Published online Jul 14, 2022. doi: 10.3748/wjg.v28.i26.3258
Peer-review started: October 27, 2021
First decision: December 27, 2021
Revised: January 4, 2022
Accepted: April 15, 2022
Article in press: April 15, 2022
Published online: July 14, 2022
The correct localization of the primary tumor site and a complete histological diagnosis represent the milestones for the proper management of gastro-entero-pancreatic neuroendocrine neoplasms (GEP-NENs).
To analyze current evidence on the role of endoscopy in the diagnosis/treatment of GEP-NENs.
An extensive bibliographical search was performed in PubMed to identify guidelines and primary literature (retrospective and prospective studies, systematic reviews, case series) published in the last 15 years, using both medical subject heading (MeSH) terms and free-language keywords: gastro-entero-pancreatic neuroendocrine neoplasms; endoscopy; ultrasound endoscopy; capsule endoscopy; double-balloon enteroscopy; diagnosis; therapy; staging.
In the diagnostic setting, endoscopic ultrasonography (EUS) represents the diagnostic gold standard for pancreatic NENs and the technique of choice for the locoregional staging of gastric, duodenal and rectal NENs. The diagnosis of small bowel NENs (sbNENs) has been improved with the advent of video capsule endoscopy and double-balloon enteroscopy, which allow for direct visualization of the entire small bowel; however, data regarding the efficacy/safety of these techniques in the detection of sbNENs are scanty and often inconclusive. From a therapeutic point of view, endoscopic removal is the treatment of choice for the majority of gastric NENs (type 1/2), for well-differentiated localized nonmetastatic duodenal NENs < 1 cm, confined to the submucosa layer and for < 10 mm, stage T1–T2, rectal NENs. EUS-guided pancreatic locoregional ablative treatments have been proposed in recent studies with promising results in order to control symptoms or reduce tumor burden in selected patients.
Standard axial endoscopy and EUS still play a pivotal role in several GEP-NENs. Advanced techniques for increasing the rate of R0 resection should be reserved for high-volume referral centers.
Core tip: Standard axial endoscopy and endoscopic ultrasonography (EUS) play a pivotal role in gastro-entero-pancreatic neuroendocrine neoplasms (GEP-NENs). Upper/lower gastrointestinal endoscopy is essential for the detection of gastrointestinal NENs. EUS represents the diagnostic gold standard for pancreatic NENs and the technique of choice for the locoregional staging of gastric, duodenal and rectal NENs. The diagnosis of small bowel NENs has been improved with the advent of capsule endoscopy and double-balloon enteroscopy, however, their use is limited in clinical practice. In selected localized GEP-NENs, endoscopic therapy is appropriate with radical intent. The multidisciplinary management and the referral to high-volume tertiary centers remain fundamental.
- Citation: Rossi RE, Elvevi A, Gallo C, Palermo A, Invernizzi P, Massironi S. Endoscopic techniques for diagnosis and treatment of gastro-entero-pancreatic neuroendocrine neoplasms: Where we are. World J Gastroenterol 2022; 28(26): 3258-3273
- URL: https://www.wjgnet.com/1007-9327/full/v28/i26/3258.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i26.3258
Gastro-entero-pancreatic neuroendocrine neoplasms (GEP-NENs) represent heterogeneous and rare tumors, whose incidence has been progressively increased in the last decades[1]. The prognosis of these neoplasms is widely variable depending on several factors including the site of the primary tumor, the grading as assessed by the specific WHO classification, and the stage as classified in a specific TNM system[2]. It is therefore clear that the correct localization of the primary tumor site, as well as a complete histologic diagnosis, represent the milestones for the proper management and the prognosis of these tumors[3-5].
In this scenario, despite advances in radiological and metabolic imaging, standard axial endoscopy and endoscopic ultrasonography (EUS) still play a pivotal role in several GEP-NENs. Upper gastrointestinal (GI) endoscopy is essential for the detection and characterization of esophageal, gastric, and duodenal NENs. Ileocolonoscopy allows the assessing and diagnosing of rectal, colonic and rarely distal ileal lesions. Small bowel NENs have proven difficult to diagnose, given their nonspecific presentation and poor accessibility of the distal small bowel to common endoscopic techniques. The diagnosis of small bowel NENs (sbNENs) has been largely improved with the advent of video capsule endoscopy (CE) in 2000 and double-balloon enteroscopy (DBE), the most promising device-assisted enteroscopy (DAE) system, in 2001, which allow for direct visualization of the entire Sb[6]. Finally, EUS is the modality of choice for both diagnosing pancreatic NENs and for the locoregional staging of several NENs, including gastric, duodenal, pancreatic and rectal NENs; of note, in the setting of pancreatic NENs (panNENs), it has demonstrated higher accuracy in tumor detection than other imaging modalities[7].
The present review is aimed at analyzing current evidence on the role of endoscopy in the management of GEP-NENs, with a specific focus on CE and DBE for sbNENs and EUS for the diagnosis and staging of panNENs and other NENs. Furthermore, we summarized available evidence on the role of endoscopy in the radical treatment of selected GEP-NENs.
An extensive bibliographical search was performed in PubMed to identify guidelines and primary literature (retrospective and prospective studies, systematic reviews, case series) published in the last 15 years, using both medical subject heading (MeSH) terms and free-language keywords: gastro-entero-pancreatic neuroendocrine neoplasms; endoscopy; ultrasound endoscopy; capsule endoscopy; double-balloon enteroscopy; diagnosis; therapy; staging. The reference lists from the studies returned by the electronic search were manually searched to identify further relevant reports. The reference lists from all available review articles, primary studies, and proceedings of major meetings were also considered. Articles published as abstracts were included, whereas non-English language papers were excluded.
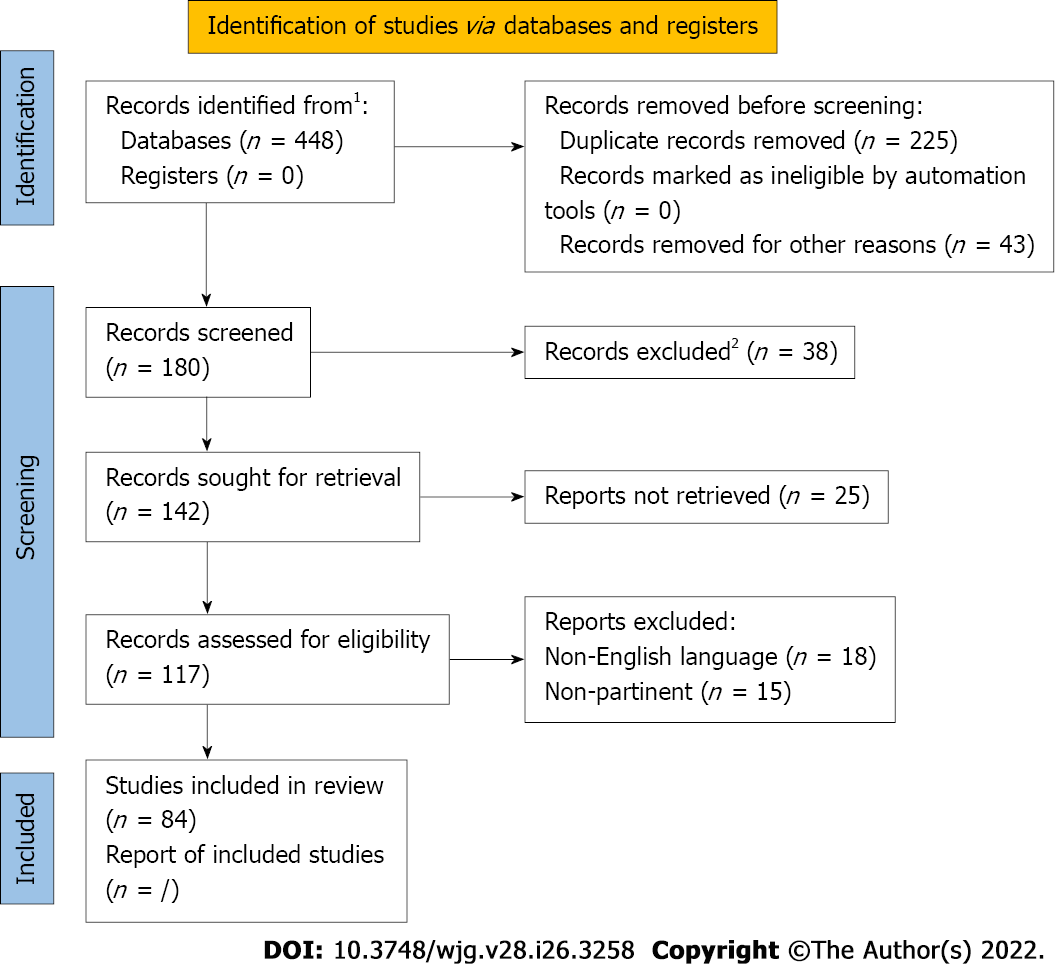
A total of 448 records were reviewed and 84 were defined as fulfilling the criteria for final consideration. Figure 1 presents the flow chart showing the process of study selection.
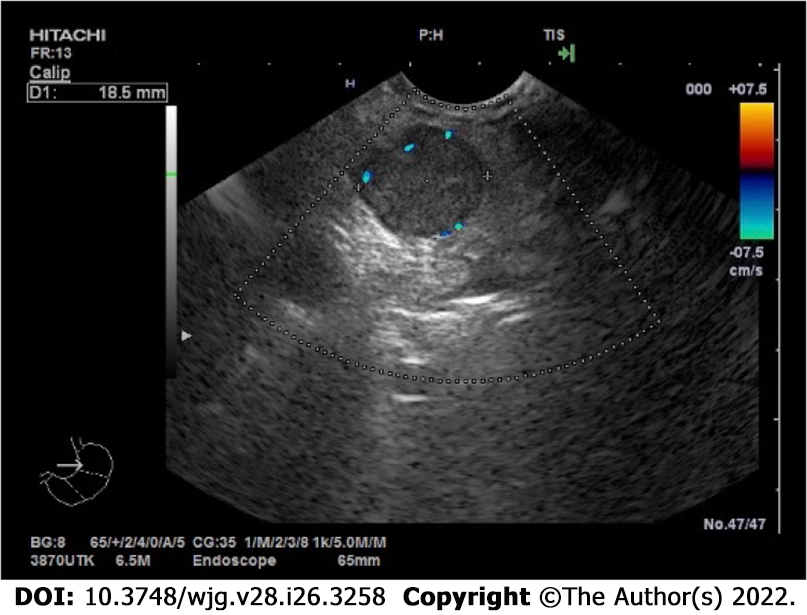
EUS represents the diagnostic gold standard for panNENs and the technique of choice for the locoregional staging of gastric, duodenal and rectal NENs. According to the latest European Neuroendocrine Tumor Society (ENETS) Consensus guidelines, EUS proved to be the most accurate diagnostic technique in panNENs detection, leading to an up-to-94% sensitivity[8]; PanNENs usually appear rounded and homogeneously hypoechoic at EUS examination (Figure 2). EUS sensitivity in detecting panNENs is even higher than noninvasive computed tomography (CT)-scan or magnetic resonance imaging (MRI) pancreatic lesion detection rate[9]. EUS is also extremely accurate in locating the lesions, even very small ones, within the pancreatic parenchyma, and it can describe the distance between the lesion and the main pancreatic duct, which represents an independent predictor of aggressive tumor behavior and of developing pancreatic fistulas[10]. EUS overall complication rate is about 1%–2%, higher for pancreatic cysts rather than for solid masses[11].
Advanced EUS techniques allow to study specific morphological and histological details of the detected lesions that may be helpful in the differential diagnosis of panNENs and in the choice of the corresponding best-suited treatment[7]. Contrast-enhanced harmonic EUS (CH-EUS) allows real-time visualization of parenchymal perfusion and, thus, helps in distinguishing hypovascular carcinomas from hypervascular less aggressive lesions. It consists of harmonic detectors that register microbubbles produced by contrast agents administrated intravenously; this method allows the identification of microvessels even with slow blood flow[12]. As demonstrated for nonfunctioning panNENs, the CH-EUS vascular pattern of neuroendocrine lesions represents an indirect reliable surrogate predictor of their aggressiveness and, thus, of their prognosis; a statistically significant positive correlation was, in fact, proven between the inhomogeneous sonographic pattern of the lesions and their Ki67 proliferative index, which in turn represents the most reliable independent predictor of malignancy. Sonographic heterogeneity at CH-EUS, and especially hypoenhancement in the early arterial phase, corresponds to lower intratumoral microvascular density and to a greater degree of fibrosis on pathological specimens, which were demonstrated to be typical features of tumor aggressiveness on a par with tumor grading[13]. According to a Japanese retrospective study[14], hypoenhancement at CH-EUS proved to be a reliable predictor of tumor aggressiveness and poor prognosis also for G1 and G2 panNENs, with sensitivity, specificity, positive predictive value, negative predictive value and accuracy of 94.7%, 100%, 100%, 96.6% and 97.9%, respectively.
EUS-fine needle aspiration (FNA) is another diagnostic advanced EUS technique, which represents the gold standard least invasive option to obtain the histological identification of a suspected pancreatic neoplasm or peripancreatic lymph nodes, with a sensitivity ranging between 80% and 90% and a specificity of nearly 96%[15] (Figure 3). It is also the operative technique of choice to aspirate the contents of cystic lesions for serological analysis and for the tumor marker dosage, which might help in the differential diagnosis of pancreatic cystic lesions. It can be performed with different diameter needles, mainly depending on the type and site of the lesion, its consistency, and echogenicity. There are several techniques described, which make different use of the suction: some of them suggest not to apply any suction due to the high risk of contaminating the specimen with blood (especially in case of highly vascularized lesions), some others apply wet or dry negative-pressure suction to guarantee sufficient material for histological diagnosis, and others again proposed a slow-pull fanning technique to ensure at the same time a greater collection of pathological cells and a low blood contamination risk[16]; to date, even if still no consensus has been reached on the optimal strategy, overall FNA–EUS sampling adequacy rates up to 94%[17,18] and its diagnostic sensitivity proved to be significantly higher than CT and/or MRI specifically in case of solid, cystic and combined solid-cystic panNENs (84% vs 42%, 70% vs 10% and 81% vs 36% respectively)[19].
The Ki-67 index histological expression of the suspected pancreatic lesion plays a fundamental role in defining the aggressiveness of the tumor, together with its radiological aspect, its localization and distance from the pancreatic duct, and its CH-EUS vascular behavior. Therefore, the Ki-67 index also drives the choice of the best-suited therapeutic approach. Data about the concordance rate between EUS–FNA and surgical specimens in terms of G1, G2 or G3 panNEN and G3 pan-neuroendocrine carcinoma differentiation based on the Ki-67 index are discordant, ranging from a 78% of accordance rate (k-statistic: 0.65)[10], to a relatively significant discrepancy, especially for G2 lesions[20]. This discordance may be first attributed to the fact that endoscopic sampling of large lesions > 20 mm, often included in the studies available to date, may not be representative of the area with the highest concentration of malignant cells and, thus, that the measured Ki-67 index might be not indicative of the most proliferative area of the neoplasm. There is a strong necessity for further studies that subclassify more accurately the included lesions depending on their size.
New EUS needle acquisition techniques (i.e., 19/22/25- G ProCoreTM needle, Cook Endoscopy, Winston-Salem, NC, USA; 19-G fine-needle biopsy, Cook Endoscopy Inc., Limerick, Ireland; Acquire® Endoscopic Ultrasound Fine Needle Biopsy (FNB) Device 22/25-G, Boston Scientific, Natick, MA, USA; SharkCoreTM, Covidien, Dublin, Ireland) have been proposed to overcome the rare cases of EUS–FNA inadequate tissue sampling; these devices are designed to maximize tissue capture and minimize bleeding and tissue fragmentation and some of them are thought to provide both cytological and histological sampling[21]. However, further studies are needed to validate these approaches in the specific setting of NENs.
EUS real-time elastography (EUS–RTE) allows not only a qualitative but also a quantitative assessment of the elasticity of the suspected pancreatic lesion compared to the one of the normal surrounding pancreatic parenchyma. Based on the evidence of higher tissue stiffness in the case of malignant lesions when compared to the normal parenchyma[22], some authors have proposed different quantitative elastography cutoffs to stratify the risk of malignancy. Havre et al[23] observed a EUS–RTE sensitivity of 67% and specificity of 71% in detecting pancreatic malignant lesions with a strain ratio cutoff of 4.4. Iglesias-García et al[24] showed an EUS–RTE sensitivity of 100% and specificity of 88% in differentiating specifically pancreatic adenocarcinomas from panNENs with a 26.6 strain ratio cutoff value. Even if, according to the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) guidelines, EUS–RTE cannot yet replace the histo-cytopathological diagnosis of carcinoma[25], this technique may facilitate the differentiation from benign to malignant pancreatic lesions.
Another advanced technique in EUS that can drive in the diagnostic orientation is represented by the needle-based confocal laser endomicroscopy, which allows the real-time direct in vivo visualization of the histological aspect of the GI mucosa overlying pancreatic NENs, which is traditionally described as clusters of compact cells on a dark background surrounded by numerous small and irregular vessels and fibrotic areas[26]. Giovannini et al[27], observed a negative predictive value of 100% for the characterization of pancreatic NENs in EUS needle-based confocal laser endomicroscopy; therefore supporting the concept that it cannot be considered as an alternative to the histological diagnosis, but that it may help to rule out malignancy.
Further applications of EUS in panNENs is represented by the preoperative EUS-guided fine-needle tattooing and EUS-guided fiducial implantation, which may help surgeons find little pancreatic lesions during laparoscopic surgery, limiting the laparoscopic resection to the lesion itself, sparing the normal surrounding parenchyma, and reducing the operating time[28].
As regards GI-NENs, EUS mainly plays a diagnostic and staging role; its sensitivity in detecting GI-NENs is up to 94%[29]; they usually appear as submucosal rounded, hypoechoic, well-demarcated lesions and can be detected when smaller than 10 mm, especially rectal NENs thanks to the growing sensibility to colorectal carcinoma screening. According to the ENETS most recent guidelines, in case of the endoscopic identification of a GI lesion that is compatible with a GI-NEN, EUS is recommended in case of lesions > 10 mm in order to study the depth of the lesion, to stage the hypothetical presence of locoregional lymph nodes and, thus, to drive the choice of the most appropriate endoscopic or surgical treatment[30]. Less than 10 mm GI-NENs, in fact, have a low risk of both lymphatic invasion and distant metastases, which is reported to be 1%–2%[31]. GI-NENs measuring 10–19 mm at their first endoscopic diagnosis deserve more accurate EUS evaluation because of the reported higher incidence rate of lymph node invasion or distant metastases, leading up to 5%–15%[32]. If the GI-NEN is limited to the submucosa and does not invade the muscularis mucosae (which corresponds to a T1 lesion), regardless of its lateral spreading, a simple en bloc endoscopic resection treatment has proved to be effective in guaranteeing a radical resection and a very limited recurrence rate during the follow-up[33], otherwise, a surgical approach is suggested. T2 or N+ stage lesions should be accurately studied with total body imaging such as 68-Ga-DOTATATE positron emission tomography (PET) and a CT scan in order to plan the best therapeutic approach.
The small intestine is the most common NEN site in humans. Historically, sbNENs have proved difficult to diagnose because of both the lack of specific symptoms at presentation and the poor accessibility of the distal small bowel[34]. Conventional radiology (both CT and MRI either in the standard technique or in combination with enteroclysis) are often not accurate enough in the detection of sbNENs[35], whereas PET/CT with 68Ga-DOTA peptides remains the most sensitive modality in the detection of well-differentiated NENs, although it does not allow to get a histological diagnosis and might not be fully accurate in the anatomical location of the primary tumor being, for instance, unable to differentiate between intestinal and mesenteric localization[36]. Furthermore, in the case of metastatic disease, the detection of the primary tumor is recommended in both resectable and non resectable diseases. However, in up to 10% of the cases after the discovery of liver or lymph node metastases, the primary tumor site remains unknown despite an extensive workup[35].
With the advent of CE and DBE the diagnosis of sbNENs has improved, even if data regarding the efficacy and safety of these techniques in the detection of sbNENs are scanty and mainly based on small retrospective series, given the rarity of the disease and the still-limited use of these techniques in routine clinical practice. Most of the available studies are focused on small bowel tumors in general and only a small percentage of included patients displayed an sbNEN[37-39]. In a study comparing CT, enteroclysis, nuclear imaging, and CE of the small bowel[34], CE showed a high diagnostic yield (45%) in identifying primary tumors. Of note, in 12 of 20 patients (60%), CE showed small-intestinal lesions that were then confirmed histologically as NEN in six of seven patients who underwent surgery.
When considering the few studies specifically focused on NENs, the results came back to be inconclusive. In a retrospective study by Frilling et al[40], including 390 patients with metastatic NENs of whom 11 with unknown primary tumor, CE identified lesions suggestive of small bowel primary in 8/10 patients in whom it was successful, and these tumors were all histologically confirmed. In a recent prospective study[41], the diagnostic yield of CE was reported to be limited. In 24 patients with a histological diagnosis of metastatic NEN of unknown origin, CE, which was preferred to DBE as less invasive and less expensive, was requested before explorative laparotomy and its diagnostic yield was compared to the surgical exploration. CE identified a primary sbNEN in 11 subjects. However, diagnosis of sbNEN was confirmed only in five (41%) cases after surgical and ultrasound exploration were performed. The high number of false-positive results could have been related to small bowel contractions, extrinsic compression, lymph stasis, or submucosal lesion of another type.
Although CE is less invasive, DBE is necessary for determining the precise location, number of tumors, and pathological diagnosis; it can be carried out through the oral (antegrade) or the anal (retrograde) route and with a combined oral and anal approach[42]. Bellutti et al[43], in a study involving 12 consecutive patients with suspected sbNEN or with liver NEN metastases, who underwent DBE, found a diagnostic yield of DBE for primary tumor of 33%. In a case series by Scherubl et al[44], five consecutive patients with metastatic midgut carcinoids underwent DBE and an NEN of the ileum was detected in four of the five patients; the histopathological evaluation of their biopsy specimens confirmed the diagnosis revealing well-differentiated NENs. Conversely, conventional radiological imaging did not visualize any of the primary tumors.
In our recent prospective study[45], we reported sensitivity and specificity of 60% and 100%, respectively for DBE in detecting sbNEN in six patients with unknown primary, showing that DBE is a safe and effective procedure in diagnosing sbNENs. We suggested that when a sbNEN is suspected, DBE should be taken into account as an accurate diagnostic tool in order both to collect biopsies for final diagnosis and to make tattoos before surgery; of note, DBE should be preferred over CE in the presurgical setting given the high specificity. Considering the limited available data, further studies are needed to better define the actual role of CE and DBE in the diagnosis of sbNENs.
Gastric NENs (gNENs) are usually subclassified into three types, according to their pathophysiology and behavior[29,46]. Type I tumors correspond to the majority of gNENs (~80%) and are associated with autoimmune atrophic gastritis. Histologically, type I gNENs are composed of enterochromaffin-like cells. The diagnosis is made by upper digestive endoscopy with biopsy. The majority of type I gNENs present as small, multiple tumors, located in the gastric body or fundus, and limited to the mucosal or submucosal layers of the stomach wall[46,47]. Since the risk of metastasis is < 5% in type I gNENs, a conservative approach based on endoscopic follow-up with lesion resection is advised for this kind of tumor. The treatment of choice for type I gNENs is endoscopic resection for lesions > 0.5 cm and endoscopic surveillance for lesions < 0.5 cm[46,48,49]. This approach has been shown to be safe and effective in a prospective series of 33 type I gNENs, with no significant procedure-related complications, no development of metastases, and a 100% long-term survival rate[50].
The ENETS guidelines[29] suggest performing EUS in case of lesions > 1 cm. Staging EUS is frequently performed to confirm the appropriateness of endoscopic resection, which applies to lesions not infiltrating beyond the muscularis propria[7]. For lesions > 1 cm, EUS is excellent for determining the exact tumor size and for excluding infiltration of the type I gNENs into the muscularis propria (T2) or enlarged regional lymph nodes[47,51].
Type II gNENs correspond to 5%–10% of gNENs; they usually develop when multiple endocrine neoplasia type 1 is present and are often associated with Zollinger–Ellison syndrome[46,48]. Like type I gNENs, type II gNENs originate from enterochromaffin-like cells. They are small, multiple, and relatively benign tumors, even though about 10%–30% of patients present as metastatic at the diagnosis[52]. For type II gNENs local excision is recommended, preferentially by endoscopy; as well as for type I gNENs, EUS plays a pivotal role in determining the tumor size, lymph node involvement, and depth of invasion; endoscopic treatment is again reserved for lesions not infiltrating beyond the muscularis propria, without lymph node involvement[7,53].
Type III gastric NENs are usually larger sporadic tumors with an infiltrative and metastatic tendency and account for 15% of all gNENs. They are generally characterized by being single lesions, > 1 cm and with a greater likelihood of evolving to regional and systemic metastases, as more than half of patients with type III gNENs are metastatic at diagnosis, mainly to the liver[46,48]. From a therapeutic point of view, surgery is the standard treatment, i.e., total or subtotal gastrectomy together with lymphadenectomy, as recommended in gastric adenocarcinoma. For patients with any surgical contraindication, endoscopic resection may be an alternative, but the risk of regional lymph node spread remains high[46]. Of note, in selected cases of small (< 1 cm) type III G1/G2 (Ki-67 < 5%) gNENs fully resected (R0) by endoscopy with no risk factors for metastatic disease, endoscopic resection might be sufficient[54]. As for other gNENs, EUS is a useful tool for locoregional staging, particularly to stage the disease by assessing the presence of regional lymph node involvement.
Conventional polypectomy with a snare for flat mucosal lesions should be avoided because complete resection is often not achieved. Early gNENs are generally removed by endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD)[47,54]. In EMR, snare resection is preceded by the submucosal injection of saline in order to raise the tumor and cut into the submucosa below the tumor[47]. ESD is preferred over EMR in case of suspicion of limited submucosal invasion or a tumor > 2 cm[55]. After submucosal injection of saline, the submucosa is dissected with specific knives in order to achieve endoscopic en bloc resection of the whole neoplasm.
The resected specimen has to be carefully evaluated regarding grade, angioinvasion, and infiltration of the deep resection margin. In case of angioinvasion, histological infiltration of the muscularis propria (T2), or grade G2/G3, radicalization with surgery with lymph node dissection is the therapy of choice in localized neuroendocrine disease[47].
Duodenal NENs (dNENs) are rare, usually small well-differentiated tumors in most of the cases; however, according to a recent multicenter retrospective study[56], dNENs’ prognosis may be highly variable as these tumors can be metastatic in up to 50% of the cases at the time of first diagnosis and can develop metastases thereafter. Upper GI endoscopy with biopsy is necessary for dNEN diagnosis and EUS should be performed to assess the local extent of tumor depth.
In view of this heterogeneous behavior, surgical resection has been suggested as the preferred treatment modality over endoscopic treatment, and surgery is generally recommended for ampullary dNENs and lesions > 2 cm in size[38]. Endoscopic resection is the treatment of choice for well-differentiated localized nonmetastatic tumors with a diameter < 1 cm and confined to the submucosa layer and the rationale for preferring the endoscopic treatment for tumors < 1 cm relies on the fact that they seem to have a low rate of nodal disease[57]. In this setting, there is no current evidence to prefer an endoscopic approach over another as prospective studies comparing the available techniques (i.e., ESD vs EMR) are lacking.
However, there is still controversy regarding the management of tumors between 1 and 2 cm, which is mainly based on the tumor location and the presence of nodal involvement on imaging. According to some authors, > 10% of patients with dNENs < 1 cm in size develop lymph node metastases, thus suggesting the need for a radical surgical approach for all dNENs despite the size of the primary tumor[58-60]. Another issue to be taken into account is the high risk of conventional and functional imaging of understaging mainly due to the presence of nodal and distant micrometastases[60]. These results represent a sign of warning for conservative approaches including endoscopy, suggesting as a possible strategy, the inclusion of EUS in the preoperative phase, although prospective studies are necessary to draw solid conclusions.
In summary, all considered, endoscopic resection either EMR or ESD should be reserved for dNENs < 10 mm, limited to the submucosal layer without evidence of lymph node or distant metastases, whereas surgery might be advised for dNENs > 10 mm with evidence of muscular layer invasion or nodal involvement. EUS should be encouraged for all dNENs in order to plan the best therapeutic approach.
Endoscopic treatment for rectal NENs (rNENs) is indicated if there is no evidence of invasion beyond submucosa and presence of locoregional disease since it aims to achieve a complete oncological resection[61].
The ENETS guidelines[30] suggest that well-differentiated (G1/G2) rNENs that are < 10 mm in stage T1 and T2 and rNENs between 10 and 20 mm in stage T1 without lymph node metastasis should be removed endoscopically. On the contrary, surgical resection is indicated in cases of G3 rNENs, 10–19 mm with muscolaris propria invasion (stage T2) and for tumors > 20 mm and/or in presence of lymph node metastases.
Endoscopic techniques for treating rNENs include standard polypectomy, EMR, modified EMR, ESD, and endoscopic full-thickness resection (EFTR). Standard polypectomy does not offer an adequate and complete resection of the lesion; therefore, it is not indicated in rNEN treatment[62]. Of note, a large number of rNENs is still removed by an improper method, such as routine snare polypectomy, during colorectal cancer screening making management more complex and putting patients at risk of metastatic spread[63].
EMR is largely used in the resection of small and superficial neoplasia confined to the mucosa and submucosal layer, but its application in rNENs is still debated since modified EMR and ESD are superior in terms of en bloc resection rate and histological complete resection rate (defined as en bloc resection with no margin involved)[64,65].
Recently, Park et al[66] observed that when EMR is performed underwater, the histological complete resection rate of NENs < 10 mm is similar to that for ESD (86.1% vs 86.1%, respectively) but with a shorter procedure time (5.8 ± 2.9 vs 26.6 ±13.4 min, respectively).
EMR performed with a dual-channel endoscope allows deeper resection compared to conventional EMR by lifting the lesion with forceps. Lee et al[67] observed that dual-channel EMR reaches a complete histological resection rate similar to that of ESD for rNENs < 16 mm (86.3 vs 88.4 %, respectively), but with a shorter procedure time (9.75 ± 7.11 vs 22.38 ± 7.56 min, respectively) and fewer complications.
Modified EMR techniques include the use of special devices that allow better resection of the tumor. EMR after circumferential precutting (EMR-P) is performed by lifting the submucosal with saline injection, precutting using the tip of the snare or special endoknife and resecting the tumor with a snare. Cap-assisted EMR (EMR-C) is performed by lifting the mucosa with saline injection, suctioning the lesion with a transparent cap fitted to the scope and then removing it with a snare looped along the ridge of the cap. EMR with a ligation device (EMR-L) is conducted by lifting the lesion with saline injection, deploying an elastic band around its base, and resecting with a snare. Histological complete resection rate for EMR-P is superior to EMR and no difference was found between EMR-P and the other modified EMR techniques, even if it required a longer procedure time[68]. Park et al[69] demonstrated that EMR-C is a safe and effective technique for rNENs, with a histological complete resection rate even better than that of ESD (92.3% vs 78.4%, respectively).
EMR-L is only applicable for tumors of < 10 mm due to the short diameter of the caps fitted to colonoscopes, but it is significantly superior to EMR in terms of complete resection of rNENs (93.3% vs 65.5%, respectively), regardless of the tumor location[70]. Histological complete resection rate is similar between EMR-C and EMR-L. However, Lee et al[71] demonstrated that EMR-L might be preferable for achieving a higher rate of en bloc resection (100% vs 92.9%, respectively), but this could be due to the fact that the band thickness used in EMR-L is larger than the snare thickness of EMR-C.
ESD is an interventional procedure suitable for en bloc resection of slightly invasive GI lesions. After injection of the submucosal with a viscous solution, an endoknife is used to incise the mucosa surrounding the lesion and to dissect it from the submucosal layer. ESD is an effective technique to treat rectal lesions, even if it is associated with a high risk of complications and a long procedure time. As it concerns rNENs, ESD has been demonstrated to be superior to EMR in terms of histological complete resection rate, but there are no significant differences between ESD and modified EMR[70].
Niimi et al[72] observed that ESD is associated with a longer procedure time and hospitalization period compared with EMR-L, with a similar complete resection rate. In order to reduce procedure time, Wang et al[73] proposed a hybrid ESD, in which the mucosal incision is performed with a polypectomy snare instead of an endoknife. This technique showed a similar en bloc resection rate (99.2% vs 98.2) and complete resection rate (94.1% vs 90.9%) to ESD but with a shorter procedure time (13.2 ± 8.3 vs 18.1 ± 9.7 min).
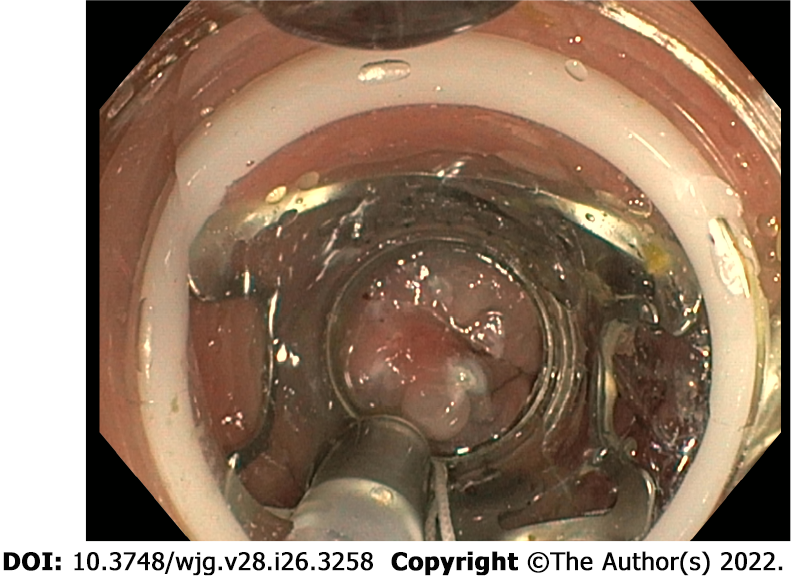
EFTR is a technique mainly used in lesions that are difficult to resect and its application in rNENs has recently been proposed. A full-thickness resection device is fitted over the scope and, after placement of a modified over-the-scope-clip, allows a single step EFTR (Figure 4).
Meier et al[74] collected data on 40 EFTRs in rNENs and observed that resection was macroscopically and histologically complete in all cases without major events, but prospective comparative studies between different resection techniques are still missing.
To conclude, rNENs < 10 mm should be treated endoscopically, and EMR-L should be considered as the first-line treatment; ESD can be used as second-line therapy when EMR-L is not applicable. EFTR can be an effective and safe technique in lesions that are difficult to treat. Treatment of rNENs with a size of 10-19 mm should be chosen after assessing the stage and the grade of differentiation.
In recent years there has been a great development of EUS techniques, not only used as diagnostic, but also as therapeutic tools. These methods find application in the management of panNENs, given the direct approach to the pancreas through the echoendoscope. The incidentally discovered small panNENs, mainly nonfunctional, represent a therapeutic challenge because surgery could be very complex in the face of neoplasms with indolent biological behavior, and active surveillance may represent an option for G1 or low G2 neoplasms, asymptomatic, mainly localized in the head of the pancreas, without radiological signs suspicious for malignancy[8,75]. In this setting, however, EUS-guided pancreatic locoregional ablative treatments, using either ethanol injection or radiofrequency ablation, have been proposed in recent studies with promising results in order to control symptoms or reduce tumor burden in selected patients[76]. The thermoablative techniques are the most used, mainly the radiofrequency methods. EUS-guided radiofrequency ablation (RFA) is reported to be a potentially effective and safe treatment for Pan-NENs[77].
Several RFA devices for EUS-guided applications are currently available. The Habib EUS-guided RFA probe (EndoHPB, EMcision UK, London, UK) is a 1 Fr (0.33 mm), monopolar catheter, which can be inserted through a regular 19- or 22-gauge FNA needle and connected to a standard radiofrequency generator. The other systems are needle-electrodes, and the most commonly used in literature is the one from Taewoong Medical (EUSRA, Taewoong Medical Co. Ltd., Gimpo-si, Geyonggi-do, South Korea), an 18- or 19-gauge needle with a long electrode lacking insulation over the terminal tip, connected to a dedicated RF current source, and an inner cooling system that circulates chilled saline inside the needle to avoid tissue charring. Under the EUS guide, the needle is inserted into the target lesion that is being treated by using high-frequency alternating current, and the energy release is applied when the needle tip of the electrode is within the lesion, while maintaining a distance of at least 2 mm from the pancreatic and bile ducts and vessels, to avoid injury or duct strictures. A recent systematic literature review explored the feasibility, effectiveness, and safety of EUS–RFA in the treatment of panNENs[94]: 12 articles describing 61 patients and 73 panNENs were analyzed and the overall effectiveness of EUS–RFA resulted in 96% (75%–100%) without any difference between functional and nonfunctional panNENs and without relevant side effects (mild adverse events, AEs 13.7%)[78-81].
The same conclusions were also confirmed by a further systematic review which included 14 studies with a total of 158 patients with solid pancreatic tumors[82]. However, even if the results of these studies are encouraging, especially for nonfunctioning panNENs and insulinomas < 2 cm, EUS–RFA is a recent technique and long-term data are thus lacking[82]. Larger studies with longer follow-up are needed to evaluate the long-term effectiveness of EUS–RFA. The specific setting of patients and the actual indication for the radiofrequency has not been standardized.
As concerned EUS-guided ethanol injection for small panNENs, this option has been proposed and studied for the treatment of patients with small panNENs not suitable for surgery or who refused surgical approach. Using pure ethanol or ethanol–lipiodol emulsion, the complete ablation rate has been reported to be ~50% up to 80% by performing more sessions[83].
In view of these results, a study protocol for a multicenter prospective study has been published[84] and the results will become available in due time.
Finally, possible future intriguing perspectives can be represented by the application, also in panNENs, of the novel techniques of locoregional delivery of drugs, such as LOcal Drug EluteR [LODER(TM)] which is a novel biodegradable polymeric matrix that shields drugs. panNENs may be considered as a possible future field of application of locoregional radiotherapy by using fiducial markers implantation, similarly to other pancreatic cancers.
The incidence of GEP-NENs has hugely increased over the last decades mainly due to better disease knowledge and to an improvement in diagnostic techniques, including endoscopy. Standard axial endoscopy and EUS still play a pivotal role in several GEP-NENs. Upper GI endoscopy is essential for the detection and characterization of esophageal, gastric and duodenal NENs. EUS represents the diagnostic gold standard for panNENs and the technique of choice for the locoregional staging of gastric, duodenal and rectal NENs. Ileocolonoscopy allows the assessing and diagnosing of rectal, colonic and rarely distal ileal lesions. However, the diagnosis of sbNENs has been largely improved with the advent of CE and DBE, although data regarding the safety and efficacy of these techniques in the neuroendocrine setting are still scanty and their use is still limited in clinical practice. In terms of treatment, in selected localized GI-NENs with the absence of features associated with lymph node metastases, endoscopic therapy is generally an appropriate treatment with radical intent. In highly selected G1 or low G2 small neoplasms without radiological signs suspicious for malignancy EUS-guided pancreatic locoregional ablative treatments, using either ethanol injection or radiofrequency ablation, have been proposed in recent studies with promising results in order to control symptoms or reduce tumor burden. Table 1 summarizes available endoscopic treatment options for GEP-NENs.
| Primary site | Tumor characteristics | Endoscopic management |
| Stomach | Type I < 5 mm | Surveillance |
| Type I ≥ 5 mm | Resection (EMR, ESD) | |
| Type II | ||
| Type III | Resection (EMR, ESD)1 | |
| G1-G2 | ||
| < 10 mm | ||
| Duodenum | < 10 mm2 | Resection (EMR, ESD) |
| G1 | ||
| No muscularis mucosae invasion | ||
| No periampullary | ||
| Pancreas | ≤ 20 mm | Surveillance; EUS-guided RFA; EUS-guided ethanol injection |
| G1-low G2 | ||
| Non-functioning | ||
| No bile/pancreatic duct compression | ||
| Functioning tumors, not suitable for surgery | EUS-guided ethanol injection | |
| The patient refuses the surgical approach | ||
| Rectum | < 10 mm3 | Resection (EMR, mEMR, ESD, EFTR) |
| G1-G2 | ||
| No muscularis mucosae invasion |
In summary, endoscopy plays a key role for diagnosis and treatment of GEP-NENs. In selected localized GEP-NENs, endoscopic therapy is appropriate with radical intent. Advanced resection techniques aimed at increasing the rate of R0 resection should be reserved to high-volume referral centers. The multidisciplinary management remains the gold standard to offer the patient the best therapeutic approach.
The prognosis of gastro-entero-pancreatic neuroendocrine neoplasms (GEP-NENs) is widely variable depending on several factors including the site of the primary tumor, the grading, and the stage. The correct localization of the primary tumor site, as well as a complete histologic diagnosis, represent the milestones for the proper management and the prognosis of these tumors. Standard axial endoscopy and endoscopic ultrasonography (EUS) still play a pivotal role in several GEP-NENs.
The incidence of GEP-NENs has hugely increased over the last decades; given the well-known heterogeneity of these tumors and the lack of large prospective studies, there is an urgent need to standardize their management.
To analyze current evidence on the role of endoscopy in the management of GEP-NENs (both diagnosis and potential treatment). A specific focus will be reserved to capsule endoscopy, double-balloon enteroscopy and ultrasound endoscopy.
An extensive bibliographical search was performed in PubMed to identify guidelines and primary literature (retrospective and prospective studies, systematic reviews, case series) published in the last 15 years, using both medical subject heading (MeSH) terms and free-language keywords: gastro-entero-pancreatic neuroendocrine neoplasms; endoscopy; ultrasound endoscopy; capsule endoscopy; double-balloon enteroscopy; diagnosis; therapy; staging.
EUS represents the diagnostic gold standard for pancreatic NENs (panNENs) and the technique of choice for the locoregional staging of gastric, duodenal and rectal NENs. EUS proved to be the most accurate diagnostic technique in panNEN detection. EUS–fine needle aspiration is a diagnostic advanced EUS technique, which represents the gold standard least invasive option to obtain the histological identification of a suspected pancreatic neoplasm or peripancreatic lymph node. The diagnosis of small bowel NENs (sbNENs) has been improved with the advent of capsule endoscopy (CE) and double-balloon enteroscopy (DBE), even if data regarding the efficacy and safety of these techniques in the detection of sbNENs are scanty and mainly based on small retrospective series, given the rarity of the disease and the still-limited use of these techniques in routine clinical practice. In selected localized gastrointestinal NENs with the absence of features associated with lymph node metastases, endoscopic therapy is generally an appropriate treatment with radical intent. In highly selected G1 or low G2 small neoplasms without radiological signs suspicious for malignancy EUS-guided pancreatic locoregional ablative treatments, using either ethanol injection or radiofrequency ablation, have been proposed in recent studies with promising results in order to control symptoms or reduce tumor burden.
Endoscopy plays a key role in GEP-NENs for both the diagnosis and the treatment. In selected localized GEP-NENs, endoscopic therapy is appropriate with radical intent. The multidisciplinary management and the referral to high-volume tertiary centers remain fundamental.
Further studies are needed: (1) To better define the actual role of CE and DBE in the diagnosis of sbNENs; and (2) To better analyze the possible role of endoscopic confocal laser endomicroscopy in the diagnosis of panNENs and radiofrequency ablation as a potential treatment. Possible future intriguing perspectives can be represented by the application, also in panNENs, of the novel techniques of locoregional delivery of drugs.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Batyrbekov K, Kazakhstan; Poddymova AV, Russia S-Editor: Wu YXJ L-Editor: Kerr C P-Editor: Wu YXJ
| 1. | Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y, Shih T, Yao JC. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. JAMA Oncol. 2017;3:1335-1342. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1510] [Cited by in F6Publishing: 1988] [Article Influence: 284.0] [Reference Citation Analysis (2)] |
| 2. | Rindi G, Bordi C, La Rosa S, Solcia E, Delle Fave G; Gruppo Italiano Patologi Apparato Digerente (GIPAD); Società Italiana di Anatomia Patologica e Citopatologia Diagnostica/International Academy of Pathology, Italian division (SIAPEC/IAP). Gastroenteropancreatic (neuro)endocrine neoplasms: the histology report. Dig Liver Dis. 2011;43 Suppl 4:S356-S360. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Rindi G, Falconi M, Klersy C, Albarello L, Boninsegna L, Buchler MW, Capella C, Caplin M, Couvelard A, Doglioni C, Delle Fave G, Fischer L, Fusai G, de Herder WW, Jann H, Komminoth P, de Krijger RR, La Rosa S, Luong TV, Pape U, Perren A, Ruszniewski P, Scarpa A, Schmitt A, Solcia E, Wiedenmann B. TNM staging of neoplasms of the endocrine pancreas: results from a large international cohort study. J Natl Cancer Inst. 2012;104:764-777. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 348] [Cited by in F6Publishing: 316] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 4. | Boninsegna L, Panzuto F, Partelli S, Capelli P, Delle Fave G, Bettini R, Pederzoli P, Scarpa A, Falconi M. Malignant pancreatic neuroendocrine tumour: lymph node ratio and Ki67 are predictors of recurrence after curative resections. Eur J Cancer. 2012;48:1608-1615. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 123] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 5. | Panzuto F, Boninsegna L, Fazio N, Campana D, Pia Brizzi M, Capurso G, Scarpa A, De Braud F, Dogliotti L, Tomassetti P, Delle Fave G, Falconi M. Metastatic and locally advanced pancreatic endocrine carcinomas: analysis of factors associated with disease progression. J Clin Oncol. 2011;29:2372-2377. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 214] [Cited by in F6Publishing: 211] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 6. | Rossi RE, Conte D, Elli L, Branchi F, Massironi S. Endoscopic techniques to detect small-bowel neuroendocrine tumors: A literature review. United European Gastroenterol J. 2017;5:5-12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Zilli A, Arcidiacono PG, Conte D, Massironi S. Clinical impact of endoscopic ultrasonography on the management of neuroendocrine tumors: lights and shadows. Dig Liver Dis. 2018;50:6-14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Falconi M, Eriksson B, Kaltsas G, Bartsch DK, Capdevila J, Caplin M, Kos-Kudla B, Kwekkeboom D, Rindi G, Klöppel G, Reed N, Kianmanesh R, Jensen RT; Vienna Consensus Conference participants. ENETS Consensus Guidelines Update for the Management of Patients with Functional Pancreatic Neuroendocrine Tumors and Non-Functional Pancreatic Neuroendocrine Tumors. Neuroendocrinology. 2016;103:153-171. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 851] [Cited by in F6Publishing: 863] [Article Influence: 107.9] [Reference Citation Analysis (1)] |
| 9. | Manta R, Nardi E, Pagano N, Ricci C, Sica M, Castellani D, Bertani H, Piccoli M, Mullineris B, Tringali A, Marini F, Germani U, Villanacci V, Casadei R, Mutignani M, Conigliaro R, Bassotti G, Zullo A. Pre-operative Diagnosis of Pancreatic Neuroendocrine Tumors with Endoscopic Ultrasonography and Computed Tomography in a Large Series. J Gastrointestin Liver Dis. 2016;25:317-321. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Fujimori N, Osoegawa T, Lee L, Tachibana Y, Aso A, Kubo H, Kawabe K, Igarashi H, Nakamura K, Oda Y, Ito T. Efficacy of endoscopic ultrasonography and endoscopic ultrasonography-guided fine-needle aspiration for the diagnosis and grading of pancreatic neuroendocrine tumors. Scand J Gastroenterol. 2016;51:245-252. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 11. | Atiq M, Bhutani MS, Bektas M, Lee JE, Gong Y, Tamm EP, Shah CP, Ross WA, Yao J, Raju GS, Wang X, Lee JH. EUS-FNA for pancreatic neuroendocrine tumors: a tertiary cancer center experience. Dig Dis Sci. 2012;57:791-800. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 12. | Dietrich CF, Ignee A, Braden B, Barreiros AP, Ott M, Hocke M. Improved differentiation of pancreatic tumors using contrast-enhanced endoscopic ultrasound. Clin Gastroenterol Hepatol. 2008;6:590-597.e1. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 118] [Cited by in F6Publishing: 114] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 13. | Malagò R, D'Onofrio M, Zamboni GA, Faccioli N, Falconi M, Boninsegna L, Mucelli RP. Contrast-enhanced sonography of nonfunctioning pancreatic neuroendocrine tumors. AJR Am J Roentgenol. 2009;192:424-430. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 63] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Ishikawa R, Kamata K, Hara A, Tanaka H, Okamoto A, Yamazaki T, Nakai A, Omoto S, 4inaga K, Yamao K, Takenaka M, Minami Y, Watanabe T, Chiba Y, Chikugo T, Matsumoto I, Takeyama Y, Matsukubo Y, Hyodo T, Kudo M. Utility of contrast-enhanced harmonic endoscopic ultrasonography for predicting the prognosis of pancreatic neuroendocrine neoplasms. Dig Endosc. 2021;33:829-839. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Leiman G. My approach to pancreatic fine needle aspiration. J Clin Pathol. 2007;60:43-49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Matsubayashi H, Matsui T, Yabuuchi Y, Imai K, Tanaka M, Kakushima N, Sasaki K, Ono H. Endoscopic ultrasonography guided-fine needle aspiration for the diagnosis of solid pancreaticobiliary lesions: Clinical aspects to improve the diagnosis. World J Gastroenterol. 2016;22:628-640. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 69] [Cited by in F6Publishing: 69] [Article Influence: 8.6] [Reference Citation Analysis (1)] |
| 17. | Chen S, Lin J, Wang X, Wu HH, Cramer H. EUS-guided FNA cytology of pancreatic neuroendocrine tumour (PanNET): a retrospective study of 132 cases over an 18-year period in a single institution. Cytopathology. 2014;25:396-403. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Gornals J, Varas M, Catalá I, Maisterra S, Pons C, Bargalló D, Serrano T, Fabregat J. Definitive diagnosis of neuroendocrine tumors using fine-needle aspiration-puncture guided by endoscopic ultrasonography. Rev Esp Enferm Dig. 2011;103:123-128. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Mitra V, Nayar MK, Leeds JS, Wadehra V, Haugk B, Scott J, Charnley RM, Oppong KW. Diagnostic performance of endoscopic ultrasound (EUS)/endoscopic ultrasound--fine needle aspiration (EUS-FNA) cytology in solid and cystic pancreatic neuroendocrine tumours. J Gastrointestin Liver Dis. 2015;24:69-75. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 20. | Weynand B, Borbath I, Bernard V, Sempoux C, Gigot JF, Hubert C, Lannoy V, Deprez PH, Jouret-Mourin A. Pancreatic neuroendocrine tumour grading on endoscopic ultrasound-guided fine needle aspiration: high reproducibility and inter-observer agreement of the Ki-67 labelling index. Cytopathology. 2014;25:389-395. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Delconte G, Cavalcoli F, Magarotto A, Centonze G, Bezzio C, Cattaneo L, Rausa E, Kelly ME, Bonitta G, Milione M, Enzo M. Does ProCore Fine-Needle Biopsy Really Improve the Clinical Outcome of Endoscopic Ultrasound-Guided Sampling of Pancreatic Masses? Dig Dis. 2022;40:78-84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Dietrich CF, Săftoiu A, Jenssen C. Real time elastography endoscopic ultrasound (RTE-EUS), a comprehensive review. Eur J Radiol. 2014;83:405-414. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 23. | Havre RF, Ødegaard S, Gilja OH, Nesje LB. Characterization of solid focal pancreatic lesions using endoscopic ultrasonography with real-time elastography. Scand J Gastroenterol. 2014;49:742-751. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Iglesias-Garcia J, Larino-Noia J, Abdulkader I, Forteza J, Dominguez-Munoz JE. Quantitative endoscopic ultrasound elastography: an accurate method for the differentiation of solid pancreatic masses. Gastroenterology. 2010;139:1172-1180. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 202] [Cited by in F6Publishing: 183] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 25. | Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, Sporea I, Calliada F, Cantisani V, D'Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Fromageau J, Havre RF, Jenssen C, Ohlinger R, Săftoiu A, Schaefer F, Dietrich CF; EFSUMB. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: Clinical applications. Ultraschall Med. 2013;34:238-253. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 621] [Cited by in F6Publishing: 461] [Article Influence: 41.9] [Reference Citation Analysis (0)] |
| 26. | Napoleon B, Lemaistre AI, Pujol B, Caillol F, Lucidarme D, Bourdariat R, Morellon-Mialhe B, Fumex F, Lefort C, Lepilliez V, Palazzo L, Monges G, Poizat F, Giovannini M. In vivo characterization of pancreatic cystic lesions by needle-based confocal laser endomicroscopy (nCLE): proposition of a comprehensive nCLE classification confirmed by an external retrospective evaluation. Surg Endosc. 2016;30:2603-2612. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 76] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 27. | French comment on article: Endoscopic ultrasound-guided needle-based confocal laser endomicroscopy in solid pancreatic masses. Endoscopy. 2016;48:961. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 28. | Varas MJ, Gornals JB, Pons C, Espinós JC, Abad R, Lorente FJ, Bargalló D. Usefulness of endoscopic ultrasonography (EUS) for selecting carcinoid tumors as candidates to endoscopic resection. Rev Esp Enferm Dig. 2010;102:577-582. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Delle Fave G, O'Toole D, Sundin A, Taal B, Ferolla P, Ramage JK, Ferone D, Ito T, Weber W, Zheng-Pei Z, De Herder WW, Pascher A, Ruszniewski P; Vienna Consensus Conference participants. ENETS Consensus Guidelines Update for Gastroduodenal Neuroendocrine Neoplasms. Neuroendocrinology. 2016;103:119-124. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 294] [Cited by in F6Publishing: 302] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 30. | Ramage JK, De Herder WW, Delle Fave G, Ferolla P, Ferone D, Ito T, Ruszniewski P, Sundin A, Weber W, Zheng-Pei Z, Taal B, Pascher A; Vienna Consensus Conference participants. ENETS Consensus Guidelines Update for Colorectal Neuroendocrine Neoplasms. Neuroendocrinology. 2016;103:139-143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 185] [Cited by in F6Publishing: 190] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 31. | Cangemi DJ, Patel MK, Gomez V, Cangemi JR, Stark ME, Lukens FJ. Small bowel tumors discovered during double-balloon enteroscopy: analysis of a large prospectively collected single-center database. J Clin Gastroenterol. 2013;47:769-772. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 32. | Bader TR, Semelka RC, Chiu VC, Armao DM, Woosley JT. MRI of carcinoid tumors: spectrum of appearances in the gastrointestinal tract and liver. J Magn Reson Imaging. 2001;14:261-269. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 113] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 33. | Frilling A, Sotiropoulos GC, Radtke A, Malago M, Bockisch A, Kuehl H, Li J, Broelsch CE. The impact of 68Ga-DOTATOC positron emission tomography/computed tomography on the multimodal management of patients with neuroendocrine tumors. Ann Surg. 2010;252:850-856. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 147] [Cited by in F6Publishing: 152] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 34. | van Tuyl SA, van Noorden JT, Timmer R, Stolk MF, Kuipers EJ, Taal BG. Detection of small-bowel neuroendocrine tumors by video capsule endoscopy. Gastrointest Endosc. 2006;64:66-72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 35. | Prasad V, Ambrosini V, Hommann M, Hoersch D, Fanti S, Baum RP. Detection of unknown primary neuroendocrine tumours (CUP-NET) using (68)Ga-DOTA-NOC receptor PET/CT. Eur J Nucl Med Mol Imaging. 2010;37:67-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 188] [Cited by in F6Publishing: 148] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 36. | Sharma P, Arora S, Mukherjee A, Pal S, Sahni P, Garg P, Khadgawat R, Thulkar S, Bal C, Kumar R. Predictive value of 68Ga-DOTANOC PET/CT in patients with suspicion of neuroendocrine tumors: is its routine use justified? Clin Nucl Med. 2014;39:37-43. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 37. | Cobrin GM, Pittman RH, Lewis BS. Increased diagnostic yield of small bowel tumors with capsule endoscopy. Cancer. 2006;107:22-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 118] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 38. | McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171-179. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4015] [Cited by in F6Publishing: 3550] [Article Influence: 136.5] [Reference Citation Analysis (0)] |
| 39. | Sidhu R, McAlindon ME. The use of capsule endoscopy for the investigation of small bowel tumors: experience from a United Kingdom single center. Dig Dis Sci. 2011;56:2763. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 40. | Frilling A, Smith G, Clift AK, Martin J. Capsule endoscopy to detect primary tumour site in metastatic neuroendocrine tumours. Dig Liver Dis. 2014;46:1038-1042. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 41. | Furnari M, Buda A, Delconte G, Citterio D, Voiosu T, Ballardini G, Cavallaro F, Savarino E, Mazzaferro V, Meroni E. The role of wireless capsule endoscopy (WCE) in the detection of occult primary neuroendocrine tumors. J Gastrointestin Liver Dis. 2017;26:151-156. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 42. | Tominaga K, Kamimura K, Yokoyama J, Terai S. Usefulness of Capsule Endoscopy and Double-balloon Enteroscopy for the Diagnosis of Multiple Carcinoid Tumors in the Small Intestine: Case Reports and a Literature Review. Intern Med. 2019;58:655-659. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 43. | Bellutti M, Fry LC, Schmitt J, Seemann M, Klose S, Malfertheiner P, Mönkemüller K. Detection of neuroendocrine tumors of the small bowel by double balloon enteroscopy. Dig Dis Sci. 2009;54:1050-1058. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 44. | Scherübl H, Faiss S, Tschöpe R, Zeitz M. Double-balloon enteroscopy for the detection of midgut carcinoids. Gastrointest Endosc. 2005;62:994; author reply 994-994; author reply 995. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 45. | Rossi RE, Elli L, Branchi F, Conte D, Massironi S. Double-Balloon Enteroscopy in Detecting Small-Bowel Neuroendocrine Neoplasms: A Single-Center Prospective Study. Digestion. 2021;102:722-730. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 46. | Roberto GA, Rodrigues CMB, Peixoto RD, Younes RN. Gastric neuroendocrine tumor: A practical literature review. World J Gastrointest Oncol. 2020;12:850-856. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 18] [Cited by in F6Publishing: 18] [Article Influence: 4.5] [Reference Citation Analysis (8)] |
| 47. | Scherübl H, Cadiot G. Early Gastroenteropancreatic Neuroendocrine Tumors: Endoscopic Therapy and Surveillance. Visc Med. 2017;33:332-338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 48. | Putzer D, Schullian P, Jaschke W, Bale R. NEN: Advancement in Diagnosis and Minimally Invasive Therapy. Rofo. 2020;192:422-430. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 49. | Panzuto F, Massironi S, Partelli S, Campana D, Rinzivillo M, Invernizzi P, Andreasi V, Lamberti G, Falconi M. Gastro-entero-pancreatic neuroendocrine neoplasia: The rules for non-operative management. Surg Oncol. 2020;35:141-148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 50. | Merola E, Sbrozzi-Vanni A, Panzuto F, D'Ambra G, Di Giulio E, Pilozzi E, Capurso G, Lahner E, Bordi C, Annibale B, Delle Fave G. Type I gastric carcinoids: a prospective study on endoscopic management and recurrence rate. Neuroendocrinology. 2012;95:207-213. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 51. | Manfredi S, Walter T, Baudin E, Coriat R, Ruszniewski P, Lecomte T, Laurenty AP, Goichot B, Rohmer V, Roquin G, Cojocarasu OZ, Lombard-Bohas C, Lepage C, Morcet J, Cadiot G. Management of gastric neuro-endocrine tumours in a large French national cohort (GTE). Endocrine. 2017;57:504-511. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 52. | Kwon YH, Jeon SW, Kim GH, Kim JI, Chung IK, Jee SR, Kim HU, Seo GS, Baik GH, Choi KD, Moon JS. Long-term follow up of endoscopic resection for type 3 gastric NET. World J Gastroenterol. 2013;19:8703-8708. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 58] [Cited by in F6Publishing: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 53. | Scherübl H, Jensen RT, Cadiot G, Stölzel U, Klöppel G. Management of early gastrointestinal neuroendocrine neoplasms. World J Gastrointest Endosc. 2011;3:133-139. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 59] [Cited by in F6Publishing: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 54. | Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A, Amato A, Berr F, Bhandari P, Bialek A, Conio M, Haringsma J, Langner C, Meisner S, Messmann H, Morino M, Neuhaus H, Piessevaux H, Rugge M, Saunders BP, Robaszkiewicz M, Seewald S, Kashin S, Dumonceau JM, Hassan C, Deprez PH. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:829-854. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 817] [Cited by in F6Publishing: 852] [Article Influence: 94.7] [Reference Citation Analysis (0)] |
| 55. | Massironi S, Campana D, Partelli S, Panzuto F, Rossi RE, Faggiano A, Brighi N, Falconi M, Rinzivillo M, Delle Fave G, Colao AM, Conte D. Heterogeneity of Duodenal Neuroendocrine Tumors: An Italian Multi-center Experience. Ann Surg Oncol. 2018;25:3200-3206. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 56. | Kim GH, Kim JI, Jeon SW, Moon JS, Chung IK, Jee SR, Kim HU, Seo GS, Baik GH, Lee YC; Korean College of Helicobacter and Upper Gastrointestinal Research. Endoscopic resection for duodenal carcinoid tumors: a multicenter, retrospective study. J Gastroenterol Hepatol. 2014;29:318-324. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 78] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 57. | Untch BR, Bonner KP, Roggin KK, Reidy-Lagunes D, Klimstra DS, Schattner MA, Fong Y, Allen PJ, D'Angelica MI, DeMatteo RP, Jarnagin WR, Kingham TP, Tang LH. Pathologic grade and tumor size are associated with recurrence-free survival in patients with duodenal neuroendocrine tumors. J Gastrointest Surg. 2014;18:457-62; discussion 462. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 58. | Gamboa AC, Liu Y, Lee RM, Zaidi MY, Staley CA, Kooby DA, Winer JH, Shah MM, Russell MC, Cardona K, Maithel SK. Duodenal neuroendocrine tumors: Somewhere between the pancreas and small bowel? J Surg Oncol. 2019;120:1293-1301. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 59. | Hatta W, Koike T, Iijima K, Asanuma K, Asano N, Musha H, Inomata Y, Sano T, Endo H, Ikehata A, Horii T, Ohyauchi M, Yokosawa S, Kasajima A, Fujishima F, Sasano H, Nakaya N, Nakamura T, Shimosegawa T. The Risk Factors for Metastasis in Non-Ampullary Duodenal Neuroendocrine Tumors Measuring 20 mm or Less in Diameter. Digestion. 2017;95:201-209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 60. | Rossi RE, Milanetto AC, Andreasi V, Campana D, Coppa J, Nappo G, Rinzivillo M, Invernizzi P, Modica R, David A, Partelli S, Lamberti G, Mazzaferro V, Zerbi A, Panzuto F, Pasquali C, Falconi M, Massironi S; ItaNet (Italian Association for Neuroendocrine Tumours) study group. Risk of preoperative understaging of duodenal neuroendocrine neoplasms: a plea for caution in the treatment strategy. J Endocrinol Invest. 2021;44:2227-2234. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 61. | Basuroy R, Haji A, Ramage JK, Quaglia A, Srirajaskanthan R. Review article: the investigation and management of rectal neuroendocrine tumours. Aliment Pharmacol Ther. 2016;44:332-345. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 62. | Son HJ, Sohn DK, Hong CW, Han KS, Kim BC, Park JW, Choi HS, Chang HJ, Oh JH. Factors associated with complete local excision of small rectal carcinoid tumor. Int J Colorectal Dis. 2013;28:57-61. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 63. | Dąbkowski K, Szczepkowski M, Kos-Kudła B, Starzynska T. Endoscopic management of rectal neuroendocrine tumours. How to avoid a mistake and what to do when one is made? Endokrynol Pol. 2020;71:343-349. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 64. | He L, Deng T, Luo H. Efficacy and safety of endoscopic resection therapies for rectal carcinoid tumors: a meta-analysis. Yonsei Med J. 2015;56:72-81. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 65. | Zhou X, Xie H, Xie L, Li J, Cao W, Fu W. Endoscopic resection therapies for rectal neuroendocrine tumors: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2014;29:259-268. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 66. | Park SS, Han KS, Kim B, Chang Kim B, Hong CW, Sohn DK, Chang HJ. Comparison of underwater endoscopic mucosal resection and endoscopic submucosal dissection of rectal neuroendocrine tumors (with videos). Gastrointest Endosc. 2020;91:1164-1171.e2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 67. | Lee WH, Kim SW, Lim CH, Kim JS, Cho YK, Lee IS, Choi MG, Choi KY. Efficacy of endoscopic mucosal resection using a dual-channel endoscope compared with endoscopic submucosal dissection in the treatment of rectal neuroendocrine tumors. Surg Endosc. 2013;27:4313-4318. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 68. | Lee HS, Moon HS, Kwon IS, Park JH, Kim JS, Kang SH, Lee ES, Kim SH, Sung JK, Lee BS, Jeong HY. Comparison of conventional and modified endoscopic mucosal resection methods for the treatment of rectal neuroendocrine tumors. Surg Endosc. 2021;35:6055-6065. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 69. | Park SB, Kim HW, Kang DH, Choi CW, Kim SJ, Nam HS. Advantage of endoscopic mucosal resection with a cap for rectal neuroendocrine tumors. World J Gastroenterol. 2015;21:9387-9393. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 33] [Cited by in F6Publishing: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 70. | Kim HH, Park SJ, Lee SH, Park HU, Song CS, Park MI, Moon W. Efficacy of endoscopic submucosal resection with a ligation device for removing small rectal carcinoid tumor compared with endoscopic mucosal resection: analysis of 100 cases. Dig Endosc. 2012;24:159-163. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 71. | Lee J, Park YE, Choi JH, Heo NY, Park J, Park SH, Moon YS, Nam KH, Kim TO. Comparison between cap-assisted and ligation-assisted endoscopic mucosal resection for rectal neuroendocrine tumors. Ann Gastroenterol. 2020;33:385-390. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 72. | Niimi K, Goto O, Fujishiro M, Kodashima S, Ono S, Mochizuki S, Asada-Hirayama I, Konno-Shimizu M, Mikami-Matsuda R, Minatsuki C, Yamamichi N, Koike K. Endoscopic mucosal resection with a ligation device or endoscopic submucosal dissection for rectal carcinoid tumors: an analysis of 24 consecutive cases. Dig Endosc. 2012;24:443-447. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 73. | Wang XY, Chai NL, Linghu EQ, Li HK, Zhai YQ, Feng XX, Zhang WG, Zou JL, Li LS, Xiang JY. Efficacy and safety of hybrid endoscopic submucosal dissection compared with endoscopic submucosal dissection for rectal neuroendocrine tumors and risk factors associated with incomplete endoscopic resection. Ann Transl Med. 2020;8:368. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 74. | Meier B, Albrecht H, Wiedbrauck T, Schmidt A, Caca K. Full-thickness resection of neuroendocrine tumors in the rectum. Endoscopy. 2020;52:68-72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 75. | Partelli S, Ramage JK, Massironi S, Zerbi A, Kim HB, Niccoli P, Panzuto F, Landoni L, Tomazic A, Ibrahim T, Kaltsas G, Bertani E, Sauvanet A, Segelov E, Caplin M, Coppa J, Armstrong T, Weickert MO, Butturini G, Staettner S, Boesch F, Cives M, Moulton CA, He J, Selberherr A, Twito O, Castaldi A, De Angelis CG, Gaujoux S, Almeamar H, Frilling A, Vigia E, Wilson C, Muffatti F, Srirajaskanthan R, Invernizzi P, Lania A, Kwon W, Ewald J, Rinzivillo M, Nessi C, Smid LM, Gardini A, Tsoli M, Picardi EE, Hentic O, Croagh D, Toumpanakis C, Citterio D, Ramsey E, Mosterman B, Regi P, Gasteiger S, Rossi RE, Smiroldo V, Jang JY, Falconi M. Management of Asymptomatic Sporadic Nonfunctioning Pancreatic Neuroendocrine Neoplasms (ASPEN) ≤2 cm: Study Protocol for a Prospective Observational Study. Front Med (Lausanne). 2020;7:598438. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 76. | Melita G, Pallio S, Tortora A, Crinò SF, Macrì A, Dionigi G. Diagnostic and Interventional Role of Endoscopic Ultrasonography for the Management of Pancreatic Neuroendocrine Neoplasms. J Clin Med. 2021;10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 77. | Imperatore N, de Nucci G, Mandelli ED, de Leone A, Zito FP, Lombardi G, Manes G. Endoscopic ultrasound-guided radiofrequency ablation of pancreatic neuroendocrine tumors: a systematic review of the literature. Endosc Int Open. 2020;8:E1759-E1764. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 78. | Rossi S, Viera FT, Ghittoni G, Cobianchi L, Rosa LL, Siciliani L, Bortolotto C, Veronese L, Vercelli A, Gallotti A, Ravetta V. Radiofrequency ablation of pancreatic neuroendocrine tumors: a pilot study of feasibility, efficacy, and safety. Pancreas. 2014;43:938-945. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 79. | Pai M, Habib N, Senturk H, Lakhtakia S, Reddy N, Cicinnati VR, Kaba I, Beckebaum S, Drymousis P, Kahaleh M, Brugge W. Endoscopic ultrasound guided radiofrequency ablation, for pancreatic cystic neoplasms and neuroendocrine tumors. World J Gastrointest Surg. 2015;7:52-59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 167] [Cited by in F6Publishing: 131] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 80. | Oleinikov K, Dancour A, Epshtein J, Benson A, Mazeh H, Tal I, Matalon S, Benbassat CA, Livovsky DM, Goldin E, Gross DJ, Jacob H, Grozinsky-Glasberg S. Endoscopic Ultrasound-Guided Radiofrequency Ablation: A New Therapeutic Approach for Pancreatic Neuroendocrine Tumors. J Clin Endocrinol Metab. 2019;104:2637-2647. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 63] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 81. | de Nucci G, Imperatore N, Mandelli ED, di Nuovo F, d'Urbano C, Manes G. Endoscopic ultrasound-guided radiofrequency ablation of pancreatic neuroendocrine tumors: a case series. Endosc Int Open. 2020;8:E1754-E1758. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 82. | Zhang L, Tan S, Huang S, Zhong C, Lü M, Peng Y, Tang X. The safety and efficacy of endoscopic ultrasound-guided ablation therapy for solid pancreatic tumors: a systematic review. Scand J Gastroenterol. 2020;55:1121-1131. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 83. | Park DH, Choi JH, Oh D, Lee SS, Seo DW, Lee SK, Kim MH. Endoscopic ultrasonography-guided ethanol ablation for small pancreatic neuroendocrine tumors: results of a pilot study. Clin Endosc. 2015;48:158-164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 84. | Matsumoto K, Kato H, Kitano M, Hara K, Kuwatani M, Ashida R, Takenaka M, Yamazaki T, Sakurai J, Yoshida M, Okada H. Study protocol for endoscopic ultrasonography-guided ethanol injection therapy for patients with pancreatic neuroendocrine neoplasm: a multicentre prospective study. BMJ Open. 2021;11:e046505. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |