Published online May 28, 2018. doi: 10.3748/wjg.v24.i20.2137
Peer-review started: March 29, 2018
First decision: April 27, 2018
Revised: May 5, 2018
Accepted: May 18, 2018
Article in press: May 18, 2018
Published online: May 28, 2018
Processing time: 60 Days and 14 Hours
Pancreatic ductal adenocarcinoma (PDAC) is one of the deadliest cancers, mostly due to its resistance to treatment. Of these, checkpoint inhibitors (CPI) are inefficient when used as monotherapy, except in the case of a rare subset of tumors harboring microsatellite instability (< 2%). This inefficacy mainly resides in the low immunogenicity and non-inflamed phenotype of PDAC. The abundant stroma generates a hypoxic microenvironment and drives the recruitment of immunosuppressive cells through cancer-associated-fibroblast activation and transforming growth factor β secretion. Several strategies have recently been developed to overcome this immunosuppressive microenvironment. Combination therapies involving CPI aim at increasing tumor immunogenicity and promoting the recruitment and activation of effector T cells. Ongoing studies are therefore exploring the association of CPI with vaccines, oncolytic viruses, MEK inhibitors, cytokine inhibitors, and hypoxia- and stroma-targeting agents. Adoptive T-cell transfer is also under investigation. Moreover, translational studies on tumor tissue and blood, prior to and during treatment may lead to the identification of biomarkers with predictive value for both clinical outcome and response to immunotherapy.
Core tip: Checkpoint inhibitors (CPI) and other immune therapies remain inefficient when used as single agents in pancreatic ductal adenocarcinoma (PDAC). Here, we present an overview of the biological mechanisms underlying these failures and the lessons learned, giving a rationale for innovative combination therapies. In particular, the latest ongoing studies are attempting to overcome the immunosuppressive microenvironment, the basis of resistance to CPI in PDAC.
- Citation: Hilmi M, Bartholin L, Neuzillet C. Immune therapies in pancreatic ductal adenocarcinoma: Where are we now? World J Gastroenterol 2018; 24(20): 2137-2151
- URL: https://www.wjgnet.com/1007-9327/full/v24/i20/2137.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i20.2137
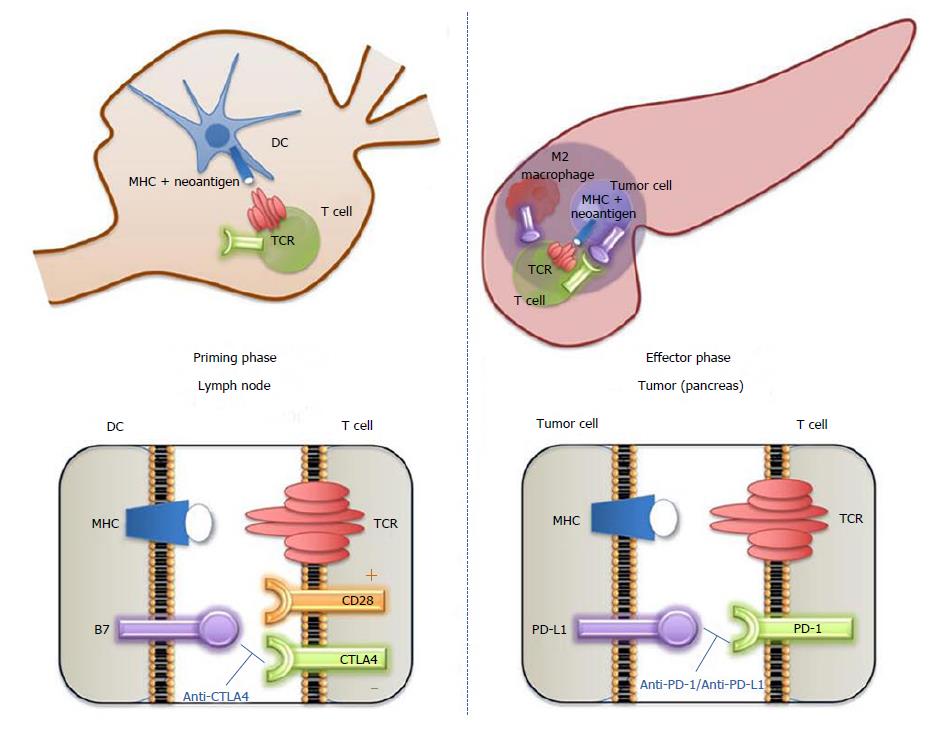
Immunotherapy has paved the way for new therapeutic opportunities in cancer. Cytotoxic T lymphocyte-associated protein 4 (CTLA-4) and programmed cell death-1 (PD-1) are receptors expressed on the surface of T-cells that regulate the duration and the amplitude of immune responses in physiological conditions[1]. CTLA-4 is involved in the priming phase (lymph node) while PD-1 and its ligand PDL-1 are implicated in the effector phase (tumor) (Figure 1). The hijacking of these immunological "checkpoints" by cancer cells is a major mechanism of immune evasion, a better understanding of which led to the clinical development of anti–CTLA-4 and anti–PD-1/PD-L1 mAb with striking efficacy in several malignancies, including chemoresistant tumors. For example, objective responses associated with prolonged survival were observed in 30%-45% of melanomas[2], 15%-20% of lung cancers[3,4], 13% of pre-treated head and neck carcinomas[5], 22%-25% of pre-treated kidney cancers[6], and more than 60% of Hodgkin lymphomas[7] following anti–PD-1/PD-L1 monotherapies, leading to their clinical approval in these indications. However, immunotherapy failed to improve the outcome of patients in some tumor types[8], notably pancreatic ductal adenocarcinoma (PDAC).
Recent epidemiological projections have predicted that PDAC will become the second leading cause of cancer-associated death in the USA and Europe by 2030[9]. PDAC is the gastrointestinal tumor with the poorest prognosis, with 80% of patients having advanced disease at diagnosis and a 5-year survival rate that does not exceed 7%[10]. PDAC is characterized by its resistance to conventional therapies (chemotherapy, targeted therapy and radiotherapy)[11]; thus innovative therapeutic options are crucially needed. Despite hopes raised by the results of immune therapies in other cancers, these strategies have so far been disappointing in PDAC. Nonetheless, an improved understanding of the biology of its microenvironment has recently provided a rationale for innovative therapeutic combinations to unlock PDAC resistance to immune therapy.
The objectives of this review are (1) to present an overview of the immune therapies that have so far been tested in PDAC, (2) to describe the main mechanisms involved in resistance to these therapies, and (3) to introduce the current strategies to overcome this resistance.
Patients with PDAC were treated with anti–PD-1/PD-L1 (pembrolizumab, atezolizumab) and anti–CTLA-4 (ipilimumab) monotherapies in three phase I[12-14] and one phase II trials[14], respectively. Overall, these studies showed no activity of checkpoint inhibitor (CPI) monotherapies in unselected patients with advanced, pre-treated, progressive PDAC (Table 1).
| Type of immunotherapy | Molecules | Trial | Phase | n | Population | Main results |
| Immune checkpoint inhibitors | PD-L1 (BMS-936559) | Brahmer et al[8] | I | 14 | Advanced PDAC Pre-treated | No objective response |
| PD-L1 (atezolizumab) | Herbst et al[12] | I | 1 | Advanced PDAC Pre-treated | No objective response | |
| PD-1 (pembrolizumab) | Patnaik et al[13] | I | 1 | Advanced PDAC Pre-treated | No objective response | |
| CTLA-4 (ipilimumab) | Royal et al[14] | II | 27 | Advanced PDAC Pre-treated | No objective response | |
| Therapeutic vaccines | GVAX | Jaffee et al[118] | I | 14 | Resected PDAC Adjuvant Combination with chemoradiotherapy | 3 patients remained disease-free for > 25 mo |
| Lutz et al[119] | II | 60 | Resected PDAC Adjuvant Combination with chemoradiotherapy | Median disease-free survival: 17.3 mo Median overall survival: 24.8 mo | ||
| Laheru et al[120] | II | 50 | Advanced PDAC Pre-treated Combination with cyclophosphamide | Median overall survival: 4.3 mo | ||
| Lutz et al[30] | Pilot Randomized | 54 | Resected PDAC Neoadjuvant and adjuvant Combination with cyclophosphamide | Arm 1: GVAX alone Arm 2: Cyclophosphamide (intravenous) + GVAX Arm 3: Cyclophosphamide (daily oral) + GVAX Intra-tumoral tertiary lymphoid aggregates PD-1 and PDL-1 upregulation | ||
| CRS 207 | Le et al[121] | I | 7 | Advanced PDAC Pre-treated | No objective response | |
| GVAX + CRS 207 | Le et al[78] | II Randomized | 90 | Advanced PDAC Pre-treated | Arm 1: Cyclophosphamide + GVAX + CRS-207 Arm 2: Cyclophosphamide + GVAX No objective response | |
| Algenpantucel-L | Hardacre et al[122] | II | 70 | Resected PDAC Adjuvant Combination with chemotherapy | Disease-free survival: 62% at 1 yr Overall survival: 86% at 1 yr | |
| Mutated KRAS peptide | Gjertsen et al[123] | I/II | 5 | Advanced PDAC Pre-treated | No objective response | |
| Gjertsen et al[124] | I/II | 48 | Advanced PDAC Pre-treated Resected PDAC Adjuvant | No objective response Median overall survival in resected PDAC: 25.6 mo | ||
| Abou-Alfa et al[125] | I | 24 | Resected PDAC Adjuvant | Median disease-free survival: 8.6 mo Median overall survival: 20.3 mo | ||
| Telomerase peptide (GV1001) | Middleton et al[126] | III Randomized | 1062 | Advanced PDAC First line Combination with chemotherapy | Arm 1: chemotherapy alone Arm 2: sequential chemo-immunotherapy Arm 3: concurrent chemo-immunotherapy No benefit on overall survival of adding vaccination to chemotherapy | |
| Oncolytic viruses | Mutated adenovirus (ONYX-15) | Hecht et al[127] | I/II | 21 | Advanced PDAC Pre-treated and first line Combination with chemotherapy | Two partial responses |
| Mulvihill et al[128] | I | 23 | Advanced PDAC Pre-treated and first line | No objective response | ||
| Anti-transforming growth factor β (TGFβ) | Anti-TGFβ2 (trabedersen) | Oettle et al[129] | I/II | 37 | Advanced PDAC Pre-treated | One complete response |
| TGFβ receptor inhibitor (galunisertib) | Melisi et al[130] | II Randomized | 156 | Advanced PDAC Pre-treated and first line Combination with chemotherapy | Arm 1: galunisertib + gemcitabine Arm 2: gemcitabine +placebo No benefit on overall survival of adding galunisertib to chemotherapy |
Nevertheless, PD-1 blockade appears to be efficient in a subset of patients with PDAC harboring a mismatch repair (MMR) deficiency. The MMR machinery is encoded by four key genes (MLH1, MSH2, MSH6, PMS2), which behave as genome safeguards by correcting base mispairs occurring during DNA replication. Loss of MMR results in drastically increased rates of somatic mutations[15,16], potentially translated into neoantigens that can be recognized by the immune system[17,18] rendering them responsive to CPI. MMR deficiency can be caused by inherited germline defect in the case of Lynch syndrome, predisposing to a spectrum of tumors [mainly, colorectal (CRC) and endometrial cancers], or emerge from somatic mutations or promoter methylation (e.g., in BRAF-mutated CRC)[19]. Microsatellite instability-high (MSI-H) is the phenotypic evidence of MMR deficiency. Recently, the use of pembrolizumab was approved for MSI-H or MMR-deficient tumors based on five clinical trials[20], which including 149 patients with tumors from 15 primary origins, mostly CRC (91/149). The objective response rate was 39.6%, including complete responses in 7.4%, and 78% of responses lasted more than 6 mo. MSI-H is thus recognized as a predictive biomarker of response to PD-1 blockade[21,22].
Six patients with PDAC were included in a multitumor expansion study of pembrolizumab (12 cancer types) with evidence of clinical benefit (one stable disease, three partial responses, and two complete responses). However, MSI-H is a rare event in PDAC[23] as illustrated by a genetic study on 385 PDAC that reported that hypermutated profiles (all related to MMR deficiency) were found in less than 2% of cases (4 out of 385)[24]. Therefore, the subset of PDAC patients eligible for CPI monotherapy is small.
Beside CPI, other immune therapy strategies (vaccines, oncolytic viruses, TGFβ inhibitors) have been tested and also remained inefficient in PDAC patients when used as monotherapies or in combination with gemcitabine chemotherapy (Table 1). Overall, except for MSI-H tumors, PDAC are considered to be resistant to single-agent immune therapy.
The “cancer-immunity cycle” theory defines three conditions that are required to obtain an effective anti-tumoral immune response[25]: tumor immunogenicity, T cell recruitment and activation.
Tumor immunogenicity: Immunogenicity is related to the degree of epitope structural difference between tumor and normal cells. The more different the epitope, the more likely to be recognized by T cells[26]. Hence, tumor-associated antigens (TAA) loosely fall into two classes based on their tumoral specificity and immunogenicity: (1) Low (differentiation antigens, overexpressed self-antigens) and (2) high (viral antigens, cancer-germline genes, and neoantigens) tumoral specificity. Neoantigens are peptides generated from non-silent coding mutations in the cancer cell genome and are highly immunogenic. Several studies have shown that tumor mutation load is linked to neoantigen burden and positively correlated with response to immunotherapy[27,28]. Pancreatic cancer has a low mutation load compared to other solid tumors, with an average mutation rate of 1 mutation per megabase (Mb) (compared to 11 mutations per Mb for melanoma), only occasionally yielding neoantigens[29]. Nevertheless, PDAC has an immunogenic capacity as reflected by the presence of T-cell infiltrates and tertiary lymphoid structures in resected PDAC samples[30-32]. Some studies suggest that although the rate of mutations is low, it is sufficient to create highly immunogenic neoantigens, notably through KRAS codon 12 mutations[33,34].
Importantly, DNA mutations do not necessarily translate into immunogenicity because both antigen presentation by major histocompatibility complex (MHC) and recognition by the T cell receptor (TCR) with a high affinity are required to induce T cell response, leading to the concept of neoantigen quality. It has been shown that the fitness of a neoantigen, i.e., its distance from the wild type sequence coupled with its binding affinity to the TCR, is correlated with the activation of T cells[35]. High-quality neoantigens (mutation-associated or microbial-like sequences) have been associated with longer survival in PDAC, highlighting the fact that the neoantigen quality outweighs the neoantigen quantity in clinical significance[36].
Determining MHC-antigenic structures (e.g., using mass spectrometry) is useful to (1) predict which neoantigen will be recognized by T cells and (2) identify actionable targets to trigger the immune response (e.g., for vaccine strategies)[37-39]. Nonetheless, such approaches are currently limited by the poor performance of neoepitope predictive algorithms. Indeed, less than 5% of predicted neoepitopes actually give rise to a biological response[34]. The Tumor Neoantigen Selection Alliance initiative is a global bioinformatics collaborative effort aiming to develop a software that can best predict immunogenic mutation-associated cancer antigens from patients’ tumor DNA[40].
T cells recruitment and activity: The release of tumor neoantigens following cell death[41] allows antigen-presenting cells (APC), such as dendritic cells to uptake and present them to T cells leading to the activation of the latter[42-44]. Secondly, T cells must be recruited into the tumor after trafficking in blood vessels[45] and passing through the endothelial wall[46]. Finally, tumor-infiltrating lymphocytes (TIL) recognize and kill tumor cells[43].
Depending on the histological pattern of TIL, tumors are classified into T-cell inflamed (also known as “hot” tumors) vs non-inflamed (“cold”) tumors, in which T cells are excluded or absent[47]. Preclinical and clinical evidence suggest that only patients who have T-cell inflamed tumors respond to CPI monotherapy[47]. Most PDAC are thought to belong to the non-inflamed tumor group, displaying low levels of TIL along with low PD-L1 expression, which can account for the poor efficacy of single-agent immune therapies[48-50].
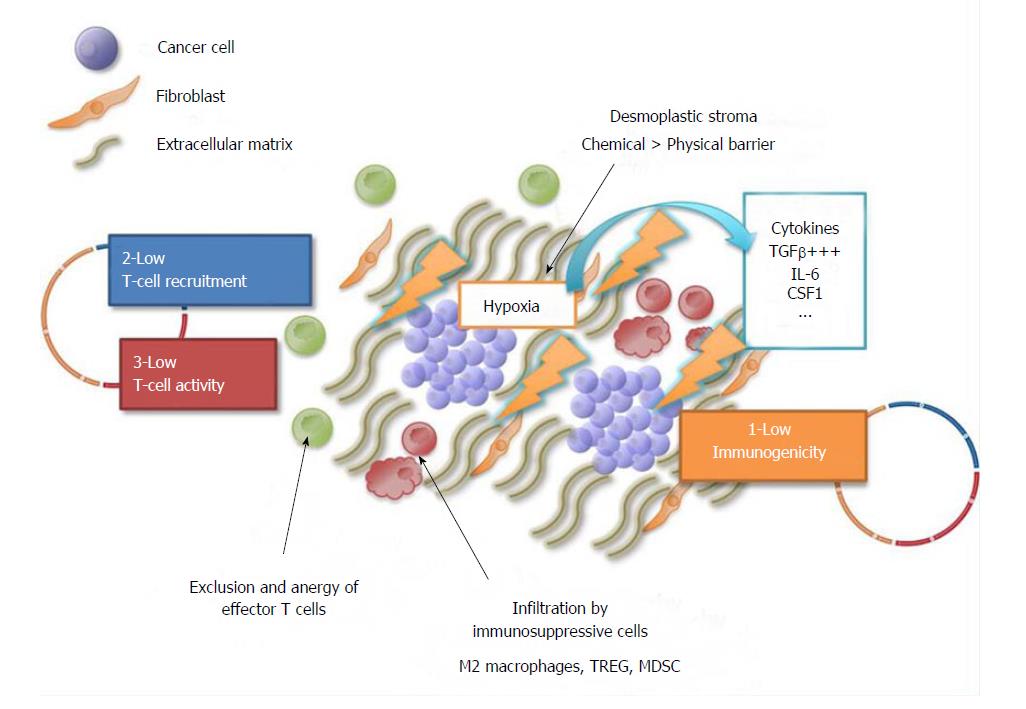
PDAC display an abundant desmoplastic stroma, the extent of which is often greater than the epithelial component of the tumor[51,52]. The stroma is a complex structure composed of extracellular matrix proteins and various cell types including cancer associated fibroblasts (CAF), endothelial cells, and immune cells[52]. This fibrotic barrier was believed to physically impede T cell infiltration[53]. However, recent work using multiplex imaging for spatial analysis of desmoplastic elements in PDAC revealed that collagen I deposits are inversely correlated with TIL numbers[54]. This observation has led to the hypothesis that the stroma may be a chemical rather than a physical barrier[55] (Figure 2). Indeed, PDAC is characterized by a high density of immunosuppressive cells including T regulatory cells (TREG) and myeloid cells [e.g. dendritic cells, myeloid derived suppressive cells (MDSC) and M2 macrophages], which are negative prognostic factors[56]. Myeloid cells release TGFβ[57], nitric oxide synthase and arginase, preventing TIL recruitment and activity[56,58]. Tumor hypoxia is a predominant driver in the recruitment of these immune cells through CAF activation[59-61]. Activated CAF then secrete immunosuppressive cytokines[62,63], such as CXCL12 and IL-6, which promote MDSC recruitment and inhibit effector T cell recruitment.
In addition, although T cell infiltration seems to be necessary for the response to immune therapy, the presence of TIL is not sufficient to induce an effective anti-tumor response[64]. Indeed, TIL activation is required. However, in PDAC, even in the presence of tumor-specific neoepitopes, T cells display a reduced activation signature[34] and most of them are PD-1–positive[65], suggesting that T cell activation is actively suppressed. Notably, not only MDSC but also TREG and CD8-positive γδT cells restrain activation of αβT cells that are directed against the tumor[66]. These deleterious TIL represent approximately 40% of CD8-positive TIL populations in PDAC and may mislead the interpretation of the biological significance of TIL in PDAC. This may enlighten some negative results showing no prognostic impact of T cell infiltration in PDAC[56,64].
Overall, given its low mutational load, low lymphocyte count, the presence of inflammatory cytokines and hypoxia, PDAC displays a unique microenvironment that is unfavorable to immune therapy according to the cancer immunogram and requires combination strategies[67].
Rational combinations: Following the failure of CPI monotherapies in PDAC, efforts have been made to develop rational combinations to overcome PDAC resistance to immune therapy. Based on the cancer immunity cycle[25], most of them combine a CPI with another agent aiming to (1) increase tumor immunogenicity; (2) increase TIL number and activity; and/or (3) attenuate immunosuppression in the tumor microenvironment. Combination therapy can employ immune therapy, conventional chemo/radiotherapy, targeted therapy, or vaccine/adoptive T-cell therapy[50,68].
Increasing tumor immunogenicity: Chemotherapeutic agents and radiotherapy may play a dual role by directly killing cancer cells, thus reducing the overall tumor burden and indirectly by releasing pro-inflammatory molecules and tumor-associated antigens (TAA) (e.g., calreticulin, ATP) which, when presented in an immunogenic fashion, may function as in situ vaccines to attract and activate T cells (so called “immunogenic death”). Among chemotherapeutic agents used in the PDAC therapeutic armamentarium, platinum-based agents and taxanes are preferential combination partners for immunotherapy because they can induce immunogenic cell death, sensitize tumor cells to immune-mediated destruction and enhance T cell activation[69-71]. Although some investigators have shown that FOLFIRI [folinic acid, 5-fluorouracil (5FU) and irinotecan combination] can be given with vaccines to CRC patients without abrogation of the immune response[72], 5FU and irinotecan have been reported to be more immunosuppressive[73]. Therefore, combining them with an immune therapy may impair the immune-mediated anti-tumor response, and a sequential design for immune therapy after induction chemotherapy using these agents may be more effective.
Tumor vaccines and oncolytic viruses both aim at increasing tumor antigen recognition by the immune system through presentation by dendritic cells[74,75]. Although relatively inefficient as monotherapies, vaccine strategies are currently explored in combination with CPI. GVAX is a granulocyte-macrophage colony-stimulating factor (GM-CSF)-secreting allogeneic PDAC vaccine. It was first evaluated in combination with anti–CTLA-4 therapy[76]. Thirty pre-treated PDAC patients were randomized to receive ipilimumab alone or combined with GVAX. The latter experienced a longer median overall survival (OS) (3.6 mo vs 5.7 mo, P = 0.07) with no additional toxicity. Furthermore, the observation that neoadjuvant GVAX was able to induce intra-tumoral tertiary lymphoid structures and upregulate PD-L1 membranous expression in resected tumor samples[30] provided a rationale for its combination with anti–PD-1. This was also supported by preclinical data in mouse models[77] showing an improved survival rate with the combination of GVAX and PD-1 blockade compared to each agent taken individually. In clinical practice, GVAX is associated to cancer vaccine CRS-207 (an attenuated form of Listeria monocytogenes) and/or cyclophosphamide (aiming at downregulating TREG) in clinical trials in the adjuvant setting[78]. GVAX/cyclophosphamide therapy is also currently being tested in PDAC in combination with nivolumab (anti–PD-1) alone (NCT02243271, NCT02451982, NCT03161379) or combined to ipilimumab (anti-CTLA-4) (NCT03190265), or with pembrolizumab (anti–PD-1) alone (NCT02648282) or combined to the indoleamine-2,3 dioxygenase (IDO, an enzyme that inhibits T cells proliferation by catalyzing the degradation of tryptophan[79]) inhibitor epacadostat (NCT03006302). Restoring the proliferation and activation of various immune cells, including T cells[80], may potentiate the response to vaccine therapy. Of note, there is also a rationale for combining GVAX with TGFβ inhibitors in preclinical models[77,81]. However, this combination has not reached clinical trials. GVAX, like peptidic “one-size-fits-all” vaccines, has to face the challenges of (1) the unique tumor antigen landscape specific to each patient and (2) the emergence of immune evasion, both of which can compromise patient response to vaccine therapy[82]. Personalized vaccine approaches are expected to partially overcome these issues but their development remains limited by their logistic complexity and high costs[82-84]. Alternatively, oncolytic viruses combine antigen presentation with the induction of a type I interferon-γ (IFN-γ) response that potentiates effector T-cell activation[74,75]. Similar to the vaccine approach, the oncolytic virus reolysin was tested in metastatic PDAC in combination with carboplatin and paclitaxel but failed to improve progression-free survival (PFS)[85]. However, a phase II study[86] explored the combination of reolysin, pembrolizumab (anti–PD-1) and chemotherapy in 11 patients with pre-treated PDAC and showed antitumor activity with a manageable safety profile. Among the 5 evaluable patients, two had stable diseases (126 and 221 d) and one had partial response lasting more than 6 mo. A phase Ib trial in combination with pembrolizumab and gemcitabine, irinotecan or leucovorin/5-fluorouracil (5-FU) is ongoing (NCT02620423).
Increase TIL recruitment and activity: Most anti–PD-1/PD-L1-based combination trials focus on converting the PDAC non-inflamed (immune-excluded or desert) microenvironment into an inflamed pattern by increasing T cells recruitment and activity.
CPI combination: The association of CTLA-4 and PD-1 antibodies resulted in an improved OS in patients with advanced melanoma compared with each agent used as monotherapy, albeit at the price of increased toxicity with 59% of patients experiencing grade 3 or 4 adverse events (vs 21%-28% with monotherapy)[87]. The PA.7 randomized phase II trial (NCT02879318) explores the combination of tremelimumab (anti–CTLA-4 mAb) and durvalumab (anti–PD-L1 mAb) with gemcitabine plus nab-paclitaxel chemotherapy vs chemotherapy alone as a first-line treatment for metastatic PDAC. Co-targeting of other immunomodulatory pathways such as IDO, OX40, CD40, the lymphocyte activation gene 3 protein (LAG3) or T cell immunoglobulin and mucin 3 (TIM3), among numerous candidates, might be as efficient and less toxic than PD-1/CTLA-4 combination[88] but remain to be explored in PDAC patients.
Combination with anti-M2/-MDSC: The CCL2-CCR2 chemokine axis induces the recruitment of immunosuppressive tumor-associated-macrophages (TAM)[89]. A CCR2 inhibitor (PF-04136309) has been tested in combination with FOLFIRINOX chemotherapy in a phase Ib study in patients with borderline resectable/locally advanced PDAC[89]. The objective response rate was 49% and disease control rate reached 97% with a manageable safety profile. Interestingly, ancillary studies showed (1) a decrease in TAM infiltration together with (2) a decrease in circulating monocytes and (3) an increase in bone marrow monocytes in patients treated with the combination, supporting the mechanistic hypothesis of a reduction in intra-tumor monocyte recruitment from the bone marrow[90].
Other inflammatory pathways have been targeted using small molecules or mAb and are currently being explored in clinical trials in combination with CPI based on promising results in mouse models. These include colony stimulating factor 1 receptor (CSF1R)[91] (NCT02777710), IL-6[92], TGFβ (NCT02734160), CCR4 (NCT02301130), CXCR2 (NCT02583477) and CXCR4/CXCL12 (NCT03168139). Nonetheless, similarly to the results obtained following pathway inhibition using tyrosine kinase inhibitors, secondary resistance due to cytokine axes compensation has emerged, leading to disease progression and pleading for combination strategies[93].
Combination with MEK inhibitors: MEK inhibition (MEK-i) was primarily developed in PDAC as a KRAS signaling inhibition strategy, given the high frequency of activating KRAS mutations in these tumors (> 90%)[94]. MEK-i failed to improve the survival rate of PDAC patients when used as monotherapy or in combination with gemcitabine[94]. However, novel perspectives are opening up for MEK-i as a combination partner with immune therapy. Indeed, MEK-i exerts multifaceted immunostimulatory effects by (1) increasing MHC-I expression and decreasing PD-L1 expression on tumor cells, (2) increasing TIL activity and survival, and (3) decreasing macrophage and MDSC infiltrates[95].
A phase Ib study (NCT01988896) has investigated the combination of cobimetinib (MEK-i) with atezolizumab (anti–PD-L1) in pre-treated metastatic CRC; durable objective responses were observed in patients with microsatellite stable (MSS)/MSI-low tumors, mostly KRAS-mutated, prompting the evaluation of this combination in PDAC in a clinical trial (NCT03193190).
Targeting tumor hypoxia: Likewise, hypoxia-targeting strategies have been tested with disappointing results in combination with gemcitabine[96]. Evofosfamide (TH-302) is a cytotoxic prodrug that is activated under hypoxic conditions, targeting hypoxic tumor areas. It is now being explored as a combination partner for immunotherapy since it can improve tumor tissue oxygenation and subsequently decrease MDSC recruitment and increase effector T cell activity[59,97]. The use of TH-302 with CPI may therefore be effective in restoring a favorable immune environment. A phase I trial is underway to study the combination of TH-302 with ipilimumab (anti-CTLA-4) in PDAC, melanoma, head and neck cancer and prostate cancer (NCT03098160).
Targeting fibroblasts and the stromal physical barrier: There have been contradictory reports on the roles of the desmoplastic stroma in PDAC (tumor-promoting vs tumor-restrictive effect). CAF elimination using sonic hedgehog inhibitors or genetic strategy for selective depletion of α-smooth muscle actin (α-SMA)-positive cells in transgenic mice resulted in aggressive and undifferentiated tumors with increased vascularization and TREG infiltration, respectively[98,99]. Clinical trials with hedgehog inhibitors in PDAC were negative for any anti-neoplastic activity[100]. Strategies then shifted toward stroma modulation rather than depletion.
Focal adhesion kinase (FAK) is a cytoplasmic tyrosine kinase protein that has been reported to be overexpressed and active in many solid tumors, including PDAC[101]. FAK is expressed by fibroblastic cells as well as tumoral, endothelial and immune cells[101], and its inhibition engenders pleiomorphic effects[102]. In preclinical models, FAK inhibition reduced fibrosis, decreased the amount of tumor-infiltrating immunosuppressive cells, and rendered the previously unresponsive KPC mouse models sensitive to PD-1 blockade[102]. Two phase I/II studies are underway to verify the benefit of this combination (NCT02546531 and NCT02758587). Other CAF-modulating or anti-fibrotic agents are also under investigation including TGFβ inhibitors (NCT02734160), PEGPH20 (NCT03193190) and vitamin D (NCT03331562) in combination with CPI. In addition, all-trans-retinoic acid (ATRA) (NCT03307148), and BET-inhibitors (NCT02711137) are being explored in combination with chemotherapy.
CAR-T cells: Adoptive cell therapy is a technology that has recently drawn increasing attention. T cells may be engineered to express a chimeric antigen receptor (CAR) in order to target specific tumor antigen[103]. This approach has already proven its effectiveness in B-cell hematological malignancies with T cells expressing CD19 CAR[104,105]. Similarly, mesothelin CAR-T therapy has been proposed in solid tumors[106]. In PDAC, this therapy led to the prolonged survival in a mouse model study[107]. Nevertheless, clinical development of this strategy in solid tumors is hampered by (1) its limited efficacy in comparison with the results seen in hematological malignancies; (2) high level of toxicity, including life-threatening immune adverse events (neurotoxicity and cytokine release syndrome); and (3) costs and logistics to be deployed on a large patient population. Next generation CAR T-cells are currently being developed to overcome these challenges[108].
Besides exploring new therapeutic avenues, it is also necessary to rethink the design of clinical immune therapy trials targeting PDAC. The clinical trial design tends to shift from traditional phase I to III development plan toward a signal detection strategy in multiple patient cohorts. In the context of an increasing number of clinical trials, there is a need to identify the most relevant combinations among the numerous candidate agents. Development of new preclinical models closer to the complex in vivo conditions should significantly improve the predictive value for therapeutic agent testing and guide the selection of the most active combinations for evaluation in clinical trials.
Second, the examples of MEK-i, vaccines, evofosfamide or TGFβ inhibitors show that it may be worth giving a second chance to some molecules that were found inactive as monotherapy.
In addition, patients with heavily pre-treated, progressive, advanced PDAC are not good candidates for immune therapy and this may partially account for failure of previous studies. These patients should possibly be excluded from immunotherapy clinical trials. Alternatively, positioning immune therapy as maintenance strategy following a course of induction chemotherapy (e.g., with FOLFIRINOX) seems to present several advantages: (1) It allows the identification and exclusion of patients with rapid tumor progression; (2) such a treatment may have induced immunogenic cell death and sensitized the tumor to CPI; and (3) given that induction chemotherapy was not interrupted due to inefficacy, it could be reintroduced at disease progression. Taken together, these elements support the development of immune therapy as maintenance therapy in patients with controlled disease.
Finally, there is a critical need for predictive biomarker identification in order to guide patient selection for immune therapy and to stratify the randomization. Meanwhile, it is necessary to assess the predictive value of already available PDAC molecular classifications in the ancillary studies of ongoing clinical trials[109-112].
PDAC is resistant to CPI monotherapy due to its unfavorable non-immune inflamed microenvironment. A better understanding of the biological mechanisms underlying PDAC immunosuppression may pave the way to innovative and promising strategies. Given the key role of the team hypoxia-TGFβ-CAF-M2/MDSC, the development of rational combinations of immunotherapy targeting these pathways and cell populations to increase intra-tumor recruitment and activation of T cells is coherent. To achieve this, we will have to reconsider inactive molecules in monotherapy, optimize the position of immunotherapy in the therapeutic sequence and develop new preclinical models to better predict therapeutic efficacy.
Furthermore, an improved understanding of the mechanisms of sensitivity and resistance to immunotherapy has revealed the increasing complexity in the tumor antigens, TIL, TREG, and MDSC landscape[113]. For instance, (1) anti-inflammatory and pro-inflammatory cytokines have counter balancing activities; (2) biological effects may be different between primary and metastatic tumor sites as illustrated by dissociated responses; (3) hypermutated tumors are more likely to respond to but also to develop resistance to CPI[114]; and (4) the immune therapy response is also dependent on the patient microbiota[115,116] and genetics[117]. Mechanisms of action of CPI remain yet to be fully elucidated. The collaboration between clinicians and researchers will be the cornerstone of future progress in this field.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: France
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chang E, Demonacos C, Schulten H S- Editor: Wang XJ L- Editor: A E- Editor: Tan WW
| 1. | Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12:252-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9936] [Cited by in RCA: 10345] [Article Influence: 795.8] [Reference Citation Analysis (34)] |
| 2. | Robert C, Schachter J, Long GV, Arance A, Grob JJ, Mortier L, Daud A, Carlino MS, McNeil C, Lotem M. Pembrolizumab versus Ipilimumab in Advanced Melanoma. N Engl J Med. 2015;372:2521-2532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4026] [Cited by in RCA: 4485] [Article Influence: 448.5] [Reference Citation Analysis (1)] |
| 3. | Brahmer J, Reckamp KL, Baas P, Crinò L, Eberhardt WE, Poddubskaya E, Antonia S, Pluzanski A, Vokes EE, Holgado E. Nivolumab versus Docetaxel in Advanced Squamous-Cell Non-Small-Cell Lung Cancer. N Engl J Med. 2015;373:123-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5686] [Cited by in RCA: 6738] [Article Influence: 673.8] [Reference Citation Analysis (0)] |
| 4. | Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, Chow LQ, Vokes EE, Felip E, Holgado E. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med. 2015;373:1627-1639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6945] [Cited by in RCA: 7534] [Article Influence: 753.4] [Reference Citation Analysis (0)] |
| 5. | Ferris RL, Blumenschein G Jr, Fayette J, Guigay J, Colevas AD, Licitra L, Harrington K, Kasper S, Vokes EE, Even C, Worden F, Saba NF, Iglesias Docampo LC, Haddad R, Rordorf T, Kiyota N, Tahara M, Monga M, Lynch M, Geese WJ, Kopit J, Shaw JW, Gillison ML. Nivolumab for Recurrent Squamous-Cell Carcinoma of the Head and Neck. N Engl J Med. 2016;375:1856-1867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3044] [Cited by in RCA: 3693] [Article Influence: 410.3] [Reference Citation Analysis (0)] |
| 6. | Motzer RJ, Escudier B, McDermott DF, George S, Hammers HJ, Srinivas S, Tykodi SS, Sosman JA, Procopio G, Plimack ER. Nivolumab versus Everolimus in Advanced Renal-Cell Carcinoma. N Engl J Med. 2015;373:1803-1813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4375] [Cited by in RCA: 4602] [Article Influence: 460.2] [Reference Citation Analysis (0)] |
| 7. | Ansell SM, Lesokhin AM, Borrello I, Halwani A, Scott EC, Gutierrez M, Schuster SJ, Millenson MM, Cattry D, Freeman GJ. PD-1 blockade with nivolumab in relapsed or refractory Hodgkin's lymphoma. N Engl J Med. 2015;372:311-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2598] [Cited by in RCA: 2802] [Article Influence: 280.2] [Reference Citation Analysis (0)] |
| 8. | Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, Drake CG, Camacho LH, Kauh J, Odunsi K. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366:2455-2465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5599] [Cited by in RCA: 6283] [Article Influence: 483.3] [Reference Citation Analysis (0)] |
| 9. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9172] [Cited by in RCA: 9957] [Article Influence: 995.7] [Reference Citation Analysis (0)] |
| 10. | Ryan DP, Hong TS, Bardeesy N. Pancreatic adenocarcinoma. N Engl J Med. 2014;371:1039-1049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1500] [Cited by in RCA: 1710] [Article Influence: 155.5] [Reference Citation Analysis (0)] |
| 11. | Neuzillet C, Tijeras-Raballand A, Bourget P, Cros J, Couvelard A, Sauvanet A, Vullierme MP, Tournigand C, Hammel P. State of the art and future directions of pancreatic ductal adenocarcinoma therapy. Pharmacol Ther. 2015;155:80-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 82] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 12. | Herbst RS, Soria JC, Kowanetz M, Fine GD, Hamid O, Gordon MS, Sosman JA, McDermott DF, Powderly JD, Gettinger SN. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature. 2014;515:563-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3965] [Cited by in RCA: 4182] [Article Influence: 380.2] [Reference Citation Analysis (0)] |
| 13. | Patnaik A, Kang SP, Rasco D, Papadopoulos KP, Elassaiss-Schaap J, Beeram M, Drengler R, Chen C, Smith L, Espino G. Phase I Study of Pembrolizumab (MK-3475; Anti-PD-1 Monoclonal Antibody) in Patients with Advanced Solid Tumors. Clin Cancer Res. 2015;21:4286-4293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 465] [Cited by in RCA: 628] [Article Influence: 62.8] [Reference Citation Analysis (0)] |
| 14. | Royal RE, Levy C, Turner K, Mathur A, Hughes M, Kammula US, Sherry RM, Topalian SL, Yang JC, Lowy I. Phase 2 trial of single agent Ipilimumab (anti-CTLA-4) for locally advanced or metastatic pancreatic adenocarcinoma. J Immunother. 2010;33:828-833. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 964] [Cited by in RCA: 977] [Article Influence: 65.1] [Reference Citation Analysis (0)] |
| 15. | Timmermann B, Kerick M, Roehr C, Fischer A, Isau M, Boerno ST, Wunderlich A, Barmeyer C, Seemann P, Koenig J. Somatic mutation profiles of MSI and MSS colorectal cancer identified by whole exome next generation sequencing and bioinformatics analysis. PLoS One. 2010;5:e15661. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 168] [Cited by in RCA: 178] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 16. | Eshleman JR, Lang EZ, Bowerfind GK, Parsons R, Vogelstein B, Willson JK, Veigl ML, Sedwick WD, Markowitz SD. Increased mutation rate at the hprt locus accompanies microsatellite instability in colon cancer. Oncogene. 1995;10:33-37. [PubMed] |
| 17. | Segal NH, Parsons DW, Peggs KS, Velculescu V, Kinzler KW, Vogelstein B, Allison JP. Epitope landscape in breast and colorectal cancer. Cancer Res. 2008;68:889-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 341] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 18. | Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, Skora AD, Luber BS, Azad NS, Laheru D. PD-1 Blockade in Tumors with Mismatch-Repair Deficiency. N Engl J Med. 2015;372:2509-2520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6096] [Cited by in RCA: 7239] [Article Influence: 723.9] [Reference Citation Analysis (0)] |
| 19. | Herman JG, Umar A, Polyak K, Graff JR, Ahuja N, Issa JP, Markowitz S, Willson JK, Hamilton SR, Kinzler KW. Incidence and functional consequences of hMLH1 promoter hypermethylation in colorectal carcinoma. Proc Natl Acad Sci USA. 1998;95:6870-6875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1343] [Cited by in RCA: 1372] [Article Influence: 50.8] [Reference Citation Analysis (0)] |
| 20. | FDA News Release. FDA approves first cancer treatment for any solid tumor with a specific genetic feature. 2017. Accessed June 12. 2017; Available from: www. fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm560167. htm. |
| 21. | Chang L, Chang M, Chang HM, Chang F. Microsatellite Instability: A Predictive Biomarker for Cancer Immunotherapy. Appl Immunohistochem Mol Morphol. 2018;26:e15-e21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 256] [Article Influence: 36.6] [Reference Citation Analysis (0)] |
| 22. | Dudley JC, Lin MT, Le DT, Eshleman JR. Microsatellite Instability as a Biomarker for PD-1 Blockade. Clin Cancer Res. 2016;22:813-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 488] [Cited by in RCA: 672] [Article Influence: 74.7] [Reference Citation Analysis (0)] |
| 23. | Laghi L, Beghelli S, Spinelli A, Bianchi P, Basso G, Di Caro G, Brecht A, Celesti G, Turri G, Bersani S. Irrelevance of microsatellite instability in the epidemiology of sporadic pancreatic ductal adenocarcinoma. PLoS One. 2012;7:e46002. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 24. | Humphris JL, Patch AM, Nones K, Bailey PJ, Johns AL, McKay S, Chang DK, Miller DK, Pajic M, Kassahn KS. Hypermutation In Pancreatic Cancer. Gastroenterology. 2017;152:68-74.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 165] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 25. | Chen DS, Mellman I. Oncology meets immunology: the cancer-immunity cycle. Immunity. 2013;39:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3297] [Cited by in RCA: 4767] [Article Influence: 397.3] [Reference Citation Analysis (1)] |
| 26. | Schumacher TN, Schreiber RD. Neoantigens in cancer immunotherapy. Science. 2015;348:69-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2935] [Cited by in RCA: 3571] [Article Influence: 357.1] [Reference Citation Analysis (0)] |
| 27. | Brown SD, Warren RL, Gibb EA, Martin SD, Spinelli JJ, Nelson BH, Holt RA. Neo-antigens predicted by tumor genome meta-analysis correlate with increased patient survival. Genome Res. 2014;24:743-750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 448] [Cited by in RCA: 483] [Article Influence: 43.9] [Reference Citation Analysis (0)] |
| 28. | Rooney MS, Shukla SA, Wu CJ, Getz G, Hacohen N. Molecular and genetic properties of tumors associated with local immune cytolytic activity. Cell. 2015;160:48-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2009] [Cited by in RCA: 2773] [Article Influence: 277.3] [Reference Citation Analysis (0)] |
| 29. | Alexandrov LB, Nik-Zainal S, Wedge DC, Aparicio SA, Behjati S, Biankin AV, Bignell GR, Bolli N, Borg A, Børresen-Dale AL. Signatures of mutational processes in human cancer. Nature. 2013;500:415-421. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7533] [Cited by in RCA: 7308] [Article Influence: 609.0] [Reference Citation Analysis (1)] |
| 30. | Lutz ER, Wu AA, Bigelow E, Sharma R, Mo G, Soares K, Solt S, Dorman A, Wamwea A, Yager A. Immunotherapy converts nonimmunogenic pancreatic tumors into immunogenic foci of immune regulation. Cancer Immunol Res. 2014;2:616-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 415] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 31. | Poschke I, Faryna M, Bergmann F, Flossdorf M, Lauenstein C, Hermes J, Hinz U, Hank T, Ehrenberg R, Volkmar M. Identification of a tumor-reactive T-cell repertoire in the immune infiltrate of patients with resectable pancreatic ductal adenocarcinoma. Oncoimmunology. 2016;5:e1240859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 75] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 32. | Hiraoka N, Ino Y, Yamazaki-Itoh R, Kanai Y, Kosuge T, Shimada K. Intratumoral tertiary lymphoid organ is a favourable prognosticator in patients with pancreatic cancer. Br J Cancer. 2015;112:1782-1790. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 155] [Cited by in RCA: 278] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 33. | Wang QJ, Yu Z, Griffith K, Hanada K, Restifo NP, Yang JC. Identification of T-cell Receptors Targeting KRAS-Mutated Human Tumors. Cancer Immunol Res. 2016;4:204-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 187] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 34. | Bailey P, Chang DK, Forget MA, Lucas FA, Alvarez HA, Haymaker C, Chattopadhyay C, Kim SH, Ekmekcioglu S, Grimm EA. Exploiting the neoantigen landscape for immunotherapy of pancreatic ductal adenocarcinoma. Sci Rep. 2016;6:35848. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 129] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 35. | Yarchoan M, Johnson BA 3rd, Lutz ER, Laheru DA, Jaffee EM. Targeting neoantigens to augment antitumour immunity. Nat Rev Cancer. 2017;17:209-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 524] [Cited by in RCA: 668] [Article Influence: 83.5] [Reference Citation Analysis (0)] |
| 36. | Balachandran VP, Łuksza M, Zhao JN, Makarov V, Moral JA, Remark R, Herbst B, Askan G, Bhanot U, Senbabaoglu Y. Identification of unique neoantigen qualities in long-term survivors of pancreatic cancer. Nature. 2017;551:512-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 920] [Cited by in RCA: 879] [Article Influence: 109.9] [Reference Citation Analysis (0)] |
| 37. | Gubin MM, Zhang X, Schuster H, Caron E, Ward JP, Noguchi T, Ivanova Y, Hundal J, Arthur CD, Krebber WJ. Checkpoint blockade cancer immunotherapy targets tumour-specific mutant antigens. Nature. 2014;515:577-581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1611] [Cited by in RCA: 1606] [Article Influence: 146.0] [Reference Citation Analysis (0)] |
| 38. | Lu YC, Yao X, Crystal JS, Li YF, El-Gamil M, Gross C, Davis L, Dudley ME, Yang JC, Samuels Y. Efficient identification of mutated cancer antigens recognized by T cells associated with durable tumor regressions. Clin Cancer Res. 2014;20:3401-3410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 315] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 39. | Łuksza M, Riaz N, Makarov V, Balachandran VP, Hellmann MD, Solovyov A, Rizvi NA, Merghoub T, Levine AJ, Chan TA. A neoantigen fitness model predicts tumour response to checkpoint blockade immunotherapy. Nature. 2017;551:517-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 402] [Cited by in RCA: 496] [Article Influence: 62.0] [Reference Citation Analysis (0)] |
| 40. | The problem with neoantigen prediction. Nat Biotechnol. 2017;35:97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 106] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 41. | Ferguson TA, Choi J, Green DR. Armed response: how dying cells influence T-cell functions. Immunol Rev. 2011;241:77-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 80] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 42. | Lippitz BE, Harris RA. Cytokine patterns in cancer patients: A review of the correlation between interleukin 6 and prognosis. Oncoimmunology. 2016;5:e1093722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 120] [Cited by in RCA: 177] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 43. | Mellman I, Coukos G, Dranoff G. Cancer immunotherapy comes of age. Nature. 2011;480:480-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2348] [Cited by in RCA: 2906] [Article Influence: 207.6] [Reference Citation Analysis (0)] |
| 44. | Franciszkiewicz K, Boissonnas A, Boutet M, Combadière C, Mami-Chouaib F. Role of chemokines and chemokine receptors in shaping the effector phase of the antitumor immune response. Cancer Res. 2012;72:6325-6332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 183] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 45. | Peng W, Liu C, Xu C, Lou Y, Chen J, Yang Y, Yagita H, Overwijk WW, Lizée G, Radvanyi L. PD-1 blockade enhances T-cell migration to tumors by elevating IFN-γ inducible chemokines. Cancer Res. 2012;72:5209-5218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 347] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 46. | Franciszkiewicz K, Le Floc'h A, Boutet M, Vergnon I, Schmitt A, Mami-Chouaib F. CD103 or LFA-1 engagement at the immune synapse between cytotoxic T cells and tumor cells promotes maturation and regulates T-cell effector functions. Cancer Res. 2013;73:617-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 144] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 47. | Hegde PS, Karanikas V, Evers S. The Where, the When, and the How of Immune Monitoring for Cancer Immunotherapies in the Era of Checkpoint Inhibition. Clin Cancer Res. 2016;22:1865-1874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 462] [Cited by in RCA: 684] [Article Influence: 76.0] [Reference Citation Analysis (0)] |
| 48. | Beatty GL, Eghbali S, Kim R. Deploying Immunotherapy in Pancreatic Cancer: Defining Mechanisms of Response and Resistance. Am Soc Clin Oncol Educ Book. 2017;37:267-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 49. | Teng MW, Ngiow SF, Ribas A, Smyth MJ. Classifying Cancers Based on T-cell Infiltration and PD-L1. Cancer Res. 2015;75:2139-2145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 879] [Cited by in RCA: 1165] [Article Influence: 116.5] [Reference Citation Analysis (0)] |
| 50. | Delitto D, Wallet SM, Hughes SJ. Targeting tumor tolerance: A new hope for pancreatic cancer therapy? Pharmacol Ther. 2016;166:9-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 51. | Erkan M, Hausmann S, Michalski CW, Fingerle AA, Dobritz M, Kleeff J, Friess H. The role of stroma in pancreatic cancer: diagnostic and therapeutic implications. Nat Rev Gastroenterol Hepatol. 2012;9:454-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 426] [Cited by in RCA: 491] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 52. | Neesse A, Algül H, Tuveson DA, Gress TM. Stromal biology and therapy in pancreatic cancer: a changing paradigm. Gut. 2015;64:1476-1484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 419] [Article Influence: 41.9] [Reference Citation Analysis (0)] |
| 53. | Watt J, Kocher HM. The desmoplastic stroma of pancreatic cancer is a barrier to immune cell infiltration. Oncoimmunology. 2013;2:e26788. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 72] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 54. | Carstens JL, Correa de Sampaio P, Yang D, Barua S, Wang H, Rao A, Allison JP, LeBleu VS, Kalluri R. Spatial computation of intratumoral T cells correlates with survival of patients with pancreatic cancer. Nat Commun. 2017;8:15095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 287] [Cited by in RCA: 478] [Article Influence: 59.8] [Reference Citation Analysis (0)] |
| 55. | Turley SJ, Cremasco V, Astarita JL. Immunological hallmarks of stromal cells in the tumour microenvironment. Nat Rev Immunol. 2015;15:669-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 575] [Cited by in RCA: 808] [Article Influence: 80.8] [Reference Citation Analysis (0)] |
| 56. | Tsujikawa T, Kumar S, Borkar RN, Azimi V, Thibault G, Chang YH, Balter A, Kawashima R, Choe G, Sauer D. Quantitative Multiplex Immunohistochemistry Reveals Myeloid-Inflamed Tumor-Immune Complexity Associated with Poor Prognosis. Cell Rep. 2017;19:203-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 442] [Article Influence: 55.3] [Reference Citation Analysis (0)] |
| 57. | Principe DR, DeCant B, Mascariñas E, Wayne EA, Diaz AM, Akagi N, Hwang R, Pasche B, Dawson DW, Fang D. TGFβ Signaling in the Pancreatic Tumor Microenvironment Promotes Fibrosis and Immune Evasion to Facilitate Tumorigenesis. Cancer Res. 2016;76:2525-2539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 161] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 58. | Beatty GL, Winograd R, Evans RA, Long KB, Luque SL, Lee JW, Clendenin C, Gladney WL, Knoblock DM, Guirnalda PD. Exclusion of T Cells From Pancreatic Carcinomas in Mice Is Regulated by Ly6C(low) F4/80(+) Extratumoral Macrophages. Gastroenterology. 2015;149:201-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 226] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 59. | Chouaib S, Noman MZ, Kosmatopoulos K, Curran MA. Hypoxic stress: obstacles and opportunities for innovative immunotherapy of cancer. Oncogene. 2017;36:439-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 277] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 60. | Mariathasan S, Turley SJ, Nickles D, Castiglioni A, Yuen K, Wang Y, Kadel EE III, Koeppen H, Astarita JL, Cubas R. TGFβ attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature. 2018;554:544-548. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3113] [Cited by in RCA: 3649] [Article Influence: 521.3] [Reference Citation Analysis (1)] |
| 61. | Palazon A, Goldrath AW, Nizet V, Johnson RS. HIF transcription factors, inflammation, and immunity. Immunity. 2014;41:518-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 669] [Cited by in RCA: 887] [Article Influence: 88.7] [Reference Citation Analysis (1)] |
| 62. | Kalluri R. The biology and function of fibroblasts in cancer. Nat Rev Cancer. 2016;16:582-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2209] [Cited by in RCA: 2941] [Article Influence: 326.8] [Reference Citation Analysis (0)] |
| 63. | Feig C, Jones JO, Kraman M, Wells RJ, Deonarine A, Chan DS, Connell CM, Roberts EW, Zhao Q, Caballero OL. Targeting CXCL12 from FAP-expressing carcinoma-associated fibroblasts synergizes with anti-PD-L1 immunotherapy in pancreatic cancer. Proc Natl Acad Sci USA. 2013;110:20212-20217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1566] [Cited by in RCA: 1553] [Article Influence: 129.4] [Reference Citation Analysis (0)] |
| 64. | Knudsen ES, Vail P, Balaji U, Ngo H, Botros IW, Makarov V, Riaz N, Balachandran V, Leach S, Thompson DM. Stratification of Pancreatic Ductal Adenocarcinoma: Combinatorial Genetic, Stromal, and Immunologic Markers. Clin Cancer Res. 2017;23:4429-4440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 144] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 65. | Shen T, Zhou L, Shen H, Shi C, Jia S, Ding GP, Cao L. Prognostic value of programmed cell death protein 1 expression on CD8+ T lymphocytes in pancreatic cancer. Sci Rep. 2017;7:7848. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 66. | Daley D, Zambirinis CP, Seifert L, Akkad N, Mohan N, Werba G, Barilla R, Torres-Hernandez A, Hundeyin M, Mani VRK. γδ T Cells Support Pancreatic Oncogenesis by Restraining αβ T Cell Activation. Cell. 2016;166:1485-1499.e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 274] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 67. | Blank CU, Haanen JB, Ribas A, Schumacher TN. CANCER IMMUNOLOGY. The "cancer immunogram". Science. 2016;352:658-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 502] [Cited by in RCA: 578] [Article Influence: 64.2] [Reference Citation Analysis (0)] |
| 68. | Smyth MJ, Ngiow SF, Ribas A, Teng MW. Combination cancer immunotherapies tailored to the tumour microenvironment. Nat Rev Clin Oncol. 2016;13:143-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 571] [Cited by in RCA: 707] [Article Influence: 70.7] [Reference Citation Analysis (0)] |
| 69. | Duffy AG, Greten TF. Immunological off-target effects of standard treatments in gastrointestinal cancers. Ann Oncol. 2014;25:24-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 70. | Bracci L, Schiavoni G, Sistigu A, Belardelli F. Immune-based mechanisms of cytotoxic chemotherapy: implications for the design of novel and rationale-based combined treatments against cancer. Cell Death Differ. 2014;21:15-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 687] [Cited by in RCA: 704] [Article Influence: 64.0] [Reference Citation Analysis (0)] |
| 71. | Di Caro G, Cortese N, Castino GF, Grizzi F, Gavazzi F, Ridolfi C, Capretti G, Mineri R, Todoric J, Zerbi A. Dual prognostic significance of tumour-associated macrophages in human pancreatic adenocarcinoma treated or untreated with chemotherapy. Gut. 2016;65:1710-1720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 207] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 72. | Harrop R, Drury N, Shingler W, Chikoti P, Redchenko I, Carroll MW, Kingsman SM, Naylor S, Griffiths R, Steven N. Vaccination of colorectal cancer patients with TroVax given alongside chemotherapy (5-fluorouracil, leukovorin and irinotecan) is safe and induces potent immune responses. Cancer Immunol Immunother. 2008;57:977-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 59] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 73. | Kanterman J, Sade-Feldman M, Biton M, Ish-Shalom E, Lasry A, Goldshtein A, Hubert A, Baniyash M. Adverse immunoregulatory effects of 5FU and CPT11 chemotherapy on myeloid-derived suppressor cells and colorectal cancer outcomes. Cancer Res. 2014;74:6022-6035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 141] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 74. | Kohlhapp FJ, Kaufman HL. Molecular Pathways: Mechanism of Action for Talimogene Laherparepvec, a New Oncolytic Virus Immunotherapy. Clin Cancer Res. 2016;22:1048-1054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 226] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 75. | Kaufman HL, Kohlhapp FJ, Zloza A. Oncolytic viruses: a new class of immunotherapy drugs. Nat Rev Drug Discov. 2015;14:642-662. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 968] [Cited by in RCA: 1078] [Article Influence: 107.8] [Reference Citation Analysis (0)] |
| 76. | Le DT, Lutz E, Uram JN, Sugar EA, Onners B, Solt S, Zheng L, Diaz LA Jr, Donehower RC, Jaffee EM, Laheru DA. Evaluation of ipilimumab in combination with allogeneic pancreatic tumor cells transfected with a GM-CSF gene in previously treated pancreatic cancer. J Immunother. 2013;36:382-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 362] [Cited by in RCA: 418] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 77. | Soares KC, Rucki AA, Wu AA, Olino K, Xiao Q, Chai Y, Wamwea A, Bigelow E, Lutz E, Liu L. PD-1/PD-L1 blockade together with vaccine therapy facilitates effector T-cell infiltration into pancreatic tumors. J Immunother. 2015;38:1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 319] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 78. | Le DT, Wang-Gillam A, Picozzi V, Greten TF, Crocenzi T, Springett G, Morse M, Zeh H, Cohen D, Fine RL. Safety and survival with GVAX pancreas prime and Listeria Monocytogenes-expressing mesothelin (CRS-207) boost vaccines for metastatic pancreatic cancer. J Clin Oncol. 2015;33:1325-1333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 386] [Cited by in RCA: 462] [Article Influence: 46.2] [Reference Citation Analysis (0)] |
| 79. | Uyttenhove C, Pilotte L, Théate I, Stroobant V, Colau D, Parmentier N, Boon T, Van den Eynde BJ. Evidence for a tumoral immune resistance mechanism based on tryptophan degradation by indoleamine 2,3-dioxygenase. Nat Med. 2003;9:1269-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1642] [Cited by in RCA: 1742] [Article Influence: 79.2] [Reference Citation Analysis (0)] |
| 80. | Liu X, Shin N, Koblish HK, Yang G, Wang Q, Wang K, Leffet L, Hansbury MJ, Thomas B, Rupar M. Selective inhibition of IDO1 effectively regulates mediators of antitumor immunity. Blood. 2010;115:3520-3530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 402] [Cited by in RCA: 444] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 81. | Neuzillet C, de Gramont A, Tijeras-Raballand A, de Mestier L, Cros J, Faivre S, Raymond E. Perspectives of TGF-β inhibition in pancreatic and hepatocellular carcinomas. Oncotarget. 2014;5:78-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 118] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 82. | van der Burg SH, Arens R, Ossendorp F, van Hall T, Melief CJ. Vaccines for established cancer: overcoming the challenges posed by immune evasion. Nat Rev Cancer. 2016;16:219-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 495] [Cited by in RCA: 536] [Article Influence: 59.6] [Reference Citation Analysis (0)] |
| 83. | Desrichard A, Snyder A, Chan TA. Cancer Neoantigens and Applications for Immunotherapy. Clin Cancer Res. 2016;22:807-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 178] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 84. | Gilboa E. The promise of cancer vaccines. Nat Rev Cancer. 2004;4:401-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 189] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 85. | Noonan AM, Farren MR, Geyer SM, Huang Y, Tahiri S, Ahn D, Mikhail S, Ciombor KK, Pant S, Aparo S. Randomized Phase 2 Trial of the Oncolytic Virus Pelareorep (Reolysin) in Upfront Treatment of Metastatic Pancreatic Adenocarcinoma. Mol Ther. 2016;24:1150-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 112] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 86. | Mahalingam D, Fountzilas C, Moseley JL, Noronha N, Cheetham K, Dzugalo A, Nuovo G, Gutierrez A, Arora SP. A study of REOLYSIN in combination with pembrolizumab and chemotherapy in patients (pts) with relapsed metastatic adenocarcinoma of the pancreas (MAP). J Clin Oncol. 2017;35 suppl; abstr e15753. |
| 87. | Wolchok JD, Chiarion-Sileni V, Gonzalez R, Rutkowski P, Grob JJ, Cowey CL, Lao CD, Wagstaff J, Schadendorf D, Ferrucci PF. Overall Survival with Combined Nivolumab and Ipilimumab in Advanced Melanoma. N Engl J Med. 2017;377:1345-1356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2362] [Cited by in RCA: 2779] [Article Influence: 347.4] [Reference Citation Analysis (0)] |
| 88. | Mahoney KM, Rennert PD, Freeman GJ. Combination cancer immunotherapy and new immunomodulatory targets. Nat Rev Drug Discov. 2015;14:561-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 832] [Cited by in RCA: 1007] [Article Influence: 100.7] [Reference Citation Analysis (1)] |
| 89. | Nywening TM, Wang-Gillam A, Sanford DE, Belt BA, Panni RZ, Cusworth BM, Toriola AT, Nieman RK, Worley LA, Yano M. Targeting tumour-associated macrophages with CCR2 inhibition in combination with FOLFIRINOX in patients with borderline resectable and locally advanced pancreatic cancer: a single-centre, open-label, dose-finding, non-randomised, phase 1b trial. Lancet Oncol. 2016;17:651-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 425] [Cited by in RCA: 599] [Article Influence: 66.6] [Reference Citation Analysis (0)] |
| 90. | Nywening TM, Belt BA, Cullinan DR, Panni RZ, Han BJ, Sanford DE, Jacobs RC, Ye J, Patel AA, Gillanders WE. Targeting both tumour-associated CXCR2+ neutrophils and CCR2+ macrophages disrupts myeloid recruitment and improves chemotherapeutic responses in pancreatic ductal adenocarcinoma. Gut. 2018;67:1112-1123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 247] [Cited by in RCA: 372] [Article Influence: 53.1] [Reference Citation Analysis (0)] |
| 91. | Zhu Y, Knolhoff BL, Meyer MA, Nywening TM, West BL, Luo J, Wang-Gillam A, Goedegebuure SP, Linehan DC, DeNardo DG. CSF1/CSF1R blockade reprograms tumor-infiltrating macrophages and improves response to T-cell checkpoint immunotherapy in pancreatic cancer models. Cancer Res. 2014;74:5057-5069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 971] [Cited by in RCA: 1015] [Article Influence: 92.3] [Reference Citation Analysis (0)] |
| 92. | Mace TA, Shakya R, Pitarresi JR, Swanson B, McQuinn CW, Loftus S, Nordquist E, Cruz-Monserrate Z, Yu L, Young G. IL-6 and PD-L1 antibody blockade combination therapy reduces tumour progression in murine models of pancreatic cancer. Gut. 2018;67:320-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 397] [Article Influence: 56.7] [Reference Citation Analysis (0)] |
| 93. | Bonapace L, Coissieux MM, Wyckoff J, Mertz KD, Varga Z, Junt T, Bentires-Alj M. Cessation of CCL2 inhibition accelerates breast cancer metastasis by promoting angiogenesis. Nature. 2014;515:130-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 512] [Cited by in RCA: 547] [Article Influence: 49.7] [Reference Citation Analysis (0)] |
| 94. | Neuzillet C, Hammel P, Tijeras-Raballand A, Couvelard A, Raymond E. Targeting the Ras-ERK pathway in pancreatic adenocarcinoma. Cancer Metastasis Rev. 2013;32:147-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 95. | Zhang Y, Velez-Delgado A, Mathew E, Li D, Mendez FM, Flannagan K, Rhim AD, Simeone DM, Beatty GL, Pasca di Magliano M. Myeloid cells are required for PD-1/PD-L1 checkpoint activation and the establishment of an immunosuppressive environment in pancreatic cancer. Gut. 2017;66:124-136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 237] [Cited by in RCA: 268] [Article Influence: 33.5] [Reference Citation Analysis (0)] |
| 96. | Van Cutsem E, Lenz H-J, Furuse J, Tabernero J, Heinemann V, Ioka T, Bazin I, Ueno M, Csõszi T, Wasan H. MAESTRO: A randomized, double-blind phase III study of evofosfamide (Evo) in combination with gemcitabine (Gem) in previously untreated patients (pts) with metastatic or locally advanced unresectable pancreatic ductal adenocarcinoma (PDAC). J Clin Oncol. 2016;34:4007-4007. [RCA] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 97. | Saggar JK, Tannock IF. Chemotherapy Rescues Hypoxic Tumor Cells and Induces Their Reoxygenation and Repopulation-An Effect That Is Inhibited by the Hypoxia-Activated Prodrug TH-302. Clin Cancer Res. 2015;21:2107-2114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 98. | Rhim AD, Oberstein PE, Thomas DH, Mirek ET, Palermo CF, Sastra SA, Dekleva EN, Saunders T, Becerra CP, Tattersall IW. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell. 2014;25:735-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1359] [Cited by in RCA: 1640] [Article Influence: 149.1] [Reference Citation Analysis (0)] |
| 99. | Özdemir BC, Pentcheva-Hoang T, Carstens JL, Zheng X, Wu CC, Simpson TR, Laklai H, Sugimoto H, Kahlert C, Novitskiy SV. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell. 2014;25:719-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1955] [Cited by in RCA: 1910] [Article Influence: 173.6] [Reference Citation Analysis (1)] |
| 100. | Catenacci DV, Junttila MR, Karrison T, Bahary N, Horiba MN, Nattam SR, Marsh R, Wallace J, Kozloff M, Rajdev L. Randomized Phase Ib/II Study of Gemcitabine Plus Placebo or Vismodegib, a Hedgehog Pathway Inhibitor, in Patients With Metastatic Pancreatic Cancer. J Clin Oncol. 2015;33:4284-4292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 407] [Cited by in RCA: 430] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 101. | Sulzmaier FJ, Jean C, Schlaepfer DD. FAK in cancer: mechanistic findings and clinical applications. Nat Rev Cancer. 2014;14:598-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 851] [Cited by in RCA: 1042] [Article Influence: 94.7] [Reference Citation Analysis (0)] |
| 102. | Jiang H, Hegde S, Knolhoff BL, Zhu Y, Herndon JM, Meyer MA, Nywening TM, Hawkins WG, Shapiro IM, Weaver DT. Targeting focal adhesion kinase renders pancreatic cancers responsive to checkpoint immunotherapy. Nat Med. 2016;22:851-860. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 556] [Cited by in RCA: 774] [Article Influence: 86.0] [Reference Citation Analysis (0)] |
| 103. | Sadelain M, Rivière I, Brentjens R. Targeting tumours with genetically enhanced T lymphocytes. Nat Rev Cancer. 2003;3:35-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 373] [Cited by in RCA: 397] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 104. | Kochenderfer JN, Dudley ME, Kassim SH, Somerville RP, Carpenter RO, Stetler-Stevenson M, Yang JC, Phan GQ, Hughes MS, Sherry RM. Chemotherapy-refractory diffuse large B-cell lymphoma and indolent B-cell malignancies can be effectively treated with autologous T cells expressing an anti-CD19 chimeric antigen receptor. J Clin Oncol. 2015;33:540-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1262] [Cited by in RCA: 1284] [Article Influence: 128.4] [Reference Citation Analysis (0)] |
| 105. | Lee DW, Kochenderfer JN, Stetler-Stevenson M, Cui YK, Delbrook C, Feldman SA, Fry TJ, Orentas R, Sabatino M, Shah NN. T cells expressing CD19 chimeric antigen receptors for acute lymphoblastic leukaemia in children and young adults: a phase 1 dose-escalation trial. Lancet. 2015;385:517-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2061] [Cited by in RCA: 2320] [Article Influence: 232.0] [Reference Citation Analysis (0)] |
| 106. | Morello A, Sadelain M, Adusumilli PS. Mesothelin-Targeted CARs: Driving T Cells to Solid Tumors. Cancer Discov. 2016;6:133-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 376] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 107. | Stromnes IM, Schmitt TM, Hulbert A, Brockenbrough JS, Nguyen H, Cuevas C, Dotson AM, Tan X, Hotes JL, Greenberg PD. T Cells Engineered against a Native Antigen Can Surmount Immunologic and Physical Barriers to Treat Pancreatic Ductal Adenocarcinoma. Cancer Cell. 2015;28:638-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 158] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 108. | June CH, O'Connor RS, Kawalekar OU, Ghassemi S, Milone MC. CAR T cell immunotherapy for human cancer. Science. 2018;359:1361-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1289] [Cited by in RCA: 2059] [Article Influence: 294.1] [Reference Citation Analysis (0)] |
| 109. | Collisson EA, Sadanandam A, Olson P, Gibb WJ, Truitt M, Gu S, Cooc J, Weinkle J, Kim GE, Jakkula L. Subtypes of pancreatic ductal adenocarcinoma and their differing responses to therapy. Nat Med. 2011;17:500-503. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1536] [Cited by in RCA: 1361] [Article Influence: 97.2] [Reference Citation Analysis (0)] |
| 110. | Moffitt RA, Marayati R, Flate EL, Volmar KE, Loeza SG, Hoadley KA, Rashid NU, Williams LA, Eaton SC, Chung AH. Virtual microdissection identifies distinct tumor- and stroma-specific subtypes of pancreatic ductal adenocarcinoma. Nat Genet. 2015;47:1168-1178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1041] [Cited by in RCA: 1477] [Article Influence: 147.7] [Reference Citation Analysis (0)] |
| 111. | Bailey P, Chang DK, Nones K, Johns AL, Patch AM, Gingras MC, Miller DK, Christ AN, Bruxner TJ, Quinn MC. Genomic analyses identify molecular subtypes of pancreatic cancer. Nature. 2016;531:47-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2848] [Cited by in RCA: 2551] [Article Influence: 283.4] [Reference Citation Analysis (0)] |
| 112. | Waddell N, Pajic M, Patch AM, Chang DK, Kassahn KS, Bailey P, Johns AL, Miller D, Nones K, Quek K. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature. 2015;518:495-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2130] [Cited by in RCA: 1991] [Article Influence: 199.1] [Reference Citation Analysis (1)] |
| 113. | Chen DS, Mellman I. Elements of cancer immunity and the cancer-immune set point. Nature. 2017;541:321-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2373] [Cited by in RCA: 3599] [Article Influence: 449.9] [Reference Citation Analysis (0)] |
| 114. | Zaretsky JM, Garcia-Diaz A, Shin DS, Escuin-Ordinas H, Hugo W, Hu-Lieskovan S, Torrejon DY, Abril-Rodriguez G, Sandoval S, Barthly L. Mutations Associated with Acquired Resistance to PD-1 Blockade in Melanoma. N Engl J Med. 2016;375:819-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2021] [Cited by in RCA: 2409] [Article Influence: 267.7] [Reference Citation Analysis (0)] |
| 115. | Sivan A, Corrales L, Hubert N, Williams JB, Aquino-Michaels K, Earley ZM, Benyamin FW, Lei YM, Jabri B, Alegre ML. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti-PD-L1 efficacy. Science. 2015;350:1084-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1979] [Cited by in RCA: 2835] [Article Influence: 283.5] [Reference Citation Analysis (1)] |
| 116. | Vétizou M, Pitt JM, Daillère R, Lepage P, Waldschmitt N, Flament C, Rusakiewicz S, Routy B, Roberti MP, Duong CP. Anticancer immunotherapy by CTLA-4 blockade relies on the gut microbiota. Science. 2015;350:1079-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1834] [Cited by in RCA: 2542] [Article Influence: 254.2] [Reference Citation Analysis (0)] |
| 117. | Patel SJ, Sanjana NE, Kishton RJ, Eidizadeh A, Vodnala SK, Cam M, Gartner JJ, Jia L, Steinberg SM, Yamamoto TN. Identification of essential genes for cancer immunotherapy. Nature. 2017;548:537-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 519] [Cited by in RCA: 639] [Article Influence: 79.9] [Reference Citation Analysis (0)] |
| 118. | Jaffee EM, Hruban RH, Biedrzycki B, Laheru D, Schepers K, Sauter PR, Goemann M, Coleman J, Grochow L, Donehower RC. Novel allogeneic granulocyte-macrophage colony-stimulating factor-secreting tumor vaccine for pancreatic cancer: a phase I trial of safety and immune activation. J Clin Oncol. 2001;19:145-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 438] [Cited by in RCA: 425] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 119. | Lutz E, Yeo CJ, Lillemoe KD, Biedrzycki B, Kobrin B, Herman J, Sugar E, Piantadosi S, Cameron JL, Solt S. A lethally irradiated allogeneic granulocyte-macrophage colony stimulating factor-secreting tumor vaccine for pancreatic adenocarcinoma. A Phase II trial of safety, efficacy, and immune activation. Ann Surg. 2011;253:328-335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 318] [Cited by in RCA: 297] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 120. | Laheru D, Lutz E, Burke J, Biedrzycki B, Solt S, Onners B, Tartakovsky I, Nemunaitis J, Le D, Sugar E. Allogeneic granulocyte macrophage colony-stimulating factor-secreting tumor immunotherapy alone or in sequence with cyclophosphamide for metastatic pancreatic cancer: a pilot study of safety, feasibility, and immune activation. Clin Cancer Res. 2008;14:1455-1463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 285] [Cited by in RCA: 268] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 121. | Le DT, Brockstedt DG, Nir-Paz R, Hampl J, Mathur S, Nemunaitis J, Sterman DH, Hassan R, Lutz E, Moyer B. A live-attenuated Listeria vaccine (ANZ-100) and a live-attenuated Listeria vaccine expressing mesothelin (CRS-207) for advanced cancers: phase I studies of safety and immune induction. Clin Cancer Res. 2012;18:858-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 273] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 122. | Hardacre JM, Mulcahy M, Small W, Talamonti M, Obel J, Krishnamurthi S, Rocha-Lima CS, Safran H, Lenz HJ, Chiorean EG. Addition of algenpantucel-L immunotherapy to standard adjuvant therapy for pancreatic cancer: a phase 2 study. J Gastrointest Surg. 2013;17:94-100; discussion p. 100-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 144] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 123. | Gjertsen MK, Bakka A, Breivik J, Saeterdal I, Gedde-Dahl T 3rd, Stokke KT, Sølheim BG, Egge TS, Søreide O, Thorsby E, Gaudernack G. Ex vivo ras peptide vaccination in patients with advanced pancreatic cancer: results of a phase I/II study. Int J Cancer. 1996;65:450-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 124. | Gjertsen MK, Buanes T, Rosseland AR, Bakka A, Gladhaug I, Søreide O, Eriksen JA, Møller M, Baksaas I, Lothe RA. Intradermal ras peptide vaccination with granulocyte-macrophage colony-stimulating factor as adjuvant: Clinical and immunological responses in patients with pancreatic adenocarcinoma. Int J Cancer. 2001;92:441-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 197] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 125. | Abou-Alfa GK, Chapman PB, Feilchenfeldt J, Brennan MF, Capanu M, Gansukh B, Jacobs G, Levin A, Neville D, Kelsen DP. Targeting mutated K-ras in pancreatic adenocarcinoma using an adjuvant vaccine. Am J Clin Oncol. 2011;34:321-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 126. | Middleton G, Silcocks P, Cox T, Valle J, Wadsley J, Propper D, Coxon F, Ross P, Madhusudan S, Roques T. Gemcitabine and capecitabine with or without telomerase peptide vaccine GV1001 in patients with locally advanced or metastatic pancreatic cancer (TeloVac): an open-label, randomised, phase 3 trial. Lancet Oncol. 2014;15:829-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 282] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 127. | Hecht JR, Bedford R, Abbruzzese JL, Lahoti S, Reid TR, Soetikno RM, Kirn DH, Freeman SM. A phase I/II trial of intratumoral endoscopic ultrasound injection of ONYX-015 with intravenous gemcitabine in unresectable pancreatic carcinoma. Clin Cancer Res. 2003;9:555-561. [PubMed] |
| 128. | Mulvihill S, Warren R, Venook A, Adler A, Randlev B, Heise C, Kirn D. Safety and feasibility of injection with an E1B-55 kDa gene-deleted, replication-selective adenovirus (ONYX-015) into primary carcinomas of the pancreas: a phase I trial. Gene Ther. 2001;8:308-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 199] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 129. | Oettle H, Seufferlein T, Luger T, Schmid RM, von Wichert G, Endlicher E, Garbe C, Kaehler KK, Enk A, Schneider A. Final results of a phase I/II study in patients with pancreatic cancer, malignant melanoma, and colorectal carcinoma with trabedersen. J Clin Oncol. 2012;30:4034-4034. [RCA] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 130. | Melisi D, Garcia-Carbonero R, Macarulla T, Pezet D, Deplanque G, Fuchs M, Trojan J, Oettle H, Kozloff M, Cleverly A. A phase II, double-blind study of galunisertib+gemcitabine (GG) vs gemcitabine+placebo (GP) in patients (pts) with unresectable pancreatic cancer (PC). J Clin Oncol. 2016;34:4019-4019. [RCA] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |