Copyright
©The Author(s) 2024.
World J Gastroenterol. Mar 7, 2024; 30(9): 1043-1072
Published online Mar 7, 2024. doi: 10.3748/wjg.v30.i9.1043
Published online Mar 7, 2024. doi: 10.3748/wjg.v30.i9.1043
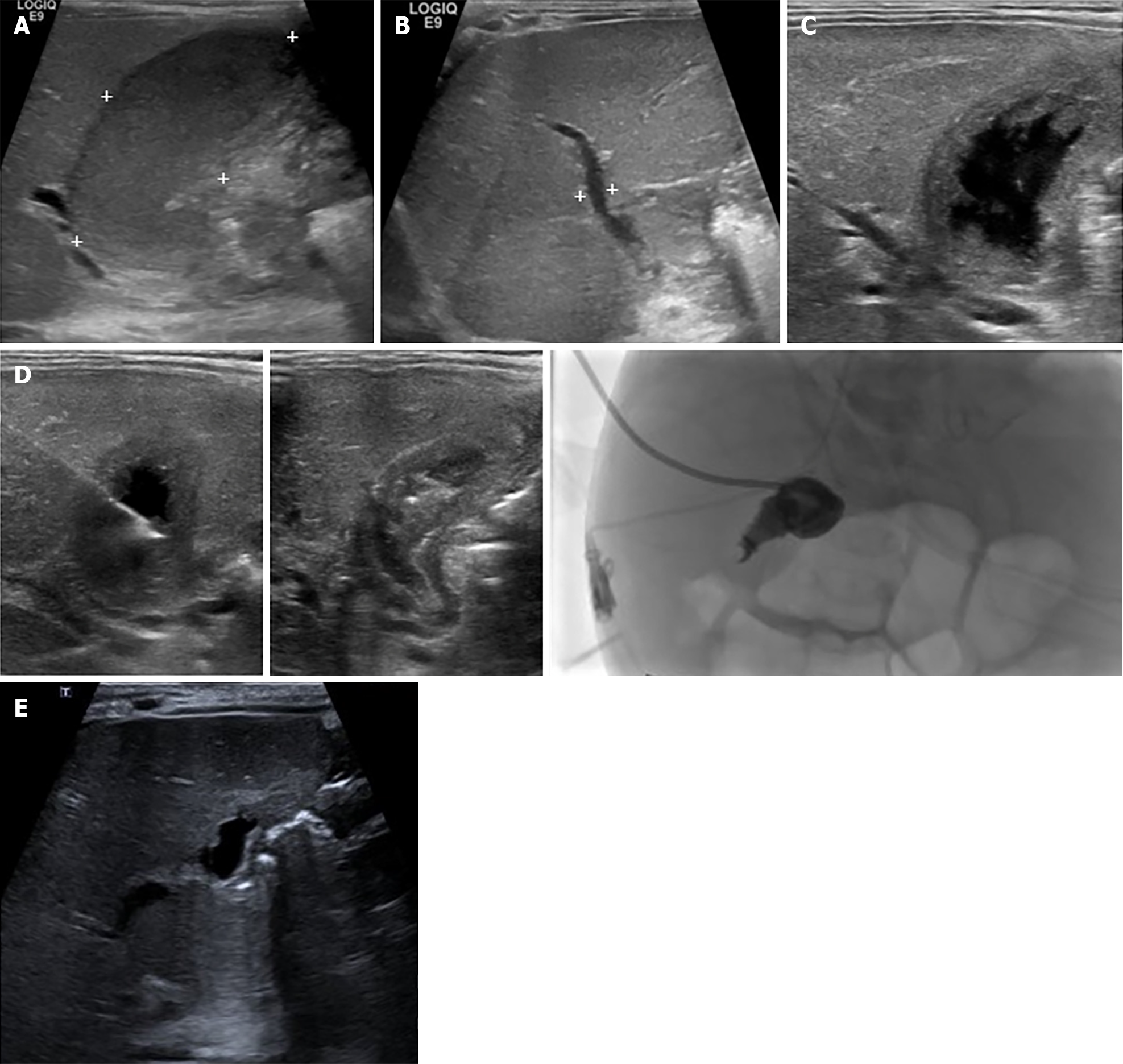
Figure 11 A 30-wk old male infant, with a birth weight of 1130 g, had a short bowel syndrome caused by necrotizing enterocolitis stage IIIB with multiple small bowels, and colonic, and cecal perforations.
He underwent multiple exploratory laparotomies with severe intra-abdominal adhesion. At the age of 3 months, he experienced jaundice and multiple episodes of sepsis. Abdominal ultrasonography revealed a marked distended gallbladder containing bile sludge with mucocele, as hydrops gall bladder, with no bile duct dilatation. The maximum total bilirubmin/direct bilirubin (TB/DB) was 28/23 mg/dL, with unclear sepsis. Percutaneous transhepatic cholecystostomy was performed. After the procedure, sepsis was clear, and TB/DB gradually returned to normal levels within 2 months. Before percutaneous cholecystostomy. A: Hydrops gallbladder 5.4 cm × 2 cm (markedly distended gallbladder with bile sludge); B: Mild dilatation ofz the common bile duct measured 3.2 mm in diameter; C: Percutaneous cholecystostomy via a transhepatic approach; D: A 6-F percutaneous cholecystostomy catheter was inserted over 0.035 Terumo wire with its tip located in the gallbladder. A 5 mL aliquot of dark bile was aspirated; then, a drainage catheter was placed in the gallbladder and connected to the drainage bag and cholecystography was performed; follow-up 1.5 years after percutaneous cholecystotomy; E: Small, lobulated gallbladder.
- Citation: Eiamkulbutr S, Tubjareon C, Sanpavat A, Phewplung T, Srisan N, Sintusek P. Diseases of bile duct in children. World J Gastroenterol 2024; 30(9): 1043-1072
- URL: https://www.wjgnet.com/1007-9327/full/v30/i9/1043.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i9.1043