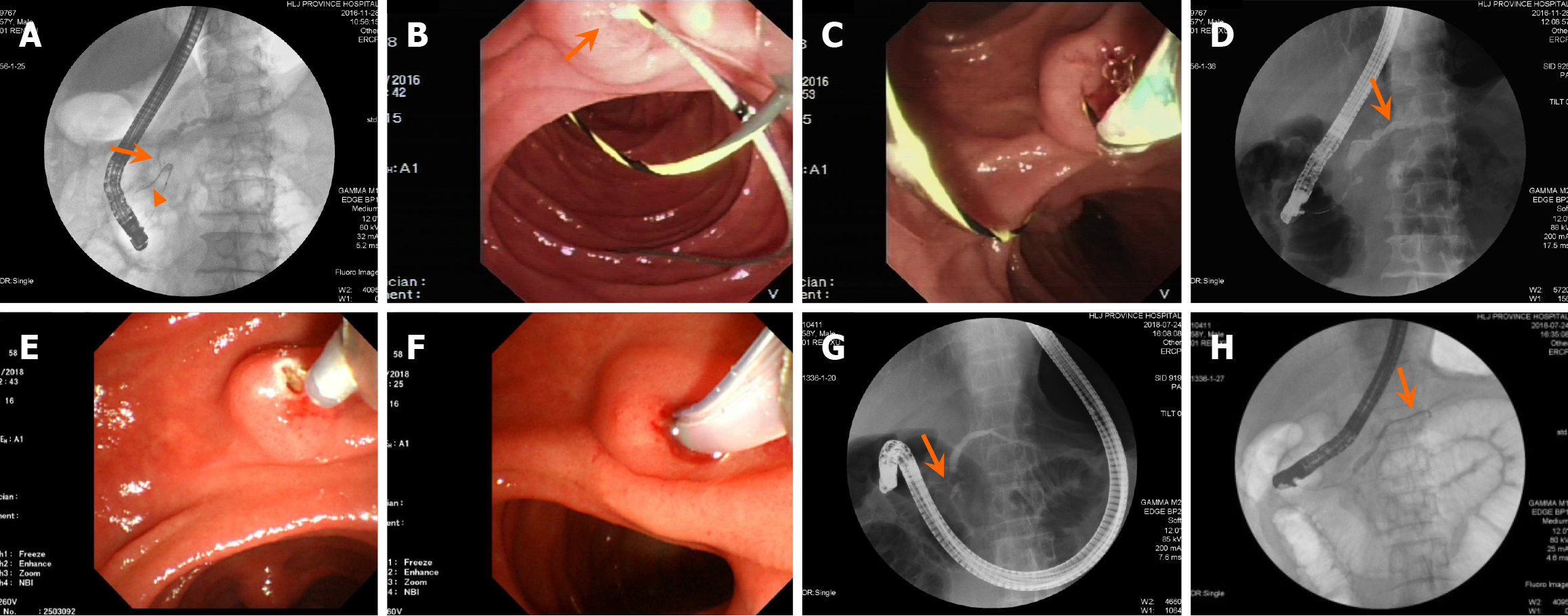
Figure 2 Illustration of the technical success of deep cannulation via the minor papilla in two patients.
A-D: Patient 1 receiving the rendezvous technique: Pancreatography shows the reverse-Z type of the main pancreatic duct (MPD) with a proximal stricture (arrow) of MPD, and the guidewire antegrade into the narrowed accessory pancreatic duct (arrowhead; A); Under duodenoscopy, the guidewire retrogradely enters from the major papilla and antegrade through the minor papilla (arrow) into the duodenum (B); The papillotome is inserted into the minor papilla over the other end of the guidewire pulled back from the biopsy channel (C); Pancreatic ductography demonstrates the guidewire (arrow) adjustment entering upstream of the MPD with successful deep cannulation (D); E-H: Patient 2 receiving additional free-hand needle-knife precut minor papillotomy: Endoscopic view shows the needle-knife precut minor papillotomy in progress (E); The papillotome is inserted into the minor papilla after incisions of the minor papilla (F); Pancreatic ductography displays a short type accessory pancreatic duct (APD) and a proximal stricture (arrow) of MPD, and upstream MPD dilation (G); and The guidewire (arrow) successfully passes through the APD into the upstream MPD, achieving successful deep cannulation (H).
- Citation: Ren X, Qu YP, Xia T, Tang XF. Technical success, clinical efficacy, and safety of endoscopic minor papilla interventions for symptomatic pancreatic diseases. World J Gastroenterol 2025; 31(20): 100192
- URL: https://www.wjgnet.com/1007-9327/full/v31/i20/100192.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i20.100192