Published online Jul 7, 2016. doi: 10.3748/wjg.v22.i25.5780
Peer-review started: March 15, 2016
First decision: March 31, 2016
Revised: April 21, 2016
Accepted: May 4, 2016
Article in press: May 4, 2016
Published online: July 7, 2016
AIM: To evaluate and validate the national trends and predictors of in-patient mortality of transjugular intrahepatic portosystemic shunt (TIPS) in 15 years.
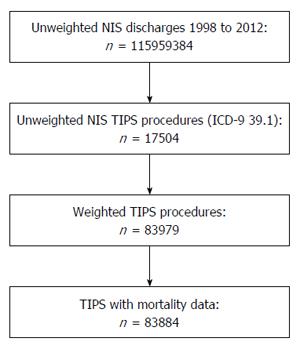
METHODS: Using the National Inpatient Sample which is a part of Health Cost and Utilization Project, we identified a discharge-weighted national estimate of 83884 TIPS procedures performed in the United States from 1998 to 2012 using international classification of diseases-9 procedural code 39.1. The demographic, hospital and co-morbility data were analyzed using a multivariant analysis. Using multi-nominal logistic regression analysis, we determined predictive factors related to increases in-hospital mortality. Comorbidity measures are in accordance to the Comorbidity Software designed by the Agency for Healthcare Research and Quality.
RESULTS: Overall, 12.3% of patients died during hospitalization with downward trend in-hospital mortality with the mean length of stay of 10.8 ± 13.1 d. Notable, African American patients (OR = 1.809 vs Caucasian patients, P < 0.001), transferred patients (OR = 1.347 vs non-transferred, P < 0.001), emergency admissions (OR = 3.032 vs elective cases, P < 0.001), patients in the Northeast region (OR = 1.449 vs West, P < 0.001) had significantly higher odds of in-hospital mortality. Number of diagnoses and number of procedures showed positive correlations with in-hospital death (OR = 1.249 per one increase in number of procedures). Patients diagnosed with acute respiratory failure (OR = 8.246), acute kidney failure (OR = 4.359), hepatic encephalopathy (OR = 2.217) and esophageal variceal bleeding (OR = 2.187) were at considerably higher odds of in-hospital death compared with ascites (OR = 0.136, P < 0.001). Comorbidity measures with the highest odds of in-hospital death were fluid and electrolyte disorders (OR = 2.823), coagulopathy (OR = 2.016), and lymphoma (OR = 1.842).
CONCLUSION: The overall mortality of the TIPS procedure is steadily decreasing, though the length of stay has remained relatively constant. Specific patient ethnicity, location, transfer status, primary diagnosis and comorbidities correlate with increased odds of TIPS in-hospital death.
Core tip: This is the first large-scale, national trends data investigating in-patient death following transjugular intrahepatic portosystemic shunt (TIPS) using the National Inpatient Sample database from 1998 to 2012. Over 80000 TIPS related data have been investigated. Overall in-patient mortality has been down-trending over the past 15 years. A significant decrease of mortality occurred after 2005 with an introduction of covered stent graft for TIPS which improved the patient survival and TIPS outcomes. Specific patient ethnicity, location, transfer status, primary diagnosis and comorbidities correlate with increased odds of in-hospital death after TIPS.
- Citation: Lee EW, Kuei A, Saab S, Busuttil RW, Durazo F, Han SH, El-Kabany MM, McWilliams JP, Kee ST. Nationwide trends and predictors of inpatient mortality in 83884 transjugular intrahepatic portosystemic shunt. World J Gastroenterol 2016; 22(25): 5780-5789
- URL: https://www.wjgnet.com/1007-9327/full/v22/i25/5780.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i25.5780
Transjugular intrahepatic portosystemic shunt, or TIPS, is currently the most commonly performed interventional procedure to treat complications of portal hypertension. TIPS achieves portal decompression through the placement of a stent bridging the hepatic and portal veins. The American Association for the Study of Liver Diseases indications for this procedure include refractory variceal bleeding and ascites[1]. Over 20 years of clinical experience have better defined TIPS candidacy and brought technical advancements such as polytetraflouroethylenne (PTFE) covered stents that have enhanced long term clinical outcomes[2]. However, TIPS remains a procedure full of clinical challenges. Patients are expected to be monitored overnight following the procedure for a number of complications including hemorrhage from extra-capsular puncture, hepatic encephalopathy, injury to the bile duct, or hepatic artery and portal vein, shunt stenosis/thrombosis/occlusion, congestive heart failure, acute pulmonary edema and death[3].
Factors affecting patient survival following TIPS have been extensively studied in the past. Detailed patient markers proposed including Model for End-stage Liver Disease (MELD) scoring, Child-Pugh scoring, serum bilirubin, and serum creatinine have found use in daily clinical practice[4-8]. However, the majority of these studies are of (1) a limited sample size; (2) outside of directly measurable patient factors; and (3) lacking broad-spectrum analysis. No contemporary nationwide analysis of patient demographic, hospital, and diagnostic data to in-patient mortality has been performed. Utilizing data from the National Inpatient Sample from 1998 to 2012, we aimed to investigate national trends in incidence and TIPS mortality and shed insight on new factors possibly associated with in-patient death.
The National (Nationwide) Inpatient Sample (NIS) is a family of hospital discharge databases part of the Healthcare Cost and Utilization Project (HCUP). The NIS is the largest publically available all-payer inpatient health care database, containing unweighted data from over 7 million hospital stays each year. NIS data approximates a 20-percent stratified sample of all discharges from United States community hospitals, excluding rehabilitation and long-term acute care hospitals. The samples are designed to facilitate discharge-level weighting for producing national estimates. Used for this study are the 15-years NIS data sets from year 1998 to 2012. This study uses only deidentified patient and hospital data and meets the “Exempt” criteria by the Institutional Board Review.
To identify the study patient population, we include all discharges with TIPS performed during hospitalization (International Classification of Diseases 9 procedural code 39.1). We identified a discharge-weighted national estimate of 83884 patients who underwent TIPS from 1998 to 2012. For multivariate analysis, patient data is categorized under three profiles: demographic, hospital, and diagnostic. The demographic profile includes patient age, gender, race, primary payer, income quartile by ZIP, admission transfer status, weekend admission status, and admission type. The hospital profile includes teaching hospital status, hospital bed size, hospital region, control of hospital. Bed size as defined by the NIS depends on the region, urban-rural designation, and teaching status of the hospital. Based on these factors, bed size categories range from 1-249 for small, 25-449 for medium, and 45-450+ for large. The diagnostic profile includes total number of diagnoses, total number of chronic conditions, total number of procedures, top diagnoses, and comorbidity measures assigned using ARHQ comorbidity software (available beginning in 2002). Proportions or mean ± SD were calculated for all studied parameters. General outcomes reported included percentile of in-hospital mortality and mean length of stay ± SD. These outcomes were further categorized as “before 2005” or “after 2005” to investigate the effects of the commercial availability of PTFE-covered stents (GORE® VIATORR® TIPS Endoprosthesis, W. L. Gore & Associates Inc, Flagstaff, Arizona, United States) around 2003-2004[9]. Appropriate Z and t tests were utilized for comparison analysis. The primary outcome measure to be evaluated through multivariate analysis was in-hospital mortality. Using multi-nominal logistic regression, we identified the most significant profile factors related to increases in in-patient mortality within the demographic, hospital, and diagnostic categories. Odds ratios with appropriate 95% confidence intervals and P values were calculated alongside a reference point for comparison analysis. For demographic and hospital variables, the reference point was selected among variable outcomes (such as Caucasian for race). For diagnostic variables, the reference of comparison was having no diagnosis of disease or comorbidity. Comorbidity measures are in accordance to the Comorbidity Software designed by the Agency for Healthcare Research and Quality (AHRQ) which identifies a set of comorbidities and separates them from the primary reason for hospitalization for use with large administrative datasets.
All statistical analysis was performed using SPSS version 22.0 (IBM Corporation, Armonk, New York) and Microsoft Excel 2013 (Microsoft, Redmond, WA, United States). P < 0.05 is considered statistically significant.
A 1998-2012 nationwide weighted total of 83884 TIPS cases were included for analysis. A total of 95 cases were excluded for analysis due to missing mortality data. The case selection process is summarized in Figure 1.
Table 1 summarizes the patient demographic data of all TIPS cases from 1998 to 2012. The mean (± SD) age of all cases was 54.2 (± 13.9) years, with most cases occurring in the age group 50-59 years (33.0%). The patient population was predominantly male (63.2%) and Caucasian (71.0%). There were more Hispanic than African American patients (16.1% vs 6.0%). The majority of patients paid through private insurance (36.6%), followed by Medicare (31.4%), then Medicaid (21.4%). Of the patients included in our analysis, 17.9% of patients were transferred in from an outside hospital and 17.0% were admitted on the weekend. Most patients were either emergency (46.1%) or urgent (26.8%) admissions while elective admissions constituted 26.9% of admissions. Trauma center admissions were uncommon at 0.1%, however this data is only available starting in 2003.
| Percent | χ2P value | |
| Age (yr) | < 0.001 | |
| 0-9 | 0.9% | |
| 10-19 | 1.3% | |
| 20-29 | 2.6% | |
| 30-39 | 6.3% | |
| 40-49 | 22.4% | |
| 50-59 | 33.0% | |
| 60-69 | 20.8% | |
| 70-79 | 10.4% | |
| 80-89 | 2.3% | |
| 90-99 | 0.1% | |
| Age > 70 | 11.4% | < 0.001 |
| Sex | < 0.001 | |
| Male | 63.2% | |
| Female | 36.8% | |
| Race | < 0.001 | |
| White | 71.0% | |
| Black | 6.0% | |
| Hispanic | 16.1% | |
| Asian/Pacific Islander | 2.0% | |
| Native American | 0.9% | |
| Other | 3.5% | |
| Unknown | 0.4% | |
| Primary payer | < 0.001 | |
| Medicare | 31.4% | |
| Medicaid | 21.4% | |
| Private | 36.6% | |
| Self-Pay | 5.6% | |
| Income quartile by ZIP code | < 0.001 | |
| (1) Quartile 1 | 28.3% | |
| (2) Quartile 2 | 26.9% | |
| (3) Quartile 3 | 24.5% | |
| (4) Quartile 4 | 19.4% | |
| Missing | 0.8% | |
| Transfer status | < 0.001 | |
| Transferred in from acute care hospital | 17.9% | |
| Not transfer | 79.3% | |
| Weekend admission status | < 0.001 | |
| Admitted on weekend (1) | 17.0% | |
| Not admitted on weekend (0) | 83.0% | |
| Admission type | < 0.001 | |
| Emergency | 46.1% | |
| Urgent | 26.8% | |
| Elective | 26.9% | |
| Trauma center | 0.1% | |
| Hospital type | < 0.001 | |
| Teaching hospital | 74.9% | |
| Non-Teaching hospital | 25.1% | |
| Hospital bed size | < 0.001 | |
| Small | 4.4% | |
| Medium | 18.0% | |
| Large | 77.6% | |
| Hospital region | < 0.001 | |
| Northeast | 17.8% | |
| Midwest | 22.7% | |
| South | 35.4% | |
| West | 24.2% | |
| Control of hospital | < 0.001 | |
| Private, non-profit | 32.8% | |
| Private, investor owned | 5.8% |
Table 1 also describes hospital characteristics of all admissions. Hospitals where patients had TIPS were mostly teaching (74.9%), non-profit (32.8%), and large (77.6%). The Southern region had the highest number of admissions with TIPS (35.4%).
Table 2 summarizes patient diagnostic information. The mean (± SD) number of total diagnoses was 10.4 (± 5.1). The fifteen most common diagnoses by international classification of diseases-9 were portal hypertension (43.5%), ascites (30.9%), esophageal variceal bleeding (28.9%), other ascites (18.8%), acute post-hemorrhagic anemia (18.3%), uncomplicated diabetes (17.8%), hepatic encephalopathy (17.5%), hypertension NOS (17.4%), cirrhosis of the liver NOS (16.1%), alcoholic liver cirrhosis (15.3%), thrombocytopenia NOS (15.0%), varices of other sites (13.7%), acute kidney failure NOS (13.3%), esophageal varices with no bleeding (13.1%), and acute respiratory failure (12.8%). Liver disease (84.1%), fluid and electrolyte disorders (36.8%), and coagulopathy (35.7%), were the most common AHRQ comorbidity measures in the patient population.
| Percent | χ2P value | |
| Diagnosis (ICD-9 code) | ||
| Portal hypertension (572.3) | 43.5% | < 0.001 |
| Ascites (789.5) | 30.9% | |
| Esophageal variceal bleeding (456.20) | 28.9% | |
| Other ascites (789.59) | 18.8% | |
| Acute post-hemorrhagic anemia (285.1) | 18.3% | |
| Diabetes, uncomplicated (250.00) | 17.8% | |
| Hepatic encephalopathy (572.2) | 17.5% | |
| Hypertension NOS (401.9) | 17.4% | |
| Cirrhosis of liver NOS (571.5) | 16.1% | |
| Alcoholic Liver Cirrhosis (571.2) | 15.3% | |
| Thrombocytopenia NOS (287.5) | 15.0% | |
| Varices of other sites (456.8) | 13.7% | |
| Acute kidney failure NOS (584.9) | 13.3% | |
| Esophageal varices w/no bleeding (456.21) | 13.1% | |
| Acute respiratory failure (518.81) | 12.8% | |
| AHRQ comorbidity measure | ||
| AIDS | 0.7% | < 0.001 |
| CHF | 5.2% | < 0.001 |
| Coagulopathy | 35.7% | < 0.001 |
| Liver disease | 84.1% | < 0.001 |
| Lymphoma | 0.6% | < 0.001 |
| Fluid and electrolyte disorders | 36.8% | < 0.001 |
| Metastatic cancer | 1.3% | < 0.001 |
| Perivascular disease | 3.7% | < 0.001 |
| Pulmonary circulation disorders | 3.2% | < 0.001 |
| Renal failure | 13.6% | < 0.001 |
| Solid tumor without mets | 3.3% | < 0.001 |
| Valvular disease | 2.4% | < 0.001 |
| Weight loss | 14.0% | < 0.001 |
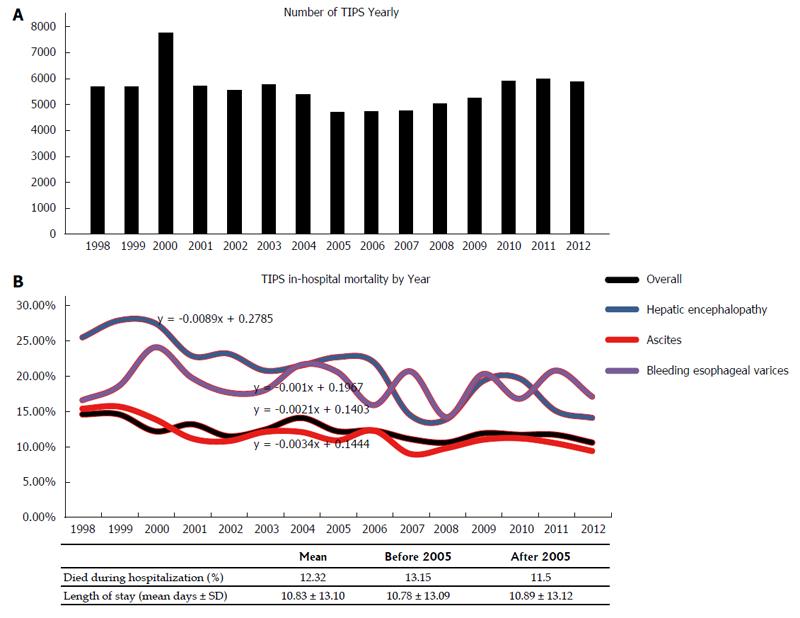
Figure 2 demonstrates the overall mortality outcomes of TIPS cases from 1998-2012. In all cases, 12.3% of patients died during hospitalization. More patients died during hospitalization before 2005 (13.5%) than after 2005 (11.5%). The overall mean (± SD) length of stay of 10.83 (± 13.10) d has remained relatively unchanged before (10.78 ± 13.09 d) and after 2005 (10.89 ± 13.12 d). Figure 2A depicts number of TIPS admissions yearly. Figure 2B charts TIPS in-hospital mortality by year and compares outcomes by common indications (ascites and esophageal variceal bleeding) and the complication of hepatic encephalopathy. As expected, overall mortality with TIPS is gradually declining (-0.22% yearly), more so in patients with ascites (-0.34% yearly) than esophageal variceal bleeding (-0.01% yearly). Patient mortality in those diagnosed with hepatic encephalopathy have shown a greater rate of decline than average (-0.89% yearly).
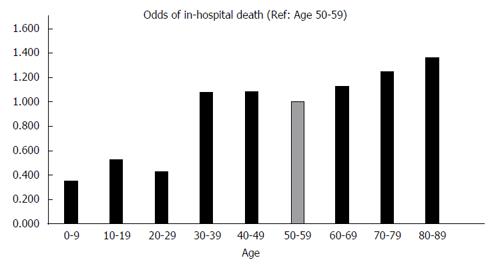
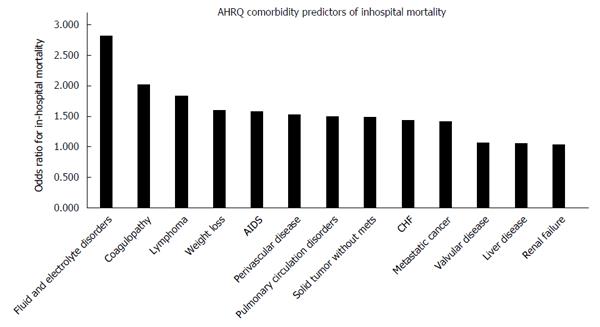
Through multivariate analysis using logistic regression and independent sample t-tests, we were able to identify predictors correlated with increased in-hospital death. Morbidity outcomes were directly compared to patient demographic factors (Table 3), hospital data (Table 3), and diagnostic factors (Table 4). Figure 3 compares odds of in-hospital mortality by age referenced to age group 50-59. Figure 4 depicts odds of in-hospital mortality in the presence of AHRQ comorbidity factors.
| OR: Death in Hospital | 95%CI: Lower | 95%CI: Upper | P value | |
| Demographic | ||||
| Age (every 1 yr increase) | 1.009 | 1.008 | 1.011 | < 0.001 |
| Age group (Reference: Age 50-59) | ||||
| 0-9 | 0.354 | 0.252 | 0.498 | < 0.001 |
| 10-19 | 0.529 | 0.417 | 0.672 | < 0.001 |
| 20-29 | 0.427 | 0.354 | 0.515 | < 0.001 |
| 30-39 | 1.076 | 0.986 | 1.175 | 0.100 |
| 40-49 | 1.085 | 1.027 | 1.147 | 0.004 |
| 50-59 | REF | REF | REF | REF |
| 60-69 | 1.124 | 1.063 | 1.189 | < 0.001 |
| 70-79 | 1.248 | 1.164 | 1.337 | < 0.001 |
| 80-89 | 1.360 | 1.197 | 1.546 | < 0.001 |
| 90-99 | 0.666 | 0.256 | 1.733 | 0.405 |
| Age > 70 (Ref: Age 0-70) | 1.280 | 1.206 | 1.359 | < 0.001 |
| Gender (Reference: Female) | ||||
| Male | 1.072 | 1.028 | 1.118 | 0.001 |
| Female | REF | REF | REF | REF |
| Race (Reference: Caucasian) | ||||
| Caucasian | REF | REF | REF | REF |
| Black | 1.809 | 1.667 | 1.963 | < 0.001 |
| Hispanic | 1.043 | 0.979 | 1.111 | 0.195 |
| Asian/Pacific Islander | 1.064 | 0.905 | 1.250 | 0.452 |
| Native American | 1.696 | 1.385 | 2.076 | < 0.001 |
| Other | 1.470 | 1.314 | 1.644 | < 0.001 |
| Unknown | 0.401 | 0.239 | 0.675 | 0.001 |
| Primary payer (Reference: Private) | ||||
| Medicare | 1.140 | 1.085 | 1.199 | < 0.001 |
| Medicaid | 1.113 | 1.052 | 1.177 | < 0.001 |
| Self-Pay | 1.610 | 1.482 | 1.749 | < 0.001 |
| Private | REF | REF | REF | REF |
| Income quartile by ZIP (Reference: 1st quartile) | ||||
| 1st quartile | REF | REF | REF | REF |
| 2nd quartile | 0.948 | 1.210 | 2.430 | 0.297 |
| 3rd quartile | 1.038 | 0.860 | 1.050 | 0.467 |
| 4th quartile | 1.012 | 0.940 | 1.150 | 0.830 |
| Missing income data | 1.714 | 0.910 | 1.130 | 0.002 |
| Transfer status (Reference: Non-transfer) | ||||
| Transferred in from different acute care hospital | 1.347 | 1.232 | 1.473 | < 0.001 |
| Non-transfer | REF | REF | REF | REF |
| Weekend admission status (Reference: Weekday) | ||||
| Weekend admission | 1.423 | 1.350 | 1.500 | < 0.001 |
| Weekday admission | REF | REF | REF | REF |
| Admission type (Reference: Elective) | ||||
| Emergency | 3.032 | 2.835 | 3.244 | < 0.001 |
| Urgent | 2.293 | 2.129 | 2.470 | < 0.001 |
| Elective | REF | REF | REF | REF |
| Trauma center | 4.541 | 2.772 | 7.440 | < 0.001 |
| Hospital | ||||
| Teaching hospital status (Reference: Non-teaching hospital) | ||||
| Teaching Hospital | 1.149 | 1.086 | 1.717 | < 0.001 |
| Non-Teaching Hospital | REF | REF | REF | REF |
| Hospital bed size (Reference: Large) | ||||
| Small | 0.858 | 0.773 | 0.953 | 0.004 |
| Medium | 0.940 | 0.891 | 0.992 | 0.025 |
| Large | REF | REF | REF | REF |
| Hospital region (Reference: West) | ||||
| Northeast | 1.449 | 1.365 | 1.538 | < 0.001 |
| Midwest | 0.982 | 0.925 | 1.043 | 0.572 |
| South | 0.917 | 0.868 | 0.969 | 0.002 |
| West | REF | REF | REF | REF |
| Hospital control (Reference: Private, investor owned) | ||||
| Private, Non-profit | 0.985 | 0.897 | 1.083 | < 0.001 |
| Private, Investor owned | REF | REF | REF | REF |
| OR: Death in Hospital | 95%CI: Lower | 95%CI: Upper | P value | |
| Number of diagnoses | 1.095 | 1.091 | 1.099 | < 0.000 |
| Number of procedures | 1.249 | 1.242 | 1.256 | < 0.000 |
| Diagnosis (Reference: No disease) | ||||
| Portal hypertension (5723) | 0.689 | 0.660 | 0.719 | 0.000 |
| Ascites (7895) | 1.020 | 0.977 | 1.066 | 0.369 |
| Esophageal variceal bleeding (45620) | 2.187 | 2.098 | 2.279 | 0.000 |
| Other ascites (78959) | 0.783 | 0.741 | 0.827 | 0.000 |
| Acute post-hemorrhagic anemia (2851) | 2.011 | 1.920 | 2.105 | 0.000 |
| Diabetes, uncomplicated (25000) | 0.474 | 0.443 | 0.506 | 0.000 |
| Hepatic encephalopathy (5722) | 2.217 | 2.118 | 2.322 | 0.000 |
| Hypertension NOS (4019) | 0.597 | 0.561 | 0.635 | 0.000 |
| Cirrhosis of liver NOS (5715) | 0.836 | 0.789 | 0.886 | 0.000 |
| Alcoholic liver cirrhosis (5712) | 1.079 | 1.021 | 1.141 | 0.007 |
| Thrombocytopenia NOS (2875) | 1.081 | 1.022 | 1.142 | 0.006 |
| Varices of other sites (4568) | 0.784 | 0.736 | 0.835 | 0.000 |
| Acute kidney failure NOS (5849) | 4.359 | 4.162 | 4.566 | 0.000 |
| Esophageal varices w/no bleeding (45621) | 0.445 | 0.411 | 0.481 | 0.000 |
| Acute respiratory failure (51881) | 8.246 | 7.875 | 8.634 | 0.000 |
| AHRQ comorbidity measures (Reference: No disease) | ||||
| AIDS | 1.579 | 1.216 | 2.050 | 0.001 |
| CHF | 1.437 | 1.300 | 1.587 | < 0.001 |
| Coagulopathy | 2.016 | 1.918 | 2.119 | < 0.001 |
| Liver disease | 1.051 | 0.981 | 1.125 | 0.156 |
| Lymphoma | 1.842 | 1.414 | 2.402 | < 0.001 |
| Fluid and electrolyte disorders | 2.823 | 2.684 | 2.969 | < 0.001 |
| Metastatic cancer | 1.412 | 1.167 | 1.708 | < 0.001 |
| Perivascular disease | 1.527 | 1.292 | 1.806 | <0.001 |
| Pulmonary circulation disorders | 1.496 | 1.249 | 1.792 | < 0.001 |
| Renal failure | 1.036 | 0.933 | 1.151 | 0.506 |
| Solid tumor without mets | 1.491 | 1.322 | 1.681 | < 0.001 |
| Valvular disease | 1.067 | 0.910 | 1.252 | 0.424 |
| Weight loss | 1.595 | 1.453 | 1.751 | < 0.001 |
Compared to the most common cohort of patients age 50-59, relative odds of in-hospital mortality were significantly lower in patients below age 30 (OR = 0.439, P < 0.001). Beyond age 70, odds of death appeared to increase incrementally, though statistically significant odds data for patients 90-99 years old is unavailable (P = 0.405). Males had at slightly higher odds of in-hospital mortality than females (OR = 1.072, P < 0.001). Black and Native American patients had markedly higher odds in-hospital death compared to Caucasians (OR = 1.809, P < 0.001 and OR = 1.696, P < 0.001). Self-paying patients had 1.610 times higher odds of in-hospital death than private payers (P < 0.001). Patient income did not appear to be a statistically significant marker of in-hospital mortality.
Transfers from an acute care hospital were at 1.347 times higher odds of in-hospital mortality than non-transfers (P < 0.001), while weekend admissions were at 1.423 times higher odds of in-hospital death than weekday admissions (P < 0.001). Compared to elective admissions, those categorized by the hospital as emergency admissions were at 3.032 times higher risk of in-hospital death (P < 0.001).
Patients in teaching hospitals were at slightly higher odds of in-hospital death (OR = 1.149, P < 0.001). Patients admitted to hospitals in the Northeast had considerably higher odds of in-hospital death to those in the West (OR = 1.449, P < 0.001), while patients in the South had slightly lower odds (OR = 0.917, P = 0.002). Patients in the Midwest had similar odds (OR = 0.982, P = 0.572).
The number of diagnoses and number of procedures show expectedly positive correlations with in-hospital death, though the number of procedures exhibit a stronger relationship (OR = 1.249 per one increase in number of procedures, P < 0.001). Of the fifteen most common diagnoses, acute respiratory failure exhibited highest odds of in-hospital death (OR = 8.246, P < 0.001), followed by acute kidney failure NOS (OR = 4.359, P < 0.001) and hepatic encephalopathy (OR = 2.217, P < 0.001). Odds of death in patients diagnosed with ascites were not significantly different than those undiagnosed (OR = 1.020, P = 0.369). Patients diagnosed with bleeding esophageal varices had a mortality odds ratio of 2.217 (P < 0.001) compared to 0.445 (P < 0.001) in patients diagnosed with non-bleeding varices. Comorbidity measures at highest odds of death were fluid and electrolyte disorders (OR = 2.823, P < 0.001), coagulopathy (OR = 2.016, P < 0.001), and lymphoma (OR = 1.842, P < 0.001) when compared to no comorbidity.
Determining useful prognostic markers for mortality is essential part of defining candidacy of any interventional procedure. A number of models for predicting TIPS outcomes have been implemented, with the most commonly applied in current practice being MELD[7,8]. Although these methods have been successful in stratifying patient risk based on biochemical markers such as bilirubin and creatinine, there remains interest on identifying new predictors that progress the way we monitor and follow up on patients[8,10-17]. Our study is the first large-scale study to examine patient demographic, hospital, and diagnostic data as potential outcome markers for TIPS patients for all indications.
The sheer volume of patient data provided by the NIS brings unique statistical value to patient factors previously not associated with patient mortality. For example, although studies in the past have been unable to find clear associations between age and mortality, our data supports this relationship[16,17]. In our study, patients over 70 were at 1.28 times higher odds for in-hospital mortality. Stepwise logistic regression analysis provided an odds ratio of 1.009 (1.008-1.011, P < 0.001) for every one year increase in age. At under 30, the odds of in-patient mortality dropped significantly (OR = 0.354-0.529, P < 0.001).
The role of ethnicity as predictor of clinical outcomes after TIPS has been controversial. One study on 643 patients finds patient ethnicity to be a poor indicator of early patient mortality[16], where another on 163 patients finds Hispanic patients to have a potential survival advantage[13]. In our study on 86,621 admissions, we found African-American (OR = 1.809, P < 0.001) and Native American (OR = 1.696, P < 0.001) patients to have statistically significant higher odds of in-hospital mortality than Caucasian patients. In contrast, Hispanic and Asian/Pacific Islander patients had similar in-house mortality as Caucasians.
Statistical relationships in any study should always warrant careful consideration. For instance, although self-payer patients were at considerably higher odds of in-patient mortality (OR = 1.610 vs private insurance), they were predominantly emergency admissions (61.1%) and therefore high risk (OR = 3.032 vs elective admissions, P < 0.001). One study on trauma victims finds a similar association between self-payers and a significantly higher mortality rate[18]. Similar to self-payers, weekend admissions also had higher odds of in-hospital mortality yet were comprised of mostly emergency admissions (65.8% vs 42.0% for weekday admissions).
Between hospital regions, the Northeast stood out with the highest mortality risk at odds 1.449 times higher than the Western region (P < 0.001). Further analysis of 2012 NIS data finds patients in the Northeast to have the highest mortality across all hospitalizations, just slightly but significantly at 1.095 times higher odds than in the West (P < 0.001).
Diagnosis as a predictive factor provides a different perspective than established clinical criteria. To illustrate, in a scenario where Child-Pugh and MELD scoring are unknown, we can anticipate a patient undergoing TIPS for esophageal variceal bleeding to be at roughly twice the odds of death in hospital following TIPS than for patients with other indications. Likewise, TIPS patients with hepatopulmonary syndrome, portopulmonary hypertension, or hepatic hydrothorax should be monitored closely for acute respiratory failure, which when diagnosed are expected to have around 8 times higher odds of in-hospital death. The same ideology applies to patient comorbidity data, especially in the situation where a physician is evaluating a patient for an elective procedure. Based on our data, physicians should be especially wary of fluid and electrolyte disorders (OR = 2.823, P < 0.001), coagulopathy (OR = 2.016, P < 0.001), and lymphoma (OR = 1.842, P < 0.001). These data should alert physicians to implement closer monitoring before and during TIPS procedure and emphasize on closer following up on those patients with higher risk of post-TIPS mortality.
From a trends perspective, NIS data supports improved clinical outcomes throughout the 15-year study period (in-patient mortality declining on average -0.22% yearly), with the primary driving factor likely being the increasing use of PTFE covered stents[2,9]. This is particularly evident comparing in-patient mortality rates before widespread adoption of PTFE covered stents in 1998-2004 (13.15%) to after in 2005-2012 (11.50%).
Identifying subgroups with minimal reductions in mortality provides insight into potential areas of improvement. Although mortality in patients with ascites have declined overall (-0.34% yearly), mortality in patients with esophageal variceal bleeding have not changed substantially over the past 15 years (-0.01% yearly). In the same way, identifying subgroups that have shown sizable reductions in mortality highlight positives in the evolution of patient management. Hepatic encephalopathy is a frequent complication related to TIPS, with incidence rates ranging between 22%-50%[19-23]. For patients diagnosed with hepatic encephalopathy, the decline of in-patient mortality (-0.89% yearly) faster than the mean reinforces that management strategies have improved outcomes in this patient cohort.
Limitations of our study include those traditionally associated with retrospective research such as missing or incorrect data, selection bias, and the inability to control other sources of exposure. Also, NIS data is weighted and does not represent the entire cohort of patients undergoing TIPS in the United States. Changes in weighting with the NIS redesign in 2012 may impact the consistency of year-to-year analysis. Associative factors are drawn from a nationwide perspective and both internal and external factors are not held constant. Details on out-patient mortality are not available using NIS data.
In the first 15-year nationwide TIPS procedure mortality assessment, we outline in-patient mortality trends and provide comparison between demographic, regional, and diagnostic data as potential predictive markers. Results from this study are intended to aid practitioners in identifying populations that require closer monitoring to improve post-TIPS mortality and clinical outcomes of TIPS.
Transjugular intrahepatic portosystemic shunt (TIPS) became a main interventional procedure in treating patients with complications of portal hypertension. However, there is no large-scale, national trends data investigating in-patient death following TIPS. Using the National Inpatient Sample (NIS) database from 1998 to 2012, the authors demonstrated downtrend in overall in-patient mortality associated with TIPS and they evaluated several factors including demographic, hospital and co-morbidities contributing to in-patient mortality in 83884 TIPS performed in the United States hospitals in 15 years.
Utilization of a nationwide, large database (NIS/HCUP) in assessing the mortality and predictors of TIPS procedure has not been fully studied. Especially, an evaluation of a large-scale database for 15 years has never been performed. In this study, the authors demonstrated the national trends of TIPS procedures and several predictors of in-patient mortality in TIPS procedures.
Using NIS/HCUP database in TIPS outcomes.
Results from this study are intended to aid hepatologists, gastroenterologists, internists, liver transplant surgeons and interventional radiologists in identifying populations that require closer monitoring and follow up to improve post-TIPS mortality and clinical outcomes of TIPS.
In this study, the authors evaluated several factors contributing to in-patient mortality in 83884 TIPS performed in the United States in 15 years using the NIS database from 1998 to 2012. In general, the main idea is interesting because this is a large-scale, national trends data investigating in-patient death following TIPS. Factors affecting patient survival following TIPS have been extensively studied.
Manuscript Source: Invited manuscript
Specialty Type: Gastroenterology and Hepatology
Country of Origin: United States
Peer-Review Report Classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Alves A, Qiu B S- Editor: Gong ZM L- Editor: A E- Editor: Ma S
| 1. | Boyer TD, Haskal ZJ. The Role of Transjugular Intrahepatic Portosystemic Shunt (TIPS) in the Management of Portal Hypertension: update 2009. Hepatology. 2010;51:306. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 390] [Cited by in F6Publishing: 380] [Article Influence: 27.1] [Reference Citation Analysis (1)] |
| 2. | Yang Z, Han G, Wu Q, Ye X, Jin Z, Yin Z, Qi X, Bai M, Wu K, Fan D. Patency and clinical outcomes of transjugular intrahepatic portosystemic shunt with polytetrafluoroethylene-covered stents versus bare stents: a meta-analysis. J Gastroenterol Hepatol. 2010;25:1718-1725. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 98] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Quiroga J, Sangro B, Núñez M, Bilbao I, Longo J, García-Villarreal L, Zozaya JM, Betés M, Herrero JI, Prieto J. Transjugular intrahepatic portal-systemic shunt in the treatment of refractory ascites: effect on clinical, renal, humoral, and hemodynamic parameters. Hepatology. 1995;21:986-994. [PubMed] [Cited in This Article: ] |
| 4. | Ferral H. The evaluation of the patient undergoing an elective transjugular intrahepatic portosystemic shunt procedure. Semin Intervent Radiol. 2005;22:266-270. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Ferral H, Gamboa P, Postoak DW, Albernaz VS, Young CR, Speeg KV, McMahan CA. Survival after elective transjugular intrahepatic portosystemic shunt creation: prediction with model for end-stage liver disease score. Radiology. 2004;231:231-236. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 128] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 6. | Richter GM, Noeldge G, Palmaz JC, Roessle M. The transjugular intrahepatic portosystemic stent-shunt (TIPSS): results of a pilot study. Cardiovasc Intervent Radiol. 1990;13:200-207. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 99] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 7. | Angermayr B, Cejna M, Karnel F, Gschwantler M, Koenig F, Pidlich J, Mendel H, Pichler L, Wichlas M, Kreil A. Child-Pugh versus MELD score in predicting survival in patients undergoing transjugular intrahepatic portosystemic shunt. Gut. 2003;52:879-885. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 207] [Cited by in F6Publishing: 223] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 8. | Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864-871. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1967] [Cited by in F6Publishing: 1911] [Article Influence: 79.6] [Reference Citation Analysis (0)] |
| 9. | Saad WE. The history and future of transjugular intrahepatic portosystemic shunt: food for thought. Semin Intervent Radiol. 2014;31:258-261. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Kim HK, Kim YJ, Chung WJ, Kim SS, Shim JJ, Choi MS, Kim do Y, Jun DW, Um SH, Park SJ. Clinical outcomes of transjugular intrahepatic portosystemic shunt for portal hypertension: Korean multicenter real-practice data. Clin Mol Hepatol. 2014;20:18-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Harrod-Kim P, Waldman DL. Abnormal portal venous flow at sonography predicts reduced survival after transjugular intrahepatic portosystemic shunt creation. J Vasc Interv Radiol. 2005;16:1459-1464. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Harrod-Kim P, Saad WE, Waldman D. Predictors of early mortality after transjugular intrahepatic portosystemic shunt creation for the treatment of refractory ascites. J Vasc Interv Radiol. 2006;17:1605-1610. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Membreno F, Baez AL, Pandula R, Walser E, Lau DT. Differences in long-term survival after transjugular intrahepatic portosystemic shunt for refractory ascites and variceal bleed. J Gastroenterol Hepatol. 2005;20:474-481. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Grunwald D, Tapper EB, Jiang ZG, Ahmed M, Malik R. A Standardized Assessment of Functional Disability Predicts 1-year Mortality in Patients Undergoing Transjugular Intrahepatic Portosystemic Shunt for Refractory Ascites. J Clin Gastroenterol. 2016;50:75-79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Heinzow HS, Lenz P, Köhler M, Reinecke F, Ullerich H, Domschke W, Domagk D, Meister T. Clinical outcome and predictors of survival after TIPS insertion in patients with liver cirrhosis. World J Gastroenterol. 2012;18:5211-5218. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 11] [Reference Citation Analysis (0)] |
| 16. | Dhanasekaran R, Gonzales P, West J, Subramanian R, Parekh S, Spivey JR, Reshamwala P, Martin LG, Kim HS. Predictors of early mortality post transjugular intrahepatic portosystemic shunts and the role of hepatic venous pressure gradient. Gastrointest Inte. 2012;1:63-68. [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Russo MW, Jacques PF, Mauro M, Odell P, Brown RS. Predictors of mortality and stenosis after transjugular intrahepatic portosystemic shunt. Liver Transpl. 2002;8:271-277. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Chikani V, Salvino C, Hussaini K, Vossbrink A, Ng AR, Bobrow B, Skubic J, Martinez R. Self-pay trauma victims have a higher mortality rate than patients with different payment methods. Ann Adv Automot Med. 2013;57:345-346. [PubMed] [Cited in This Article: ] |
| 19. | Freedman AM, Sanyal AJ, Tisnado J, Cole PE, Shiffman ML, Luketic VA, Purdum PP, Darcy MD, Posner MP. Complications of transjugular intrahepatic portosystemic shunt: a comprehensive review. Radiographics. 1993;13:1185-1210. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 229] [Cited by in F6Publishing: 234] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 20. | Casadaban LC, Parvinian A, Minocha J, Lakhoo J, Grant CW, Ray CE, Knuttinen MG, Bui JT, Gaba RC. Clearing the Confusion over Hepatic Encephalopathy After TIPS Creation: Incidence, Prognostic Factors, and Clinical Outcomes. Dig Dis Sci. 2015;60:1059-1066. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 21. | Tripathi D, Ferguson J, Barkell H, Macbeth K, Ireland H, Redhead DN, Hayes PC. Improved clinical outcome with transjugular intrahepatic portosystemic stent-shunt utilizing polytetrafluoroethylene-covered stents. Eur J Gastroenterol Hepatol. 2006;18:225-232. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 68] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 22. | Angeloni S, Merli M, Salvatori FM, De Santis A, Fanelli F, Pepino D, Attili AF, Rossi P, Riggio O. Polytetrafluoroethylene-covered stent grafts for TIPS procedure: 1-year patency and clinical results. Am J Gastroenterol. 2004;99:280-285. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 59] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Bureau C, Pagan JC, Layrargues GP, Metivier S, Bellot P, Perreault P, Otal P, Abraldes JG, Peron JM, Rousseau H. Patency of stents covered with polytetrafluoroethylene in patients treated by transjugular intrahepatic portosystemic shunts: long-term results of a randomized multicentre study. Liver Int. 2007;27:742-747. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 220] [Cited by in F6Publishing: 206] [Article Influence: 12.1] [Reference Citation Analysis (0)] |