Published online Sep 15, 1997. doi: 10.3748/wjg.v3.i3.174
Revised: November 16, 1996
Accepted: December 23, 1996
Published online: September 15, 1997
AIM: To investigate the morphologic changes of the myocardium and its relationship to serum bile acids in obstructive jaundice.
METHODS: Part 1: 35 rats were randomly assigned to three groups: Group I (BDL1, n = 11), the common bile duct (CBD) was ligated and severed and mice were then sacrificed after one week. Group I (BDL2, n = 11), the CBD was ligated and severed and mice were then killed after two weeks. Group I (SO, n = 13), the CBD was isolated. Hearts were collected for morphologic studies and blood was taken to determine the total serum bile acids (TAB). Part 2: 13 rats received gastric intubation of 10% 4 mL/kg sodium cholate. Their serum TBA and the heart’s morphologic changes were then examined.
RESULTS: One to two weeks after the CBD was ligated and severed, damage was evident in the mitochondria within the myocardium and the serum TBA was significantly increased. When rats were administered sodium cholate to make their peak blood concentration mimic the average blood concentration in BDL2, a similar degree of myocardial damage was observed.
CONCLUSION: An increase in endogenous bile acids is one causative factor of myocardial damage in obstructive jaundice.
- Citation: Mu YP, Peng SY. Relation between bile acids and myocardial damage in obstructive jaundice. World J Gastroenterol 1997; 3(3): 174-176
- URL: https://www.wjgnet.com/1007-9327/full/v3/i3/174.htm
- DOI: https://dx.doi.org/10.3748/wjg.v3.i3.174
Patients who suffer from jaundice due to extrahepatic biliary obstruction experience high rates of both postoperative complications and death. According to a recent research review, surgery to treat obstructive jaundice has a 10%-25% mortality rate as well as a 56% rate of major complications[1]. It is generally accepted that both cardiovascular instability and predisposition to hypotention and shock are main some of the primary causes for the development of postoperative life-threatening complications such as renal failure. Nevertheless, the mechanism of these postoperative complications remains unclear.
Previous studies on isolated cholemia demonstrated that cholemia might lead to cardiac depression. This result suggested that myocardiac dysfunction causes circulatory failure in jaundice patients[2,3]. The aim of this study is to further investigate whether there is morphologic myocardial damage. Since serum bile acids have detergent properties and are elevated in obstructive jaundice, this study also investigates the relationship between bile acids and myocardial damage.
Part I: 35 male Spraque-Dawley (SD) rats weighing 200-250 g were randomly divided into three groups: group I (BDL1, n = 11), the common bile duct (CBD) was ligated and severed, and rats were sacrificed after one week: group II (BDL2, n = 11), the CBD was also ligated and severed, however the rats were sacrificed after two weeks: group III (SO, n = 13), the CBD was isolated and the rats were sacrificed after one week. When the rats were sacrificed, heart specimens were collected for both light and electron microscopic examination, and blood was taken to determine the total bile acid (TBA) and to perform the biochemical liver function test.
Part II: 13 male SD rats weighing 200-250 g received gastric intubation of 10% 4 mL/kg sodium cholate (Sigma, USA). The changes in both their serum TBA and myocardial morphologies were examined one, two, three, four, and 24 h later.
Specimens for light microscopic studies were fixed in 10% formalin, embedded in paraffin and stained with hematoxylin and eosin (H&E). Specimens for electron microscopic studies were double fixed in osmic acid and glutaraldehyde, stained with uranyl acetate, embedded in EPON-812 epoxy resin, and observed under a Philip EM 412 electron microscope.
Total bile acid (TBA) was determined enzymatically using 3-α hydroxysteroid dehydrogenase.
All results represent the mean ± SD. Means were compared using the Student’s t test. P < 0.05 was considered statistically significant.
Part I: Rats subjected to BDL ligation and severing (BDL groups 1 and 2) had significantly higher serum TB and TAB than the sham operated (SO) group (Table 1).
| SO group | BDL1 group | BDL2 group | |
| TBA(μmol/L) | 60.83 ± 14.8 | 243.12 ± 129.72a | 355.30 ± 238.38ac |
| TB(μmol/L) | 5.37 ± 3.16 | 108.24 ± 38.33a | 80.03 ± 37.62a |
| DB(μmol/L) | 1.71 ± 1.20 | 76.19 ± 26.43a | 57.57 ± 33.45a |
| AKP(u/L) | 29.27 ± 8.96 | 51.49 ± 15.05a | 55.21 ± 18.94a |
| γ-GT(u/L) | 5.77 ± 4.32 | 31.43 ± 20.15a | 31.00 ± 23.87a |
| ALT(u/L) | 49.38 ± 24.53 | 235.57 ± 235.36 | 153.22 ± 148.39a |
| AST(u/L) | 209.46 ± 104.47 | 1112.86 ± 1138.88a | 622.33 ± 536.56a |
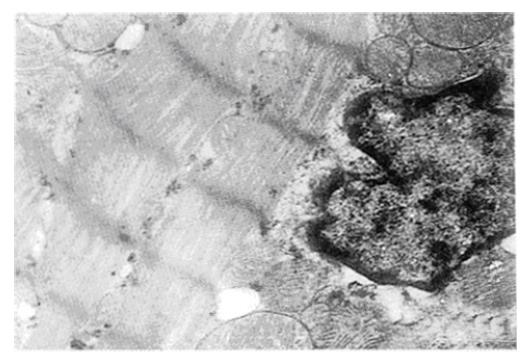
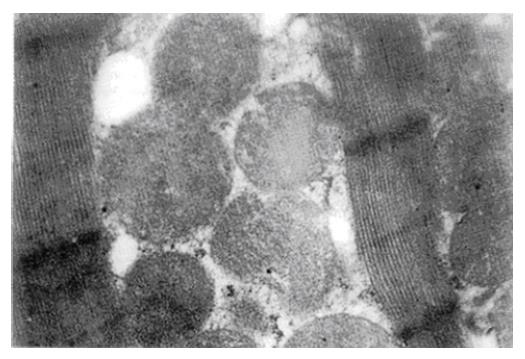
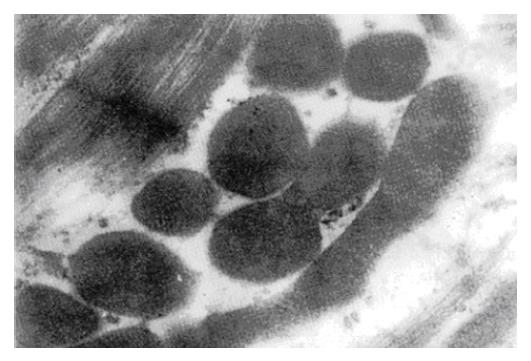
Morphological studies using light microscopy showed that vascular dilation was only evident within the myocardial interstitium for both BDL groups 1 and 2. Using electron microscopy, however, the myocardial mitochondria appeared swollen, decreased and distorted both both groups, with cristae and outer membranes that either looked obscured or had completely disappeared. Nevertheless, the changes seen in the BDL2 group were more obvious than those in the BDL1 group (Figure 1, Figure 2, Figure 3).
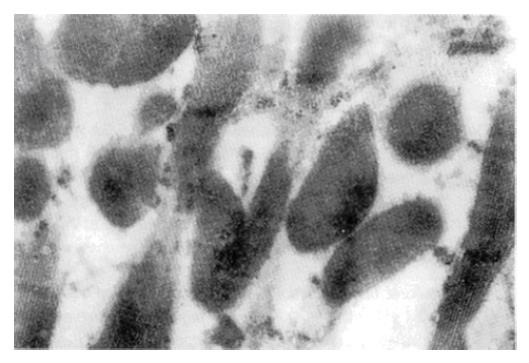
Part II: The serum TBA one, two, three, four, or 24 h following sodium cholate ingestion were 47.7, 132.8, 332.7, 115.0 and 64.3 μmol/L, respectively. The mitochondria in the myocardium appeared swollen and decreased, with cristae and outer membranes that either looked indistinct or had disappeared (Figure 4).
Cardiovascular predisposition and instability to both shock and hypotension have been reported in obstructive jaundice patients. Central and peripheral mechanisms seem to be responsible for increased susceptibility to shock and decreased vascular responsiveness. Recent studies on animal models of isolated cholemia that were induced using choledochocaval anastomosis demonstrated that the mean left ventricular time (LVET) decreased, whereas the mean preejection period (PEP) and mean PEP/LVET were increased. These results suggested that the performance of the left ventricle in isolated cholemia was impaired[2,3]. However, the component of bile that was responsible for this impaired performance remained unclear. It also was unclear whether bile caused any morphological changes within the myocardium.
Bile acids are the chief constituents of bile. Due to its mild detergent properties, it may prove cytotoxic at certain concentrations[4,5]. Since serum bile acids are elevated in obstructive jaundice, it is important to investigate the relationship between bile acids and the myocardial damage characteristic of obstructive jaundice.
This study demonstrates that 1-2 wk after the CBD was ligated and severed, the serum TBA raises significantly and the myocardial mitochondria decrease in number and swell, exhibiting cristae that appear distorted, curled or entirely dissolved. When rats ingested sodium cholate until their peak blood concentration mimicked the average blood concentration in obstructive jaundice, their myocardium was damaged to a similar degree. These results suggest that the myocardial mitochondria was damaged, thus indicating that endogenous bile acids have a significant deleterious effect that contributes to obstructive jaundice.
It remains unclear how the myocardium can protect itself from the damage caused by bile acids. Previous studies in rats demonstrated that ursodeoxycholic acid could limit histologic liver alterations and portal hypertension typically induced by bile duct ligation[6]. Using the hemolysis of erythrocytes as a model of cytotoxicity, Sagawa et al[7] demonstrated that both liposomes and hydrophilic bile acids (such as ursodeoxycholate acid) may protect against hydrophobic bile salt-induced cell membrane damage. We anticipate that the operative mortality and morbidity rates would be decreased if perioperative measures against bile acids toxicity were taken to improve cardiac function[8].
Yi Ping Mou, male, born on May 15, 1965 in Huangyan County of Zhejiang Province, graduated from Wenzhou Medical College and obtained a Bachelors degree in 1986. From 1990 to 1995, under the instruction of Professor Peng Shu You, he was engaged in the diagnosis and surgical treatment of hepatobiliary and pancreatic diseases, the study on the pathophysiology of obstructive jaundice and on the clinical nutriology, and obtained an MD. He is now working in the Department of Surgery, Second Affiliated Hospital, Zhejiang Medical University, and has 15 published papers.
A preliminary report was presented at the 95th China International Meeting on Hapatic, Biliary and Pancreatic Surgery.
Original title:
S- Editor: Filipodia L- Editor: Jennifer E- Editor: Hu S
| 1. | Scott-Conner CE, Grogan JB. The pathophysiology of biliary obstruction and its effect on phagocytic and immune function. J Surg Res. 1994;57:316-336. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 118] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Green J, Beyar R, Sideman S, Mordechovitz D, Better OS. The “jaundiced heart”: a possible explanation for postoperative shock in obstructive jaundice. Surgery. 1986;100:14-20. [PubMed] [Cited in This Article: ] |
| 3. | Zhiwei Q, Qingpei L, Zhewei F. Experimental study on the influence of bstructive jaundice on cardiac function. Acta Universitatis Medicinalis Secondae Shanghai. 1993;13:88-90. [Cited in This Article: ] |
| 4. | Mu YP, Peng SY. The acute and chronic toxicity of bile acids Foreign Medical Sciences. Surgery. 1995;22:76-78. [Cited in This Article: ] |
| 5. | Mu YP, Peng SY. Advance in the studies on the cytotoxicity of bile acids. Foreign Med Sci: Physiol Pathophysio. 1995;15:163-165. [Cited in This Article: ] |
| 6. | Poo JL, Feldmann G, Erlinger S, Braillon A, Gaudin C, Dumont M, Lebrec D. Ursodeoxycholic acid limits liver histologic alterations and portal hypertension induced by bile duct ligation in the rat. Gastroenterology. 1992;102:1752-1759. [PubMed] [Cited in This Article: ] |
| 7. | Sagawa H, Tazuma S, Kajiyama G. Protection against hydrophobic bile salt-induced cell membrane damage by liposomes and hydrophilic bile salts. Am J Physiol. 1993;264:G835-G839. [PubMed] [Cited in This Article: ] |
| 8. | Mu YP, Peng SY. Toxicity of bile acids in obstructive jaundice. Chinese Journal of Practical Surgery. 1996;16:16-17. [Cited in This Article: ] |