Published online May 21, 2016. doi: 10.3748/wjg.v22.i19.4781
Peer-review started: January 21, 2016
First decision: March 7, 2016
Revised: March 20, 2016
Accepted: March 30, 2016
Article in press: March 30, 2016
Published online: May 21, 2016
Processing time: 117 Days and 23.4 Hours
Although primary gastrointestinal lymphoma is a rare malignancy, it can cause an intussusception in adults and can be a clinically challenging condition to manage. Intussusception could progress to life-threatening complications if left untreated or could delay chemotherapy if inappropriate surgical management is used. We report a 31-year-old man diagnosed with human immunodeficiency virus who was being treated with antiretroviral therapy. He presented with nausea, vomiting, poor appetite, and intermittent, cramping abdominal pain for over 1 wk. Abdominal computed tomography revealed a well-defined homogeneous mass in the mesenteric root region, together with a long segmental wall thickening in the ileum with ileocolic-type intussusception, which was suspected to be caused by a lymphoma. The intussusception was successfully laparoscopically reduced, and the tumor involvement of the appendix was confirmed by appendectomy with intraoperative frozen section. Systemic chemotherapy was immediately initiated after surgery without the need for bowel resection.
Core tip: In general, surgical management of adult with an intussusception mandates the resection of the involved bowel segment. However, the surgical resection of an intussusception that is caused by intestinal lymphoma is controversial because the intestinal involvement is generally diffuse. Concerning the diffuse invasive characteristics of gastrointestinal lymphomas, laparoscopic reduction of intussusceptions and appendectomy with intraoperative frozen section were both performed that enabled us to intraoperatively identify the tumor involvement of the resected appendix. By avoiding bowel resection, systemic chemotherapy could be initiated early after surgery.
- Citation: Yang TW, Lin YY, Tsuei YW, Chen YL, Huang CY, Hsu SD. Successful management of adult lymphoma-associated intussusception by laparoscopic reduction and appendectomy. World J Gastroenterol 2016; 22(19): 4781-4785
- URL: https://www.wjgnet.com/1007-9327/full/v22/i19/4781.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i19.4781
Although an intussusception is common in the pediatric population, it is a rare[1-5] but clinically challenging condition in adults, accounting for 1%-5% of mechanical bowel obstruction cases[6,7]. If left untreated, an intussusception could progress to tissue necrosis, bowel perforation, or peritonitis. In adults, it is typically because of the presence of a pathological lead point within the bowel, which is malignant in over half of all cases[6,7]. Most surgeons agree that adults with an intussusception require resection via surgery because most of such cases have lesions intraluminally. Nevertheless, the optimal resected range and if the intussusception should be reduced or not remain a controversy[8]. In this study, we present an unusual case of an adult with ileocolic intussusception that is caused by an intestinal lymphoma. He was successfully treated with laparoscopic surgery without bowel resection.
The patient was a 31-year-old man with human immunodeficiency virus (HIV) who was being treated with antiretroviral therapy. He presented with nausea, vomiting, poor appetite, and intermittent, cramping abdominal pain for over 1 wk. On arrival, his blood pressure was 126/66 mmHg; pulse rate, 92 beats per minute; and body temperature, 36.3 °C. Physical examination disclosed tympanic sounds on percussion and mild periumbilical tenderness on palpation. Upper gastrointestinal (GI) panendoscopy was performed but revealed no specific findings; however, abdominal sonography subsequently identified a mass over the periumbilical region. Therefore, a contrast-enhanced computed tomography (CT) of the abdomen was performed, which revealed a well-defined, homogeneous mass, measuring approximately 6 cm × 4 cm × 7 cm, in the mesenteric root region (Figure 1, asterisk). The lymphoma was clinically highly suspected on the basis of imaging finding. In addition, there was evidence of a long segmental wall thickening in the terminal ileum with an ileocolic-type intussusception, and a lymphoma in the terminal ileum was also suspected (Figure 1, arrow).
The patient underwent diagnostic laparoscopy, which revealed tumors with diffuse involvement that included the terminal ileum and proximal colon. On closer inspection, the terminal ileum and appendix were both invaginating into the proximal colon, and the tip of the appendix was still visible outside the invagination. Both of the invaginated ileum and proximal colon were relatively healthy, with no ischemic changes (Figure 2). We used non-traumatic graspers to retract the ileum and residual appendix and successfully reduced the intussusception. The appendix appeared red and swollen under laparoscopy.
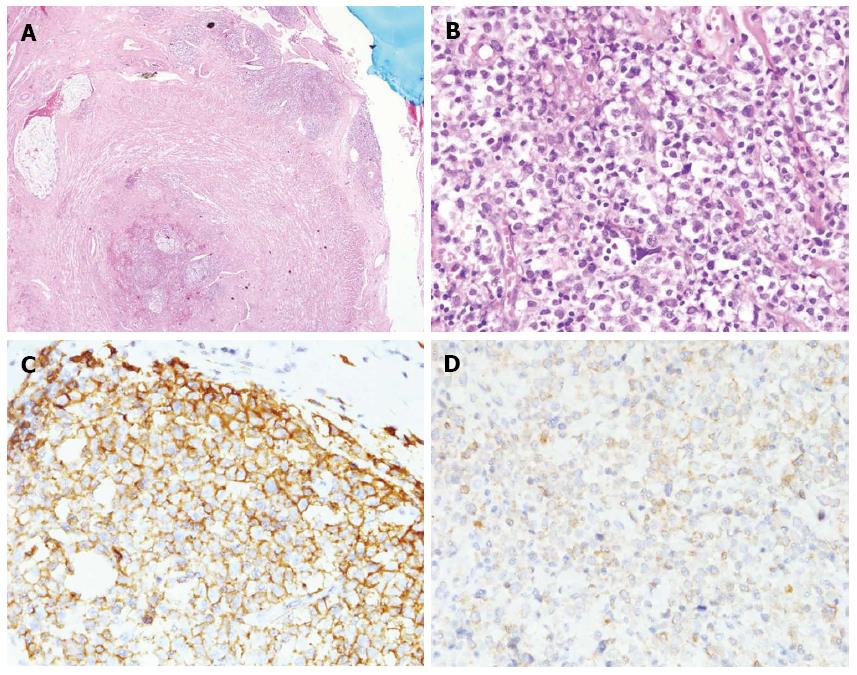
Tumor cell infiltration in the serosal layer of the appendix was confirmed by an immediate frozen section of the appendix, and the final pathology result indicated a diffuse large B-cell lymphoma (Figure 3). The patient received systemic chemotherapy on postoperative day 12, and enteral feeding was well tolerated. The patient was subsequently discharged with good bowel movements and without any complication. He was referred to hematology for further chemotherapy treatment.
The optimal management of an intussusception remains controversial in adults. Surgical management usually involves the resection of the affected bowel to determine the underlying cause, which is malignant in more than half of all cases[9]. In contrast, chemotherapy is often the preferred treatment for primary intestinal lymphomas; surgery plays a limited role because the diffuse involvement would necessitate complete resection that might be complicated with short bowel syndrome[10-13]. Therefore, it is recommended that resection be reserved for patients with acute complications, such as obstruction, hemorrhage, abscess, or perforation, with no evidence supporting the uses of preventive surgery[14,15].
After Kaposi sarcoma, lymphomas are the second most malignancy that is observed in patients with HIV[16], and the most common type are diffuse large B-cell non-Hodgkin lymphoma[17]. GI tract involvement of lymphoma is common in patients with HIV[18], including the appendix, which is considered a part of the gut-associated lymphoid tissue. Leukemic and lymphomatous tumor involvement of the appendix can be primary or secondary[19]. Typical CT findings of the intestinal lymphoma include a enormous mass, extenseive infiltration fat planes preservation, multiple site involvement, and associated bulky lymphadenopathy[20,21]. Other differential diagnoses similar to these CT findings include carcinoids, adenocarcinomas, sarcoma (e.g., gastrointestinal stromal tumor), and leiomyomatosis peritonealis disseminata. In our case, there was a well-defined homogeneous mass in the mesenteric root region and a long segmental wall thickening in the terminal ileum on contrast-enhanced CT of the abdomen. Intestinal lymphoma was presumed on the basis of this imaging, and tumor involvement of the appendix was suspected because of its proximity to the terminal ileum. During surgery, the use of a frozen section of the resected appendix helped us quickly confirm that there was tumor-cell infiltration of the appendix. Given these findings, surgical management was limited to laparoscopic reduction of the ileocolic intussusception and appendectomy. Therefore, possible complications from diffuse large bowel resection could be avoided. Had the frozen section of the resected appendix not revealed tumor involvement, we might have considered performing a tumor biopsy instead.
Most intussusceptions are of the ileocolic type and occur because of a leading point that is located in the ileocolic region[1]. Because of this, we used traction of the appendix with surgical forceps to make the ileocolic intussusception easier to reduce and help perform the laparoscopic appendectomy.
Although adjuvant chemotherapy is typically initiated within 6-8 wk after surgery, several recent meta-analyses have confirmed that delayed administration of adjuvant chemotherapy is associated with significantly reduced overall survival[22,23]. Laparoscopic surgery is typical considered as a less-injurious surgery that enables earlier initiation of adjuvant chemotherapy[24,25]. Our patient was able to initiate systemic chemotherapy without too much delay because the surgery was limited to laparoscopic reduction of the intussusception and appendectomy.
In conclusion, diffuse large B-cell lymphomas may involve multiple sites in the GI tract and can cause intussusception in patients with HIV. To minimize any surgery-related complications and to improve prognosis, surgeons could consider laparoscopic reduction and appendectomy with intraoperative frozen section to identify tumor invasion. This approach facilitates earlier initiation of postoperative chemotherapy and could improve patient outcomes.
A 31-year-old human immunodeficiency virus (HIV)-infected man who was being treated with antiretroviral therapy, presented with nausea, vomiting, poor appetite, and intermittent, cramping abdominal pain for over 1 wk.
Nausea, vomiting, and intermittent abdominal cramping pain with mild periumbilical tenderness.
Gastroesophageal reflux disease, peptic ulcer disease, irritable bowel syndrome, small or larbe bowel obstruction, cholelithiasis or pancreatitis.
All laboratory tests were within normal limits.
Computed tomography (CT) of the abdomen revealed a 6 cm x 4 cm x 7 cm well-defined mass in the mesenteric root region, and a long segmental wall thickening in the terminal ileum with an ileocolic-type intussusception.
Diffuse large B-cell lymphoma.
Laparoscopic reduction and appendectomy with postoperative systemic chemotherapy.
Intussusception in patients with HIV is often associated with lymphoma, and other causes including Kaposi sarcoma and opportunistic infection had been reported.
After Kaposi sarcoma, non-Hodgkin lymphomas are the second most malignancy that is observed in patients with HIV, and the most common type are diffuse large B-cell lymphoma.
For adult lymphoma-associated intussusception with diffuse intestinal involvement, laparoscopic reduction and appendectomy with intraoperative frozen section could be an alternative to make a definite diagnosis and avoid bowel resection.
CT findings in our case are not specific to lymphoma and could evoke other differential diagnosis.
P- Reviewer: Jerraya H, Manguso F S- Editor: Ma YJ L- Editor: A E- Editor: Zhang DN
| 2. | Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88-94. [PubMed] |
| 3. | Weilbaecher D, Bolin JA, Hearn D, Ogden W. Intussusception in adults. Review of 160 cases. Am J Surg. 1971;121:531-535. [PubMed] |
| 4. | Reijnen HA, Joosten HJ, de Boer HH. Diagnosis and treatment of adult intussusception. Am J Surg. 1989;158:25-28. [PubMed] |
| 5. | Nagorney DM, Sarr MG, McIlrath DC. Surgical management of intussusception in the adult. Ann Surg. 1981;193:230-236. [PubMed] |
| 6. | Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, Theodosopoulos T. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15:407-411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 428] [Cited by in RCA: 501] [Article Influence: 31.3] [Reference Citation Analysis (2)] |
| 7. | Zubaidi A, Al-Saif F, Silverman R. Adult intussusception: a retrospective review. Dis Colon Rectum. 2006;49:1546-1551. [PubMed] |
| 8. | Tan KY, Tan SM, Tan AG, Chen CY, Chng HC, Hoe MN. Adult intussusception: experience in Singapore. ANZ J Surg. 2003;73:1044-1047. [PubMed] |
| 9. | Yakan S, Caliskan C, Makay O, Denecli AG, Korkut MA. Intussusception in adults: clinical characteristics, diagnosis and operative strategies. World J Gastroenterol. 2009;15:1985-1989. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 111] [Cited by in RCA: 134] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 10. | Takeuchi K, Tsuzuki Y, Ando T, Sekihara M, Hara T, Kori T, Kuwano H. The diagnosis and treatment of adult intussusception. J Clin Gastroenterol. 2003;36:18-21. [PubMed] |
| 11. | Erkan N, Haciyanli M, Yildirim M, Sayhan H, Vardar E, Polat AF. Intussusception in adults: an unusual and challenging condition for surgeons. Int J Colorectal Dis. 2005;20:452-456. [PubMed] |
| 12. | Khan MN, Agrawal A, Strauss P. Ileocolic Intussusception - A rare cause of acute intestinal obstruction in adults; Case report and literature review. World J Emerg Surg. 2008;3:26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Franz B, Rabl C, Neureiter D, Öfner D, Emmanuel K. Emergency surgery for enteric and colonic intussusception in adults. Eur Surg. 2010;42:180-183. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Cheung MC, Housri N, Ogilvie MP, Sola JE, Koniaris LG. Surgery does not adversely affect survival in primary gastrointestinal lymphoma. J Surg Oncol. 2009;100:59-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Cirocchi R, Farinella E, Trastulli S, Cavaliere D, Covarelli P, Listorti C, Desiderio J, Barberini F, Avenia N, Rulli A. Surgical treatment of primitive gastro-intestinal lymphomas: a systematic review. World J Surg Oncol. 2011;9:145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Danzig JB, Brandt LJ, Reinus JF, Klein RS. Gastrointestinal malignancy in patients with AIDS. Am J Gastroenterol. 1991;86:715-718. [PubMed] |
| 17. | Mantina H, Wiggill TM, Carmona S, Perner Y, Stevens WS. Characterization of Lymphomas in a high prevalence HIV setting. J Acquir Immune Defic Syndr. 2010;53:656-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Parente F, Rizzardini G, Cernuschi M, Antinori S, Fasan M, Bianchi Porro G. Non-Hodgkin’s lymphoma and AIDS: frequency of gastrointestinal involvement in a large Italian series. Scand J Gastroenterol. 1993;28:315-318. [PubMed] |
| 19. | Khanna M, Buddhavarapu SR. Primary Burkitt’s Lymphoma Of The Appendix Presenting As Acute Abdomen: A Case Report. J Radiol Case Rep. 2008;2:9-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Ghai S, Pattison J, Ghai S, O’Malley ME, Khalili K, Stephens M. Primary gastrointestinal lymphoma: spectrum of imaging findings with pathologic correlation. Radiographics. 2007;27:1371-1388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 116] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 21. | Lee WK, Lau EW, Duddalwar VA, Stanley AJ, Ho YY. Abdominal manifestations of extranodal lymphoma: spectrum of imaging findings. AJR Am J Roentgenol. 2008;191:198-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Des Guetz G, Nicolas P, Perret GY, Morere JF, Uzzan B. Does delaying adjuvant chemotherapy after curative surgery for colorectal cancer impair survival? A meta-analysis. Eur J Cancer. 2010;46:1049-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 175] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 23. | Biagi JJ, Raphael MJ, Mackillop WJ, Kong W, King WD, Booth CM. Association between time to initiation of adjuvant chemotherapy and survival in colorectal cancer: a systematic review and meta-analysis. JAMA. 2011;305:2335-2342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 536] [Cited by in RCA: 481] [Article Influence: 34.4] [Reference Citation Analysis (0)] |
| 24. | Zheng Z, Jemal A, Lin CC, Hu CY, Chang GJ. Comparative effectiveness of laparoscopy vs open colectomy among nonmetastatic colon cancer patients: an analysis using the National Cancer Data Base. J Natl Cancer Inst. 2015;107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 25. | Day AR, Middleton G, Smith RV, Jourdan IC, Rockall TA. Time to adjuvant chemotherapy following colorectal cancer resection is associated with an improved survival. Colorectal Dis. 2014;16:368-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |