Published online Apr 7, 2020. doi: 10.3748/wjg.v26.i13.1540
Peer-review started: December 4, 2019
First decision: January 13, 2020
Revised: March 4, 2020
Accepted: March 10, 2020
Article in press: March 10, 2020
Published online: April 7, 2020
Hemolymphangiomas are rare malformations composed of both lymphatic and vascular vessels and are located in the pancreas, spleen, mediastinum, etc. Small intestinal hemolymphangioma is extremely rare and often presents as obscure gastrointestinal bleeding. It is rarely diagnosed correctly before the operation. Endoscopic injection sclerotherapy is usually used as a management of bleeding in esophageal varices and was occasionally reported as a treatment of vascular malformation. The treatment of small intestinal hemolymphangioma with enteroscopic injection sclerotherapy has not been reported.
A 42-year-old male complained of recurrent episodes of melena and dizziness, fatigue and reduced exercise capacity for more than 2 mo. Gastroduodenoscopy and blood test revealed a gastric ulcer and anemia. Treatment with oral proton-pump inhibitors and iron did not improve symptoms. We then performed a capsule endoscopy and anterograde balloon-assisted enteroscopy and revealed a hemolymphangioma. Considering it is a benign tumor without malignant potential, we performed enteroscopic injection sclerotherapy. He was discharged 4 days later. At follow-up 3 mo later, the melena disappeared. Balloon-assisted enteroscopy revealed an atrophied tumor atrophied and no bleeding. Argon plasma coagulation was applied to the surface of the hemolymphangioma to accelerated healing. When he returned for follow-up 1 year later, anemia was resolved and the tumor had been cured.
Balloon-assisted enteroscopy and capsule endoscopy are effective methods for diagnosis of hemolymphangioma. Enteroscopic injection sclerotherapy is an effective treatment.
Core tip: Small intestinal hemolymphangioma is a rare malformation presenting as obscure gastrointestinal bleeding and anemia. Though the malformation has a typical lymphangiectatic appearance of white patches on the mucosal surface, it is rarely diagnosed correctly before the operation. We report a case of intestinal hemolymphangioma diagnosed by capsule endoscopy and balloon-assisted enteroscopy. We applied a new, minimally invasive therapy named enteroscopic injection sclerotherapy to manage this disease, which has been proven to be effective and safe. The literature review can present a better understanding of this disease and the advantage of the new management.
- Citation: Xiao NJ, Ning SB, Li T, Li BR, Sun T. Small intestinal hemolymphangioma treated with enteroscopic injection sclerotherapy: A case report and review of literature. World J Gastroenterol 2020; 26(13): 1540-1545
- URL: https://www.wjgnet.com/1007-9327/full/v26/i13/1540.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i13.1540
Small intestinal hemolymphangioma is a rare benign malformation consisting of blood vessels and lymphatic channels with luminal dilation. Individuals with small intestinal hemolymphangioma may present with obscure gastrointestinal bleeding and anemia. Though the malformation has a typical lymphangiectatic appearance of white patches on the mucosal surface, it is rarely diagnosed correctly with conventional endoscopy due to the special anatomic location. Here we present a case of small intestinal hemolymphangioma diagnosed by capsule endoscopy (CE) and balloon-assisted enteroscopy (BAE). We applied a new, minimally invasive therapy named enteroscopic injection sclerotherapy to manage this disease, which has been proven to be effective and safe.
A 42-year-old male complained of recurrent episodes of melena and dizziness, fatigue and reduced exercise capacity for more than 2 mo.
The patient's symptoms started 2 mo ago with recurrent episodes of melena and he frequently felt fatigued. He was diagnosed with a gastric ulcer and anemia after undergoing gastroduodenoscopy, colonoscopy and laboratory blood tests. Then he took oral proton-pump inhibitors and iron for 1.5 mo, but these therapies did not ameliorate the symptoms.
The patient had no previous medical history.
On examination, anemic face and upper abdominal tenderness were noted. The vital signs were normal with a respiratory rate of 18/min, heart rate of 96/min and blood pressure of 102/62 mmHg.
Blood analysis revealed severe iron-deficiency anemia with hemoglobin of 53 g/dL, and fecal occult blood was positive. Blood biochemistry, tumor biomarkers, other blood tests as well as urine analysis were normal. Electrocardiogram and chest X-ray were also normal.
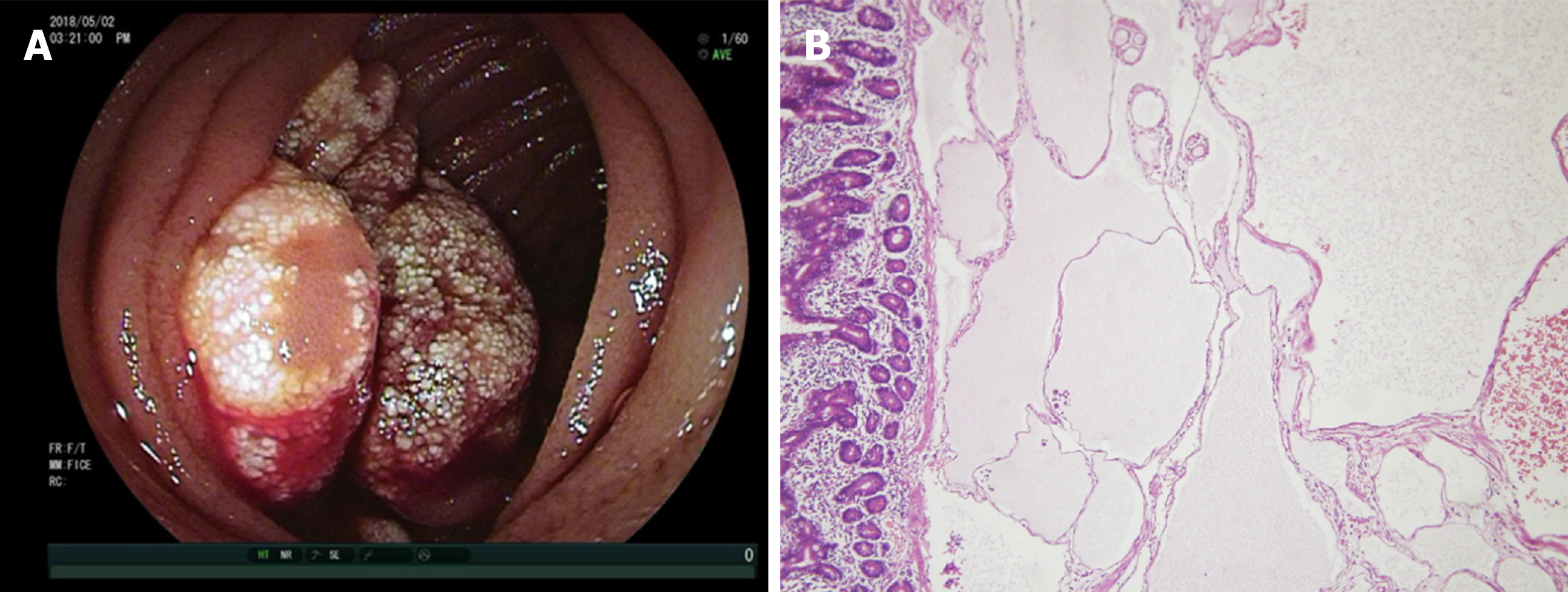
When the patient presented in our hospital, two units of blood were transfused. The gastroduodenoscopy was performed again. A sealed ulcer without any signs of bleeding sign were found in the antrum. We then performed a CE. Bleeding was found in the jejunum after running the capsule for 97 min. The total running time in the small bowel was about 300 min. The CE cannot determine the cause of bleeding due to the short stay around the lesion and the influence of the blood. An anterograde BAE was performed, and a protruded lesion was revealed in the jejunum at about 150 cm distal to the ligament of Treitz. It filled half of the intestinal cavity. The tumor was lobulated with white patches on the mucosal surface with blood oozing in the fundus (Figure 1A). Multiple biopsies were taken, and pathological findings further revealed that hyperplastic thin-walled lymphatic and venous with luminal dilation presented in the submucosal area (Figure 1B).
The final diagnosis of the presented case was iron-deficiency anemia with intestinal bleeding due to hemolymphangioma.
Considering it is a benign tumor without malignant potential, we performed enteroscopic injection sclerotherapy with polidocanol to manage the chronic bleeding. The malformation was completely sclerotized, and no bleeding or perforation was experienced. He was discharged 4 d later.
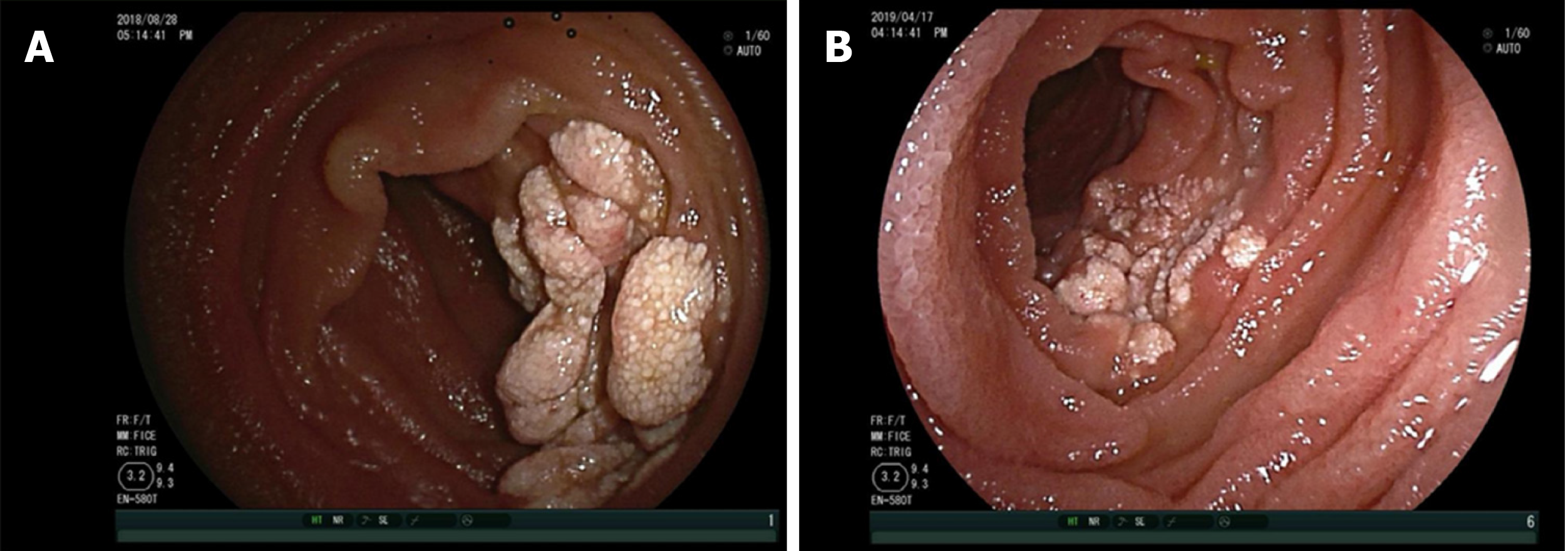
During a follow-up visit, 3 mo after enteroscopic injection sclerotherapy, the patient felt better than before. The patient’s hemoglobin was 126 g/dL, and the melena had disappeared. The tumor had atrophied dramatically, and bleeding was hardly observed (Figure 2A). Argon plasma coagulation was applied to the atrophic hemolymphangioma to accelerated healing. At 1 year later the patient returned to our department for the second follow-up. Laboratory blood tests revealed a normal hemoglobin of 140 g/dL. The tumor was gone, and only a few white patches on the mucosal surface were visible (Figure 2B).
Hemolymphangioma is an uncommon category of lymphangioma, which is a group of malformations of the lymphatic system. Lymphangioma can be located at the mesentery, pancreas, mediastinum, etc, but small intestinal lymphangiomas are extremely rare (less than 1% of all lymphangiomas). Only 19 reports (with 40 patients) of small bowel lymphangioma were reported from 1960 to 2009 in a literature review on lymphangiomas[1]. About half of those patients presented with gastrointestinal bleeding, and the majority of lesions were within the jejunum. The standard treatment of this disease was surgical resection and only two of the forty patients were treated by BAE. One lesion was treated with an injection of 1:10000 epinephrine and was very small (4 mm × 6 mm)[2]. The other lesion treated by BAE was not clearly described[3]. With the advent of CE and BAE, small intestinal lymphangiomas have been found more often, and even small intestinal hemolymphangioma have been reported. We proceeded to a review the literature from 2010 to 2019 by searching “hemolym-phangioma [All Fields] OR hemangiolymphangioma [All Fields]” on PubMed. Six case reports of small intestinal hemolymphangioma were found (Table 1)[4-9]. All of them were located in the proximal jejunum (or duodenum) and presented as anemia due to gastrointestinal bleeding. Six lesions were diagnosed by endoscopy (five enteroscopy and one gastroduodenoscopy), and three were detected by CE examination. These data support that CE and BAE are effective tools for diagnosing hemolymphangioma.
| Ref. | Year | Age/sex | Symptom | Location | Tumor size in cm | Diagnostic method | Management |
| Fang et al[4] | 2012 | 57/F | Melena, anemia | 30 cm distal to Treitz | 5.0 | Enteroscopy | Surgical resection |
| Antonino et al[5] | 2014 | 24/F | Anemia | Second portion of duodenum | 5.0 | Gastroduodenoscopy | Surgical resection |
| Gómez-Galán et al[6] | 2016 | 43/F | Chronic anemia | Distal duodenum | 4.0 | Capsule endoscopy and enteroscopy | Surgical resection |
| Blanco et al[7] | 2017 | 45/F | Melena, anemia | 90 cm distal to Treitz | 8.0 | Capsule endoscopy and enteroscopy | Laparoscopic small bowel resection |
| Iwaya et al[8] | 2018 | 70/M | Melena, anemia | 120 cm distal to Treitz | 2.0 | Capsule endoscopy and enteroscopy | Laparoscopic small bowel resection |
| Yang et al[9] | 2019 | 20/F | Melena, anemia | 60 cm distal to Treitz | 10.0 | Computed tomography scan and enteroscopy | Laparoscopic small bowel resection |
The standard management of hemolymphangioma until recently has been through surgical resection. Surgeons usually aim for complete removal of the tumor because partial ablation of the tumor leads to a 50%-100% recurrence[4]. But invasive surgery pushes endoscopists to pursue new management methods that are minimally invasive. Hemolymphangioma managed by endoscopy is acceptable for the nature of a benign tumor. Endoscopic mucosal resection with a band ligation device had been reported in managing a gastric hemolymphangioma[10]. Also, an endoscopic polypectomy and argon plasma coagulation was successfully performed in a jejunal lymphangioma[11]. Endoscopic injection sclerotherapy is usually used as a treatment for esophageal varices, including the treatment of esophageal hemangioma. Furthermore, polidocanol injection therapy was also applied in small bowel hemangioma without bleeding or perforation[12]. Based on these precedents and our experience in the treatment of blue rubber bleb nevus syndrome[13], we performed enteroscopic injection sclerotherapy to manage the jejunum hemolymphangioma. To our knowledge, this is the first case of small intestinal hemolymphangioma successfully treated by enteroscopic injection sclerotherapy. At the 1 year follow-up, no recurrence of anemia or melena proved that this treatment is feasible.
In summary, small intestinal hemolymphangioma is a rare malformation consisting of blood vessels and lymphatic channels. The lesion is mainly located within the proximal jejunum and clinically presents as melena and anemia. BAE and CE are effective methods for preoperative diagnosis of hemolymphangioma, and enteroscopic injection sclerotherapy is a feasible, minimally invasive treatment to manage this benign tumor.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Chinese Medical Association; Chinese Medical Doctor Association.
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: García-Compeán D, Kwon KA S-Editor: Ma YJ L-Editor: Filipodia E-Editor: Ma YJ
| 1. | Morris-Stiff G, Falk GA, El-Hayek K, Vargo J, Bronner M, Vogt DP. Jejunal cavernous lymphangioma. BMJ Case Rep. 2011;2011. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Li F, Osuoha C, Leighton JA, Harrison ME. Double-balloon enteroscopy in the diagnosis and treatment of hemorrhage from small-bowel lymphangioma: a case report. Gastrointest Endosc. 2009;70:189-190. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Shyung LR, Lin SC, Shih SC, Chang WH, Chu CH, Wang TE. Proposed scoring system to determine small bowel mass lesions using capsule endoscopy. J Formos Med Assoc. 2009;108:533-538. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Fang YF, Qiu LF, Du Y, Jiang ZN, Gao M. Small intestinal hemolymphangioma with bleeding: a case report. World J Gastroenterol. 2012;18:2145-2146. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 41] [Cited by in F6Publishing: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Antonino A, Gragnano E, Sangiuliano N, Rosato A, Maglio M, De Palma M. A very rare case of duodenal hemolymphangioma presenting with iron deficiency anemia. Int J Surg Case Rep. 2014;5:118-121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Gómez-Galán S, Mosquera-Paz MS, Ceballos J, Cifuentes-Grillo PA, Gutiérrez-Soriano L. Duodenal hemangiolymphangioma presenting as chronic anemia: a case report. BMC Res Notes. 2016;9:426. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Blanco Velasco G, Tun Abraham A, Hernández Mondragón O, Blancas Valencia JM. Hemolymphangioma as a cause of overt obscure gastrointestinal bleeding: a case report. Rev Esp Enferm Dig. 2017;109:213-214. [PubMed] [Cited in This Article: ] |
| 8. | Iwaya Y, Streutker CJ, Coneys JG, Marcon N. Hemangiolymphangioma of the small bowel: A rare cause of chronic anemia. Dig Liver Dis. 2018;50:1248. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Yang J, Zhang Y, Kou G, Li Y. Jejunum Hemolymphangioma Causing Refractory Anemia in a Young Woman. Am J Gastroenterol. 2019;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Kim WT, Lee SW, Lee JU. Bleeding gastric hemolymphangioma: endoscopic therapy is feasible. Dig Endosc. 2013;25:553-554. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Kida A, Matsuda K, Hirai S, Shimatani A, Horita Y, Hiramatsu K, Matsuda M, Ogino H, Ishizawa S, Noda Y. A pedunculated polyp-shaped small-bowel lymphangioma causing gastrointestinal bleeding and treated by double-balloon enteroscopy. World J Gastroenterol. 2012;18:4798-4800. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 15] [Cited by in F6Publishing: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Igawa A, Oka S, Tanaka S, Kunihara S, Nakano M, Chayama K. Polidocanol injection therapy for small-bowel hemangioma by using double-balloon endoscopy. Gastrointest Endosc. 2016;84:163-167. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Ning S, Zhang Y, Zu Z, Mao X, Mao G. Enteroscopic sclerotherapy in blue rubber bleb nevus syndrome. Pak J Med Sci. 2015;31:226-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |