Copyright
©The Author(s) 2016.
World J Gastroenterol. Jan 14, 2016; 22(2): 600-617
Published online Jan 14, 2016. doi: 10.3748/wjg.v22.i2.600
Published online Jan 14, 2016. doi: 10.3748/wjg.v22.i2.600
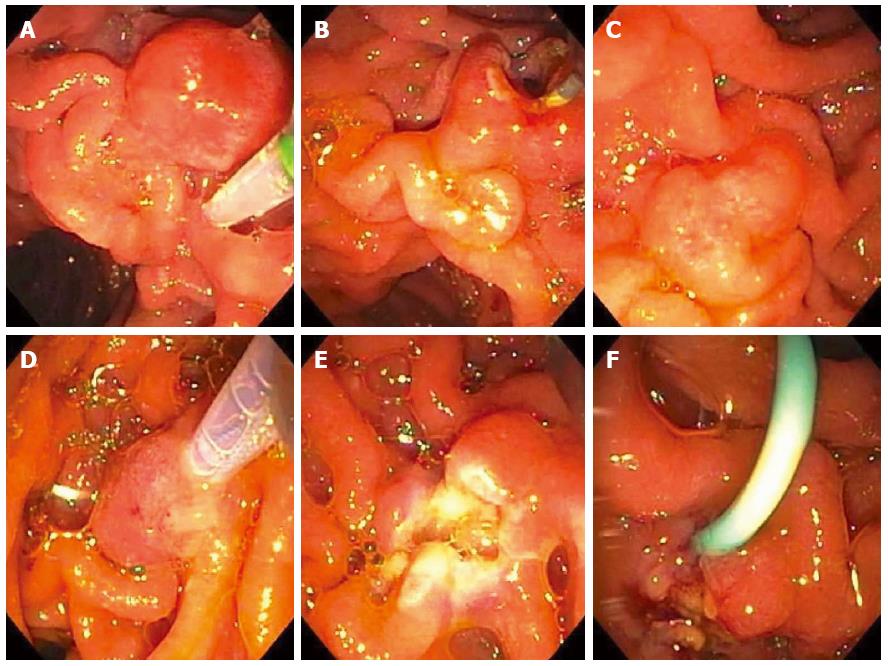
Figure 13 A 63-year-old woman presented with chronic abdominal pain and recurrent acute pancreatitis in the setting of pancreas divisum.
Endoscopic retrograde cholangiopancreatography (ERCP) for minor papillotomy and pancreatic duct (PD) stenting was intended. During ERCP, the minor papilla was found to be enlarged to about 1-cm in size and was somewhat hard on palpation with the sphincterotome (A). A minor papillotomy was performed (B), the minor papilla was biopsied, and a pancreatic duct (PD) stent was placed. Pathology showed adenoma, and the patient returned for minor papillectomy several weeks later. The prior papillotomy had healed (C), and hot-snare resection was used to resect the minor papilla without a saline lift (D); No residual adenomatous tissue was seen after minor papillectomy (E); and biopsies of the resection margins provided pathologic confirmation of complete resection. A PD stent was left at the conclusion of the procedure (F) and rectal indomethacin was administered.
- Citation: Gaspar JP, Stelow EB, Wang AY. Approach to the endoscopic resection of duodenal lesions. World J Gastroenterol 2016; 22(2): 600-617
- URL: https://www.wjgnet.com/1007-9327/full/v22/i2/600.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i2.600