Copyright
©The Author(s) 2022.
World J Gastroenterol. Aug 21, 2022; 28(31): 4263-4298
Published online Aug 21, 2022. doi: 10.3748/wjg.v28.i31.4263
Published online Aug 21, 2022. doi: 10.3748/wjg.v28.i31.4263
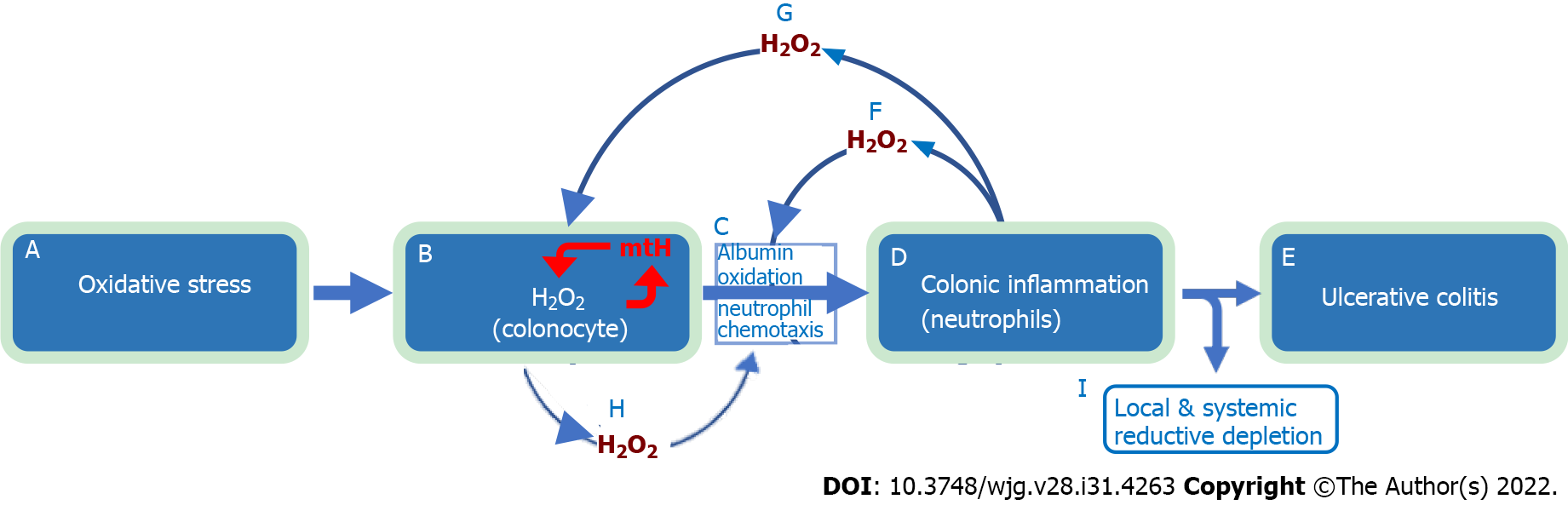
Figure 3 Natural history of ulcerative colitis.
The evidence-based natural history of ulcerative colitis begins with exposure to oxidative stressors (a), which increases colonocyte hydrogen peroxide (H2O2) (b). The increase in colonocyte H2O2 facilitates extracellular diffusion which overwhelms (oxidizes) local interstitial serum albumin antioxidant defense (60% of serum albumin is interstitial), leading to directed migration of neutrophils (chemotaxis) into the colonic epithelium (c) and mucosal inflammation (d) with subsequent development of ulcerative colitis (e). Large amounts of H2O2 are released by neutrophils into the extracellular space (f) with further oxidation of interstitial albumin and exhaustion of tissue antioxidant capacity (c). This worsens colonic inflammation (d) leading to local and systemic reductive depletion (i) as albumin is circulated through the colonic interstitium into tissue lymphatics and back into the systemic circulation. Neutrophil released H2O2 “back flows” into colonocytes (g) adding to the already elevated intracellular H2O2 levels resulting in mitochondrial DNA damage and mitochondrial heteroplasmy (b, red mtH). Mitochondrial heteroplasmy introduces mutations into the electron transport chain protein subunits, which generate additional H2O2 via enhanced electron leakage setting up a vicious cycle of ever increasing colonocyte H2O2 (b, red arrows). Increased colonocyte H2O2 diffuses into the extracellular space (h) causing disease relapse (c, d, e). The combination of local and systemic reductive depletion along with a ready supply of H2O2 from colonocytes and neutrophils (b and d) creates a mucosal inflammation that is self-amplifying, forward propagating, and auto-initiating (relapsing). Elimination of neutrophilic inflammation (d) by any means (i.e., immunosuppressive agents) will not stop relapse from occurring as colonocyte H2O2 continues to diffuse into the extracellular space (c, h). Conversely, normalizing colonocyte H2O2 alone will not stop the inflammation, which has become self-sustaining. This indicates that simultaneous elimination of all pathological sources contributing H2O2 to the inflammatory field must be achieved to ensure long-term remission and normal colonic functionality. Systemic reductive depletion may contribute to other serious health hazards as detailed below. H2O2: Hydrogen peroxide.
- Citation: Pravda J. Evidence-based pathogenesis and treatment of ulcerative colitis: A causal role for colonic epithelial hydrogen peroxide. World J Gastroenterol 2022; 28(31): 4263-4298
- URL: https://www.wjgnet.com/1007-9327/full/v28/i31/4263.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i31.4263