Copyright
©The Author(s) 2020.
World J Gastroenterol. Oct 28, 2020; 26(40): 6111-6140
Published online Oct 28, 2020. doi: 10.3748/wjg.v26.i40.6111
Published online Oct 28, 2020. doi: 10.3748/wjg.v26.i40.6111
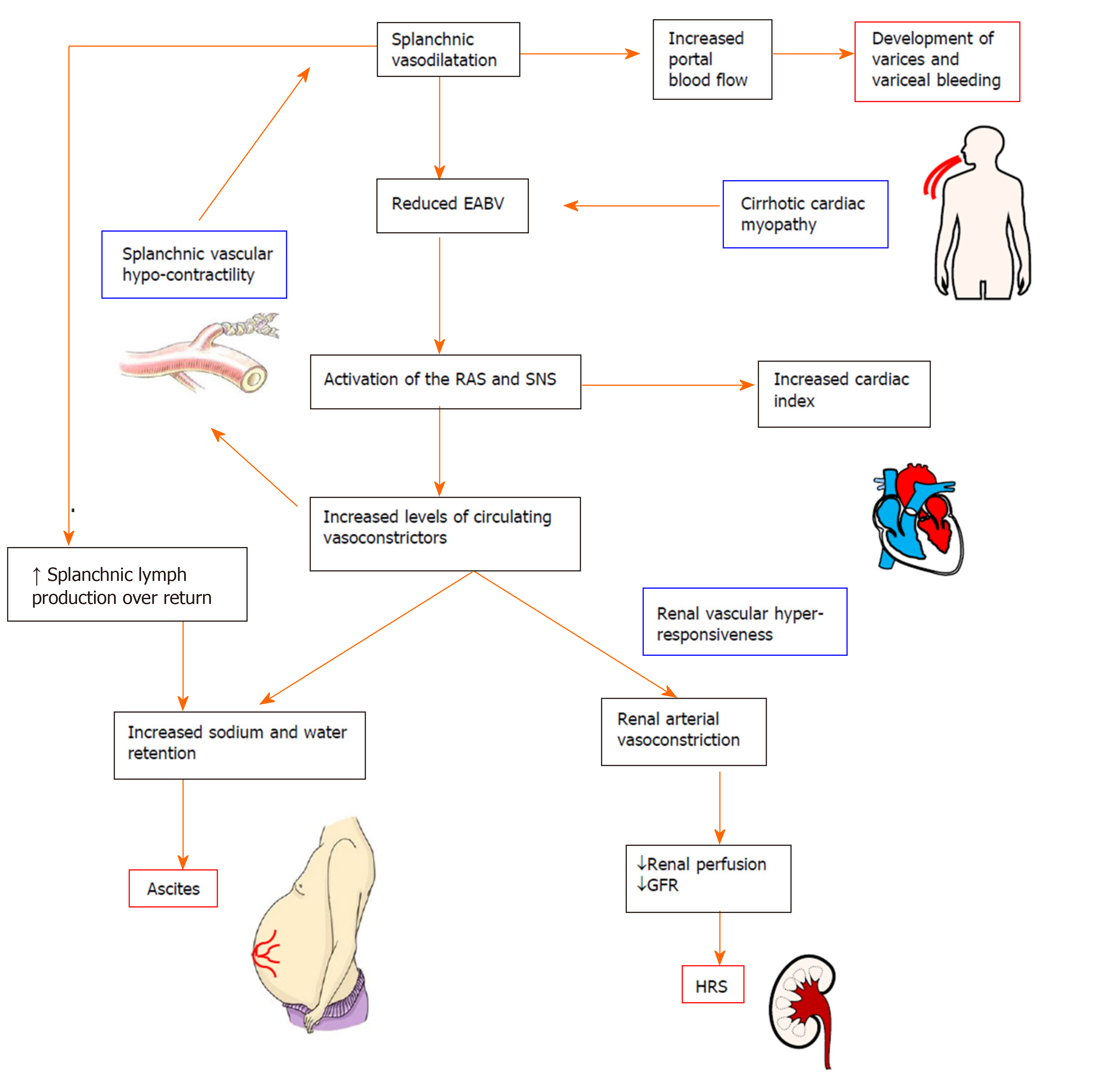
Figure 2 Pathophysiology of the complications in decompensated cirrhosis.
Splanchnic vasodilatation and subsequent reduction of effective arterial blood volume (EABV) triggers the activation of homeostatic mechanisms such as the renin angiotensin system and sympathetic nervous system to promote sodium and water retention and vasoconstriction. Increased hydrostatic pressure and increased capillary permeability in splanchnic vessels cause leaking of excess fluid into peritoneal cavity and the onset of ascites. The renal vasculature is hyper-responsive to the activated circulating vasoconstrictor systems, creating a deficit in renal perfusion and glomerular filtration rate which in turn leads to the development of hepatorenal syndrome. In decompensated cirrhosis, the compensatory mechanisms to restore EABV are ineffective due to the intrinsic splanchnic vascular hypocontractility and cardiomyopathy. EABV: Effective arterial blood volume; RAS: Renin angiotensin system; SNS: Sympathetic nervous system; GFR: Glomerular filtration rate; HRS: Hepatorenal syndrome.
- Citation: Gunarathne LS, Rajapaksha H, Shackel N, Angus PW, Herath CB. Cirrhotic portal hypertension: From pathophysiology to novel therapeutics. World J Gastroenterol 2020; 26(40): 6111-6140
- URL: https://www.wjgnet.com/1007-9327/full/v26/i40/6111.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i40.6111