Copyright
©The Author(s) 2020.
World J Gastroenterol. Jul 14, 2020; 26(26): 3800-3813
Published online Jul 14, 2020. doi: 10.3748/wjg.v26.i26.3800
Published online Jul 14, 2020. doi: 10.3748/wjg.v26.i26.3800
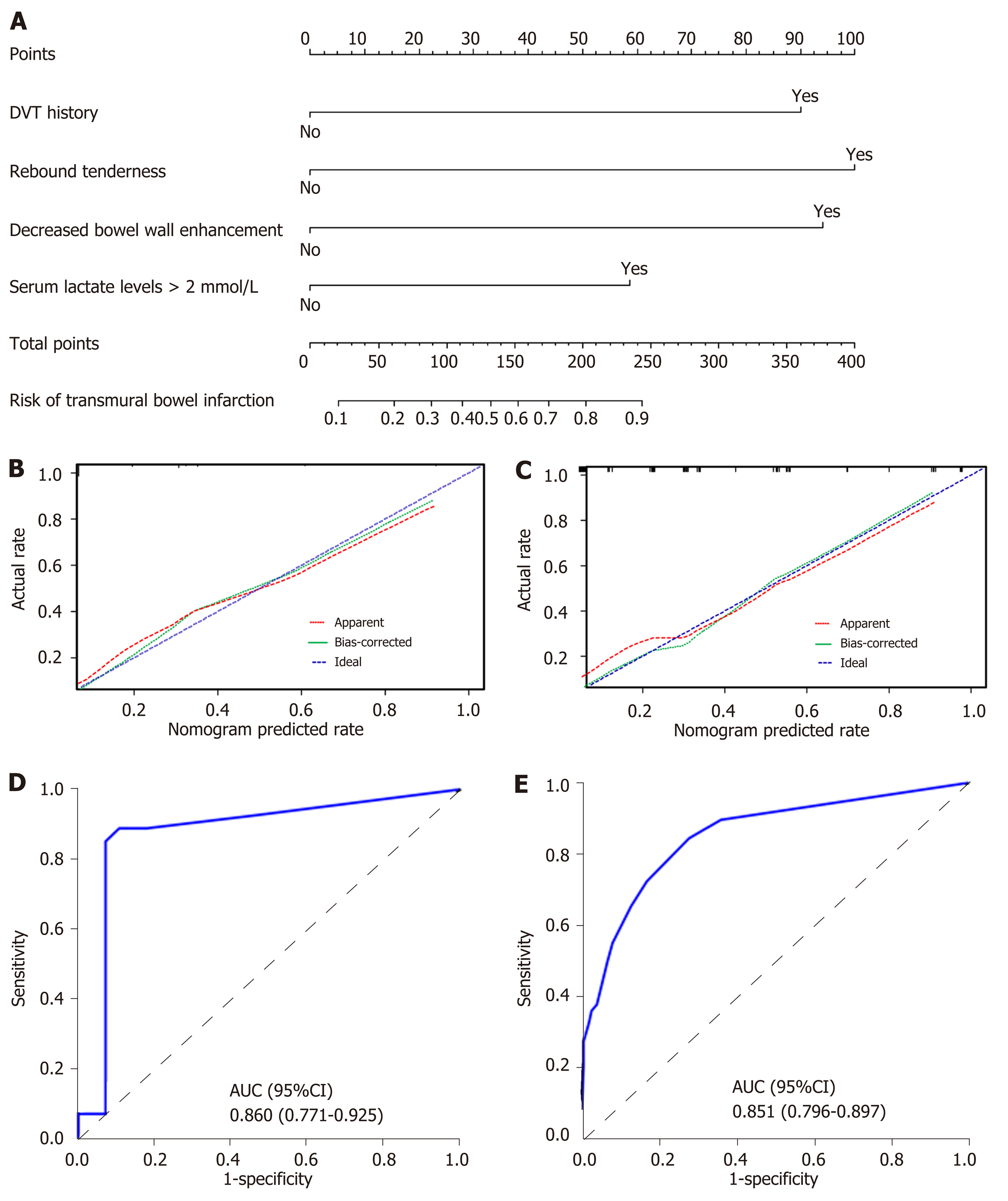
Figure 2 Nomogram for evaluation of transmural bowel infarction risk and its predictive performance.
A: Nomogram for estimating the risk of transmural bowel infarction (TBI) in patients with acute mesenteric ischemia (AMI). The nomogram is used to find the position of each variable on the corresponding axis, draw a line to the points axis for the number of points, add the points from all of the variables, and draw a line from the total points axis to determine the risk of TBI at the lower line of the nomogram. For example, a 30-year-old male patient (have transmural bowel infarction finally) with a previous history of deep venous thrombosis and serum lactate levels > 2 mmol/L, no rebound tenderness and no decreased bowel wall enhancement, has a risk of 59% of TBI calculated by the nomogram; B and C: Calibration curves of the nomogram in the training and validation sets, respectively. Calibration curves depict the calibration of the model in terms of the agreement between the predicted probabilities of TBI and observed outcomes of TBI. The dotted blue line represents an ideal prediction, and the dotted red line represents the predictive ability of the nomogram. The closer the dotted red line fit is to the dotted blue line, the better the predictive accuracy of the nomogram is; D and E: The ROC curves of the nomogram in the training and validation sets, respectively. TBI: Transmural bowel infarction; AMI: Acute mesenteric ischemia; DVT: Deep venous thrombosis; AUC: Area under the receiver operator characteristic curve; ROC: Receiver operator characteristic curve.
- Citation: Jiang M, Li CL, Pan CQ, Lv WZ, Ren YF, Cui XW, Dietrich CF. Nomogram for predicting transmural bowel infarction in patients with acute superior mesenteric venous thrombosis. World J Gastroenterol 2020; 26(26): 3800-3813
- URL: https://www.wjgnet.com/1007-9327/full/v26/i26/3800.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i26.3800