Published online Apr 21, 2017. doi: 10.3748/wjg.v23.i15.2811
Peer-review started: September 23, 2016
First decision: December 2, 2016
Revised: December 14, 2016
Accepted: January 17, 2017
Article in press: January 17, 2017
Published online: April 21, 2017
Processing time: 209 Days and 17.3 Hours
Transjugular intrahepatic portosystemic shunt (TIPS) placement is a standard procedure for the treatment of portal hypertension complications. When this conventional approach is not feasible, alternative procedures for systemic diversion of portal blood have been proposed. A one-step interventional approach, combining minilaparotomy-assisted transmesenteric (MAT) antegrade portal recanalization and TIPS, is described in an adolescent with recurrent esophageal varice bleeding and portal cavernoma (PC). A 16-year-old girl was admitted to our Unit because of repeated bleeding episodes over a short period of time due to esophageal varices in the context of a PC. A portal vein recanalization through an ileocolic vein isolation with the MAT approach followed by TIPS during the same session was performed. In the case of failed portal recanalization, this approach, would also be useful for varice endovascular embolization. Postoperative recovery was uneventful. Treatment consisting of propanolol, enoxaparin and a proton pump inhibitor was prescribed after the procedure. One month post-op, contrast enhanced computed tomography confirmed the patency of the portal and intrahepatic stent grafts. No residual peritoneal fluid was detected nor opacification of the large varices. Endoscopy showed good improvement of the varices. Doppler ultrasound confirmed the accelerated flow in the portal stent and hepatopetal flow inside the intrahepatic portal branches. Three months post-op, TIPS maintained its hourglass shape despite a slight expansion. Portal hypertension and life threatening conditions related to PC would benefit from one-step portal recanalization. MAT-TIPS is feasible and safe for the treatment of PC even in children. This minimally invasive procedure avoids or delays surgical treatment or re-transplantation when necessary in pediatric patients.
Core tip: We present the first successful hybrid intervention used to treat a portal cavernoma causing recurrent bleeding in a young girl: one step minilaparotomy-assisted transmesenteric anterograde portal recanalization and transjugular intrahepatic portosystemic shunt (TIPS). The combined approach allows direct varices embolization, restores hepatopetal portal flow, in turn preserving the portal stent graft patency by means of the TIPS placement. It is a minimally invasive procedure that can be utilized to avoid or delay surgical treatment or transplantation.
- Citation: Pelizzo G, Quaretti P, Moramarco LP, Corti R, Maestri M, Iacob G, Calcaterra V. One step minilaparotomy-assisted transmesenteric portal vein recanalization combined with transjugular intrahepatic portosystemic shunt placement: A novel surgical proposal in pediatrics. World J Gastroenterol 2017; 23(15): 2811-2818
- URL: https://www.wjgnet.com/1007-9327/full/v23/i15/2811.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i15.2811
Portal cavernoma (PC) is a critical condition with a risk of variceal hemorrhage in pediatric patients. Approximately 80% of patients with PC, present with at least one episode of upper gastrointestinal bleeding[1]. Cavernous transformation of the portal vein consists in the development of a network of tortuous collateral vessels that bypass the obstructed area due to chronic portal vein thrombosis (PVT) events. Slow blood flow through this tortuous network of veins, redistribution of blood, and new thromboses all contribute to increased portal vein pressure[2-4]. In the majority of affected patients, portal hypertension may develop with esophagogastric varices, splenomegaly and even biliary abnormalities. Given the complexity and rarity of PC, different surgical techniques, such as various portosystemic shunts and gastrosplenic decompression, have been proposed to prevent and treat variceal hemorrhage, thrombosis recurrence and symptoms related to portal biliopathy[5,6].
Minilaparotomy-assisted transmesenteric (MAT) alone for antegrade portal recanalization[7] or combined with transjugular or transfemoral intrahepatic portosystemic shunt placement has been described as a useful technique in adults with a patent portal vein[8,9]. This minimally invasive approach could be extended to include pediatric patients when the patency of the PC is difficult to manage. Here we present the case of a 16 year-old girl with multiple upper gastro-intestinal (GI) bleeding events due to oesophageal varices in the context of a PC, treated with a new hybrid approach.
A 16-year-old girl was admitted to the Pediatric Surgery Unit for abdominal pain and hematemesis. Her clinical history was normal until three months before, when she started experiencing GI bleeding. The girl was diagnosed in her home country as having esophageal varices and PVT in the context of a PC. There was no familial or personal history of coagulation disorders, nor was the patient cirrhotic. The only risk factor for PC, was an umbilical catheterization at birth following a pre-term emergency cesarean delivery. A first sclerotherapy treatment was done two months before the admission to our Institution and the patient was treated with propanolol.
Clinical evaluation of the patient showed normal cardiovascular parameters, blood values were as follows: (Hb 11.1 g/dL), no signs of hepatitis (negative serology for viral hepatitis) or liver abnormalities (GOT 22 mU/mL, GPT 26 mU/mL, GGT 14 mU/mL); ammonium was normal, (49 μg/dL); no signs of cholangitis were recorded (WBC 7.7 × 103/μL, PCR 0.57 mg/dL, alkaline phosphatase 57 mU/mL, total bilirubin 1.93 mg/dL, direct bilirubin 0.59 mg/dL). The abdominal ultrasound examination confirmed the presence of a PC, an enlarged spleen (14 cm longitudinal diameter) and no ascites. The angio CT-scan evaluation confirmed the presence of a PC involving the main portal trunk, extending 3 cm. (Figure 1), sparing the spleno-mesenteric confluence. Splenic and mesenteric venous flow were maintained through the enlarged hepatofugal left gastric vessel. The upper gastrointestinal endoscopy evidenced multiple third degree varices with bleeding cherry red spots requiring immediate treatment with endoscopical ligature.
One month later, massive upper gastrointestinal bleeding re-occurred and her hemoglobin level decreased from 12.4 to 8.4 g/dL. Considering the patient’s history and the number of bleeding episodes over a short period of time, the indication for a portosystemic shunt was discussed. The multidisciplinary team, including pediatric surgeons, interventional radiologists, and pediatric gastroenterologists agreed upon the choice to perform a portal vein recanalization through ileocolic vein isolation with a MAT approach, followed by transjugular intrahepatic portosystemic shunt (TIPS) during the same session. In the case of failed portal recanalization, this approach, would also be useful for varice endovascular embolization and serve as a bridge for a delayed mesorex procedure[10]. Prior to the intervention, and after being informed on the nature of the intervention, the patient’s parents gave written consent to endovascularly treat the PC by inserting a portal stent followed by TIPS to stop the variceal bleeding and readdress the portal flow to the liver.
Under general anesthesia, the right neck and the entire abdomen were sterilely prepared for both minilaparotomy and jugular access. A transverse minilaparotomy of the right lower abdomen and isolation of the ileocolic vein were facilitated by the insertion of a 6 Fr sheath to access the superior mesenteric vein.
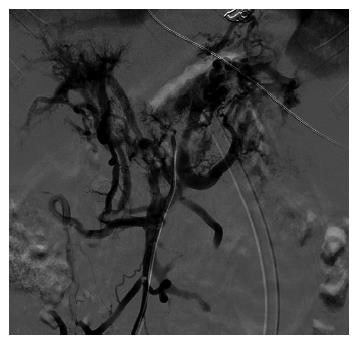
Venography of the patent superior mesenteric vein with 16 mL (Visipaque 270 mgI/dL, GE, United States) nonionic contrast medium (CM) diluted with saline, confirmed the occlusion of the main trunk of the portal vein with intrahepatic portal branches (lately opacified through tiny collateral vessels), the patency of the splenic vein and an abnormal varicose gastric trunk (Figure 2).
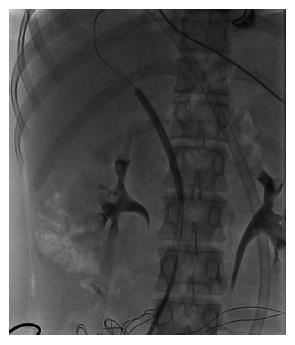
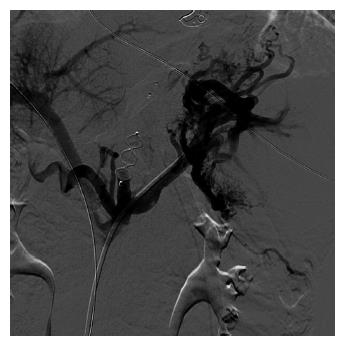
Through a 5Fr angled catheter (Van Schie, Cook, Bloomington, United States) a 0.035’ hydrophilic guide wire (Terumo, Tokyo, Japan) was gently advanced across the PC until an intrahepatic portal branch was reached. Then the hydrophilic guide wire was replaced with a 0.018’ guide wire (V18, Boston Sc, United States). With the distal tip in the right portal branch, multiple dilations (6 and 8 mm in width) of the occluded portal trunk were made (Figure 3). Due to the competitive high hepatofugal flow in the gastric varices, catheterization of the varicose trunk with a 6 Fr guiding catheter was performed. Two Amplatzer plugs (S.Jude, Type III, 6 mm and 10 mm) were released under fluororscopy in the proximal part of the large varicose vein. Venography revealed the occlusion of the hepatofugal flow (Figure 4).
At this point, we proceeded with the right transjugular approach for the insertion of the intrahepatic portosystemic shunt. Once the right hepatic vein was catheterized, entry into the right portal branch was facilitated by antegrade CM flushing through the trans-mesenteric catheter introducer. After positioning a guide wire into the splenic vein, portography with a pigtail catheter was performed. After pre-dilation of the intrahepatic tract with a 6mm balloon, the patient suddenly became hypotensive. Portography revealed a minor extrahepatic leakage of the CM near the hilum (probably due to an extrahepatic puncture of the portal bifurcation).
A Viatorr stent graft (10 mm × 70 mm, Gore, Flagstaff, AZ) was promptly released into the portal vein, with the leading two centimeters of open mesh at the splenomesenteric confluence. Subsequently, a second Viatorr stent graft (10 mm × 80 mm, Gore, Flagstaff, AZ) was inserted to bridge the portal vein with the inferior vena cava. The leading portion of the open mesh was left partially overlapping with the first stent graft, paying attention to preserve the portal branch outflow. Therefore, the portal stent graft was entirely dilated to 9 mm as well as the distal overlapping portion of the transhepatic stent. The intraparenchymal tract of the liver stent graft was dilated to 6 mm, yielding an hourglass-like shape, in order to avoid shunt overflow[11]. Following stabilization of the patient’s hemodynamic values, the angiography confirmed that the portal perihilar leak had been repaired.
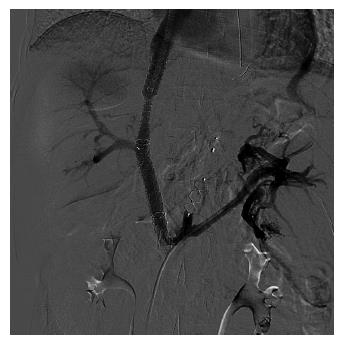
A follow-up angiography showed rapid hepatopetal flow to the right atrium through the TIPS with preserved patency of the portal branches and no residual hepatofugal filling of the gastric varices (Figure 5). The portosystemic pressure gradient was reduced postoperatively from 22 to 12 mmHg.
After the procedure, fluoroscopy revealed a perihepatic fluid layer. The patient was hemodynamically stable. Through the minilaparotomy the peridiaphragmatic fluid was carefully cleaned. Abdominal suturing, measuring 3 cm in length, was performed with 3.0Vicryl running stitches.
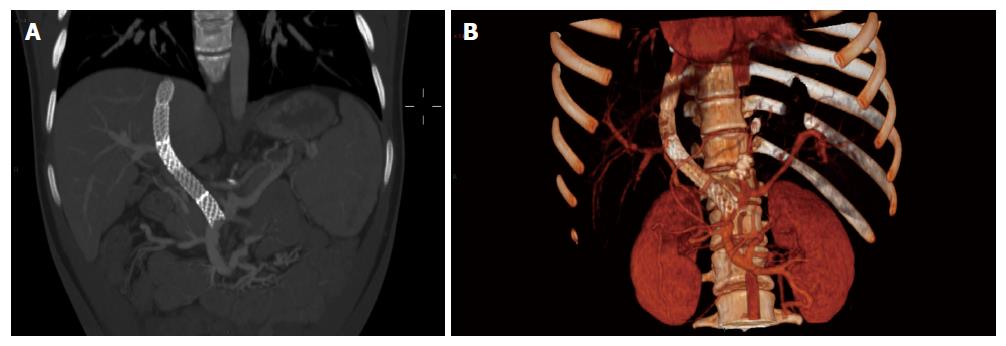
Postoperative recovery was uneventful. No blood transfusion was necessary. No encephalopathy episodes were observed. The girl was discharged 15 d after the surgery. Therapy consisting of propranolol and a proton pump inhibitor was prescribed for three consecutive months after the procedure. One month later, a contrast enhanced CT confirmed the patency of the portal and intrahepatic stent grafts. No residual peritoneal fluid was detected nor opacification of the large varices. The TIPS maintained its hourglass shape despite a slight expansion Figure 6A and B). The serum ammonia level was 55 μmol/L. The upper gastrointestinal endoscopy showed good improvement of the varices, reclassified as second degree with no cherry red spots. Doppler ultrasound confirmed the accelerated flow through the portal stent with a peak systolic velocity of 34 cm/s and hepatopetal flow inside the intrahepatic portal branches.
We present the first successful treatment of PC causing recurrent gastro-esophageal varice bleeding in a young girl with a novel hybrid approach: MAT antegrade portal recanalization combined with TIPS in a single session.
Esophageal varices are the most frequent cause of upper gastrointestinal bleeding in portal hypertension. PC is a common cause of secondary portal hypertension and bleeding in non cirrhotic children[12,13] and it is characterized by an extended network of small and extremely sinuous vessels in the hilum which compensate for the impaired hepatopetal flow, resulting from a PVT event. The causes of PVT in non cirrhotic patients can be divided into four different groups: direct injury to the portal vein and consequent thrombus formation and obstruction, as occurs in omphalitis or in umbilical catheterization; congenital malformation of the portal system associated with other cardiovascular disorders; coagulation disorders; and idiopathic PVT.
PVT clinical presentation is different in the context of acute or chronic onset and depends on the development and extent of the collateral circulation. Intestinal congestion and ischemia, with abdominal pain, diarrhea, rectal bleeding, abdominal distention, nausea, vomiting, anorexia, fever, lactacidosis sepsis, and splenomegaly are common features of acute PVT. In contrast, chronic PVT can be completely asymptomatic or characterized by splenomegaly, pancytopenia, varices, and rarely, ascites[5]. The abdominal ultrasound with Doppler/power-Doppler examination is the investigation of choice in PVT diagnosis, with a sensitivity and specificity ranging between 60% and 100%[14]. It can reveal the presence of solid, hyperechoic material in a distended portal vein or its tributaries, the presence of collateral vessels or a cavernoma. Doppler imaging can confirm the absence of flow in part or all of the vessel lumen; and, if present, a cavernomatous transformation[15-17]. Multiphase CT, identifying characteristic changes involving the portal trunk, can confirm the diagnosis, by demonstrating numerous vascular structures in the region of the portal vein, which are enhanced during the portal venous phase, and not during the arterial phase. MRI is also a proven method for imaging the portal venous system and may be used as a complementary or alternative modality to CT.
Although spontaneous resolution of PVT has been reported in the literature, specific therapeutic management is mandatory to resolve portal vein obstruction and avoid serious complications[18,19]. The correction of causal factors, prevention of thrombosis extension and achievement of portal vein patency are considered the goals of PVT treatment. However, in case of long standing thrombosis, the management of complications related to the appearance of portal hypertension should be considered[20].
In adult patients, TIPS placement is considered the standard procedure for treatment of portal hypertension[21] unresponsive to medical and endoscopic treatment. PC was initially considered a contraindication to TIPS placement. Recently, this procedure has been revisited and is now considered feasible in selected patients with portal thrombosis[22,23]. When the conventional transjugular hepatic vein to portal vein approach is not feasible[8,9,24,25], alternative radiological approaches as well as transhepatic, transplenic and trans-mesenteric have been described. Surgical portosystemic shunt placement for systemic diversion of portal blood has been reported[26].
PVT is also a complication that may occur after liver transplantation in adults and children. To improve graft survival and avoid patient compromise, a combined technique for PV recanalization, in cases of PV obstruction after liver transplantation has been described. PV recanalization is promoted through a combined approach (transhepatic and minilaparotomy) with the aim of re-establishing portal flow, which can be followed postoperatively with Doppler US evaluation. The transhepatic retrograde access in combination with a minilaparotomy is an option when percutaneous recanalization is unsuccessful, as in the case of extensive portomesenteric thrombosis[27,28].
The TIPS-MAT combination is described in the literature, using a combination of transjugular or transfemoral access to the hepatic vein combined with transmesenteric access to the patent portal system with a minilaparotomy[8,9]. This combination is considered a reasonable alternative to the conventional technique, particularly in patients in whom a conventional approach is technically challenging[29]. MAT portal recanalization has been described by Matsui et al[7]. They performed a trans-mesenteric recanalization of a thrombosed main portal trunk followed by a portal stenting in a patient with alcoholic cirrhosis. Five days post-op, a portal thrombosis abruptly occurred. The authors were obliged to recanalize the portal system from a transjugular route targeting with the needle the bare metal stent placed in the right portal branch. Finally TIPS was performed[7].
A retrospective review of all adult patients who have undergone a MAT compared with the conventional TIPS procedure over a 6-year period showed similar shunt primary patency and technical success rates; the MAT approach, more frequently adopted in patients referred for refractory ascites, was associated with a significantly higher rate of minilaparotomy-related wound or infectious complications[29].
In children, portosystemic shunt procedures typically lead to a decrease in portal flow over time and may impair the structure and function of the liver; which in turn may result in long-term complications such as hepatic encephalopathy (due to hyperammonemia) or hepato-pulmonary syndrome. For this reason, selective shunts, as opposed to central portosystemic shunts, have become preferable for treating portal hypertension in the pediatric age[30-32]. The Meso-Rex shunt procedure, first described in 1992 by de Ville de Goyet et al[33] for the treatment of extrahepatic portal vein obstruction in pediatric liver transplant patients, provides more physiological relief of portal hypertension compared with porto-systemic shunts.
The one-step TIPS-MAT technique has never been described in the pediatric population nor in non cirrhotic patients with portal hypertension or PC[34]. In our young patient with PC, the MAT recanalization of the cavernoma associated with MAT varices embolization was followed in the same session by TIPS placement. Simultaneous TIPS placement reduces early portal stent thrombosis risk[7], and is indicated in subjects with coagulation disorders; where it decreases peripheral resistance and increases blood flow velocity in the portal system thereby permitting easy access to the portal vein for any further treatment. For instance, calibration of the TIPS diameter during the patient’s lifetime could become a therapeutic option that could be applied for encephalopathy. Furthermore, a dedicated ePTFE stent graft such as Viatorr (Gore, Flagstaff, United States) ensures superior patency. This device requires advancement of a 10 Fr sheath through the target vessel and its release. It seems likely to be risky performing a portal stenting alone by transmesenteric approach with Viatorr.
In case of PV obstruction in the pediatric age, this combined approach could preserve portal flow and avoid impairment of liver function related to portosystemic shunt placement. MAT portal recanalization associated with direct varices embolization and TIPS may be considered a feasible and safe treatment for PC reducing portal hypertension and life-threating relapsing bleeding ss. It is a minimally invasive procedure and can be used to avoid or delay surgical treatment, or transplantation.
Consequently, recent experience and technical improvements encourage the application of this technique in the management of pediatric patients with non cirrhotic portal hypertension. The use of this procedure in conjunction with other strategies and techniques might be of interest for a multidisciplinary team, particularly those caring for children, in order to expand the indications for this procedure before resorting to surgery.
The authors thank Dr. L. Kelly for English revision of the manuscript.
A 16-year-old girl was admitted to our Unit with recurrent bleeding episodes over a short period of time due to esophageal varices and portal hypertension in the context of a portal cavernoma (PC).
Recurrent massive upper gastrointestinal bleeding due to esophageal varices.
Portal hypertension in non-cirrhotic patients may result from direct injury to the portal vein and consequent thrombus formation and obstruction; congenital malformation of the portal system associated with other cardiovascular disorders, schistosomiasis, coagulation disorders, or idiopathic portal vein thrombosis (PVT).
Hemoglobin level decrease from 12.4 to 8.4 g/dL, no signs of hepatitis or liver abnormalities or cholangitis, normal ammonium level, normal coagulation parameters, no thrombophilic gene mutations.
Angio CT-scan evaluation confirming the presence of a PC involving the main portal trunk, extending 3 cm, sparing the spleno-mesenteric confluence. Splenic and mesenteric venous flow were maintained through the enlarged hepatofugal left gastric vein. Upper gastrointestinal endoscopy evidenced multiple third degree varices with bleeding cherry red spots.
PC involving the main portal trunk causing huge varices.
Minilaparotomy-assisted transmesenteric (MAT) portal vein antegrade recanalization and direct varices embolization combined in the same session with transjugular intrahepatic portosystemic shunt placement (TIPS).
The one-step TIPS-MAT technique and direct varices embolization has never been described in the pediatric population nor in non-cirrhotic patients with portal hypertension or PC.
MAT recanalization of the cavernoma associated with MAT varices embolization was followed in the same session by TIPS placement. Simultaneous TIPS placement reduces early and late portal stent thrombosis risk; where it decreases peripheral resistance and increases blood flow velocity in the portal system thereby permitting easy access to the portal vein for any further treatment.
The combined approach allows direct varices embolization, restores the hepatopetal portal flow, in turn preserving the portal stent graft by means of the TIPS placement. It is a minimally invasive procedure that can be utilized to avoid or delay surgical treatment or transplantation.
The MAT + TIPS (one step) is a relevant procedure, which is a therapeutic option in patients with PVT.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Backes AN S- Editor: Yu J L- Editor: A E- Editor: Zhang FF
| 1. | Zhang MM, Pu CL, Li YC, Guo CB. Sixty-four-slice computed tomography in surgical strategy of portal vein cavernous transformation. World J Gastroenterol. 2011;17:4334-4338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (2)] |
| 2. | De Gaetano AM, Lafortune M, Patriquin H, De Franco A, Aubin B, Paradis K. Cavernous transformation of the portal vein: patterns of intrahepatic and splanchnic collateral circulation detected with Doppler sonography. AJR Am J Roentgenol. 1995;165:1151-1155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 146] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 3. | Bambini DA, Superina R, Almond PS, Whitington PF, Alonso E. Experience with the Rex shunt (mesenterico-left portal bypass) in children with extrahepatic portal hypertension. J Pediatr Surg. 2000;35:13-18; discussion 18-19. [PubMed] |
| 4. | Gu S, Chang S, Chu J, Xu M, Yan Z, Liu DC, Chen Q. Spleno-adrenal shunt: a novel alternative for portosystemic decompression in children with portal vein cavernous transformation. J Pediatr Surg. 2012;47:2189-2193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Wang J, Tian XG, Li Y, Zhang CQ, Liu FL, Cui Y, Liu JY. Comparison of modified percutaneous transhepatic variceal embolization and endoscopic cyanoacrylate injection for gastric variceal rebleeding. World J Gastroenterol. 2013;19:706-714. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Amitrano L, Guardascione MA, Manguso F, Bennato R, Bove A, DeNucci C, Lombardi G, Martino R, Menchise A, Orsini L. The effectiveness of current acute variceal bleed treatments in unselected cirrhotic patients: refining short-term prognosis and risk factors. Am J Gastroenterol. 2012;107:1872-1878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 133] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 7. | Matsui O, Yoshikawa J, Kadoya M, Gabata T, Takashima T, Urabe T, Unoura M, Kobayashi K. Transjugular intrahepatic portosystemic shunt after previous recanalization of a chronically thrombosed portal vein via a transmesenteric approach. Cardiovasc Intervent Radiol. 1996;19:352-355. [PubMed] |
| 8. | Rozenblit G, DelGuercio LR, Savino JA, Rundback JH, Cerabona TD, Policastro AJ, Artuso DP. Transmesenteric-transfemoral method of intrahepatic portosystemic shunt placement with minilaparotomy. J Vasc Interv Radiol. 1996;7:499-506. [PubMed] |
| 9. | Rozenblit G, Del Guercio LR. Combined transmesenteric and transjugular approach for intrahepatic portosystemic shunt placement. J Vasc Interv Radiol. 1993;4:661-666. [PubMed] |
| 10. | Durham JD, Kumpe DA, Van Stiegmann G, Goff JS, Subber SW, Rothbarth LJ. Direct catheterization of the mesenteric vein: combined surgical and radiologic approach to the treatment of variceal hemorrhage. Radiology. 1990;177:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Holster IL, Tjwa ET, Moelker A, Wils A, Hansen BE, Vermeijden JR, Scholten P, van Hoek B, Nicolai JJ, Kuipers EJ. Covered transjugular intrahepatic portosystemic shunt versus endoscopic therapy + β-blocker for prevention of variceal rebleeding. Hepatology. 2016;63:581-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 164] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 12. | Shah OJ, Shah P, Robbani I, Mir F, Nazir P. An 18-year-old female with recurrent esophageal variceal bleeding. Ann Saudi Med. 2009;29:61. [PubMed] |
| 13. | Qi X, Han G, Yin Z, He C, Wang J, Guo W, Niu J, Zhang W, Bai M, Fan D. Transjugular intrahepatic portosystemic shunt for portal cavernoma with symptomatic portal hypertension in non-cirrhotic patients. Dig Dis Sci. 2012;57:1072-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 14. | Chawla Y, Duseja A, Dhiman RK. Review article: the modern management of portal vein thrombosis. Aliment Pharmacol Ther. 2009;30:881-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 103] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 15. | Denninger MH, Chaït Y, Casadevall N, Hillaire S, Guillin MC, Bezeaud A, Erlinger S, Briere J, Valla D. Cause of portal or hepatic venous thrombosis in adults: the role of multiple concurrent factors. Hepatology. 2000;31:587-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 466] [Cited by in RCA: 450] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 16. | Kocher G, Himmelmann A. Portal vein thrombosis (PVT): a study of 20 non-cirrhotic cases. Swiss Med Wkly. 2005;135:372-376. [PubMed] |
| 17. | Belli L, Puttini M, Marni A. Extrahepatic portal obstruction: Clinical experience and surgical treatment in 105 patients. J Cardiovasc Surg (Torino). 1980;21:439-448. [PubMed] |
| 18. | Condat B, Pessione F, Helene Denninger M, Hillaire S, Valla D. Recent portal or mesenteric venous thrombosis: increased recognition and frequent recanalization on anticoagulant therapy. Hepatology. 2000;32:466-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 342] [Cited by in RCA: 330] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 19. | Baril N, Wren S, Radin R, Ralls P, Stain S. The role of anticoagulation in pylephlebitis. Am J Surg. 1996;172:449-452; discussion 452-453. [PubMed] |
| 20. | DeLeve LD, Valla DC, Garcia-Tsao G. Vascular disorders of the liver. Hepatology. 2009;49:1729-1764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 739] [Cited by in RCA: 650] [Article Influence: 40.6] [Reference Citation Analysis (0)] |
| 21. | Fidelman N, Kwan SW, LaBerge JM, Gordon RL, Ring EJ, Kerlan RK. The transjugular intrahepatic portosystemic shunt: an update. AJR Am J Roentgenol. 2012;199:746-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 119] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 22. | Senzolo M, Burra P, Cholongitas E, Lodato F, Marelli L, Manousou P, Patch D, Sturniolo GC, Burroughs AK. The transjugular route: the key hole to the liver world. Dig Liver Dis. 2007;39:105-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Senzolo M, Tibbals J, Cholongitas E, Triantos CK, Burroughs AK, Patch D. Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with and without cavernous transformation. Aliment Pharmacol Ther. 2006;23:767-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 178] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 24. | LaBerge JM, Ring EJ, Gordon RL. Percutaneous intrahepatic portosystemic shunt created via a femoral vein approach. Radiology. 1991;181:679-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Fitsiori K, Tsitskari M, Kelekis A, Filippiadis D, Triantafyllou K, Brountzos E. Transjugular intrahepatic portosystemic shunt for the treatment of Budd-Chiari syndrome patients: results from a single center. Cardiovasc Intervent Radiol. 2014;37:691-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 26. | Gur I, Diggs BS, Orloff SL. Surgical portosystemic shunts in the era of TIPS and liver transplantation are still relevant. HPB (Oxford). 2014;16:481-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Carnevale FC, Szejnfeld D, Moreira AM, Gibelli N, De Gregório MA, Tannuri U, Cerri GG. Long-term follow-up after successful transjugular intrahepatic portosystemic shunt placement in a pediatric patient with Budd-Chiari syndrome. Cardiovasc Intervent Radiol. 2008;31:1244-1248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Carnevale FC, Santos AC, Seda-Neto J, Zurstrassen CE, Moreira AM, Carone E, Marcelino AS, Porta G, Pugliese R, Miura I. Portal vein obstruction after liver transplantation in children treated by simultaneous minilaparotomy and transhepatic approaches: initial experience. Pediatr Transplant. 2011;15:47-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Jalaeian H, Talaie R, D’Souza D, Taleb S, Noorbaloochi S, Flanagan S, Hunter D, Golzarian J. Minilaparotomy-Assisted Transmesenteric-Transjugular Intrahepatic Portosystemic Shunt: Comparison with Conventional Transjugular Approach. Cardiovasc Intervent Radiol. 2016;39:1413-1419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | de Ville de Goyet J, Gibbs P, Clapuyt P, Reding R, Sokal EM, Otte JB. Original extrahilar approach for hepatic portal revascularization and relief of extrahepatic portal hypertension related to later portal vein thrombosis after pediatric liver transplantation. Long term results. Transplantation. 1996;62:71-75. [PubMed] |
| 31. | de Ville de Goyet J, Martinet JP, Lacrosse M, Goffette P, Melange M, Lerut J. Mesenterico-left intrahepatic portal vein shunt: original technique to treat symptomatic extrahepatic portal hypertension. Acta Gastroenterol Belg. 1998;61:13-16. [PubMed] |
| 32. | Mitchell A, Mirza D, de Ville de Goyet J, Buckels J. Absence of the left portal vein: a difficulty for reduction of liver grafts? Transplantation. 2000;69:1731-1732. [PubMed] |
| 33. | de Ville de Goyet J, Clapuyt P, Otte JB. Extrahilar mesenterico-left portal shunt to relieve extrahepatic portal hypertension after partial liver transplant. Transplantation. 1992;53:231-232. [PubMed] |
| 34. | Di Giorgio A, Agazzi R, Alberti D, Colledan M, D’Antiga L. Feasibility and efficacy of transjugular intrahepatic portosystemic shunt (TIPS) in children. J Pediatr Gastroenterol Nutr. 2012;54:594-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |