Published online Feb 21, 2015. doi: 10.3748/wjg.v21.i7.2225
Peer-review started: July 8, 2014
First decision: August 6, 2014
Revised: August 21, 2014
Accepted: September 29, 2014
Article in press: September 30, 2014
Published online: February 21, 2015
Schwannomas are rarely observed in the gastrointestinal tract. The most common symptoms of a gastric schwannoma are abdominal pain or dyspepsia, gastrointestinal bleeding, and an abdominal mass. Many gastric schwannomas are asymptomatic and are discovered incidentally or at postmortem. The diagnosis of a schwannoma is based on immunohistochemical positivity for S-100 protein. We present a case report of a rare complication of gastric schwannoma causing gastroduodenal intussusception that was successfully managed by a Billroth II distal gastrectomy. In this rare case, the patient had intermittent, colicky abdominal pain, nausea, and vomiting for over 4 wk accompanied by a weight loss. A diagnosis of gastric intussusception was made by computed tomography. A Billroth II distal gastrectomy was then performed, and complete en bloc removal (R0 resection) was achieved. Pathology confirmed a gastric schwannoma through positive immunohistochemical staining for S-100 protein.
Core tip: Schwannomas are rarely observed in the gastrointestinal tract. We present a case report of a rare complication of gastric schwannoma causing gastroduodenal intussusception that was successfully managed by a Billroth II distal gastrectomy.
- Citation: Yang JH, Zhang M, Zhao ZH, Shu Y, Hong J, Cao YJ. Gastroduodenal intussusception due to gastric schwannoma treated by billroth II distal gastrectomy: One case report. World J Gastroenterol 2015; 21(7): 2225-2228
- URL: https://www.wjgnet.com/1007-9327/full/v21/i7/2225.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i7.2225
Schwannomas, also known as neurinomas, are tumors originating from any nerve that has a Schwann cell sheath[1]. Schwannomas are rarely observed in the gastrointestinal tract; when they do occur there, the most common site is the stomach. The most common symptoms of a gastric schwannoma are abdominal pain or dyspepsia, gastrointestinal bleeding, and an abdominal mass[2]. Imaging modalities, such as computed tomography (CT), magnetic resonance imaging (MRI), esophagogastroduodenoscopy (EGD), and endoscopic ultrasound (EUS), might offer useful preliminary diagnostic information. Pre-operative investigation is not pathognomonic; therefore, many schwannomas are diagnosed as gastrointestinal stromal tumors (GISTs). The diagnosis of a schwannoma is based on immunohistochemical positivity for S-100 protein, a calcium-binding protein found within cell lines of neural crest origin[3]. Gastric schwannomas are almost uniformly benign, and surgery is regarded as the curative treatment of choice.
We present a case report of a gastric schwannoma causing gastroduodenal intussusception that was treated by Billroth II distal gastrectomy, which resulted in complete en bloc removal (R0 resection).
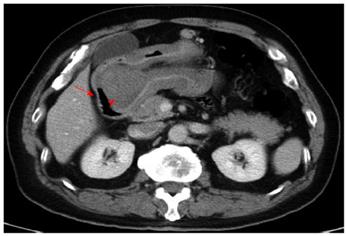
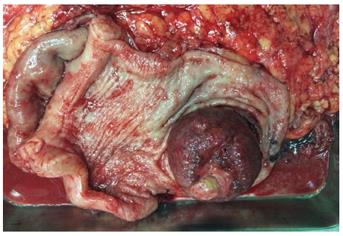
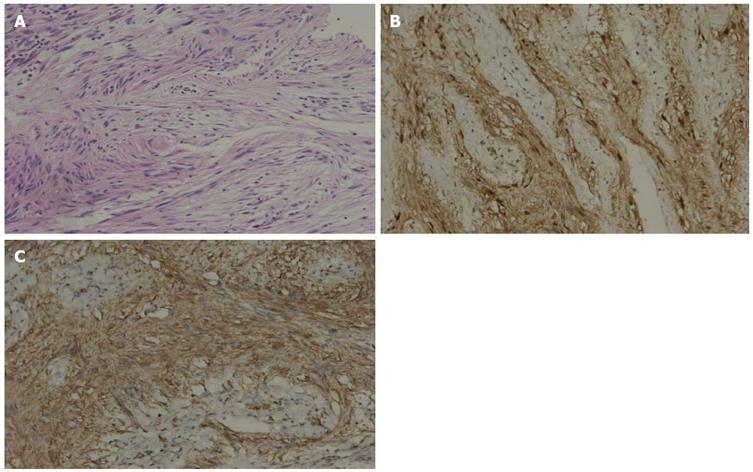
A 69-year-old man was admitted due to intermittent, colicky abdominal pain, nausea, and vomiting for over 4 wk, accompanied by a weight loss (5 kg in 4 wk). A clinical examination revealed succession splash. CT showed that a pedunculated soft tissue tumor mass at the gastric antrum, including the stomach wall and its outer mesentery, had telescoped into the duodenum through the gastric pylorus (Figure 1). We diagnosed that the gastric intussusception was likely induced by an antrum gastrointestinal stromal tumor. A conventional laparotomy was then performed, which showed an indentation of the inferior aspect of the gastric antrum with no evidence of metastasis, as seen below (Figures 2 and 3). A Billroth II distal gastrectomy was then performed, and complete en bloc removal (R0 resection) was achieved. Pathological analysis of the gastric mass confirmed a gastric schwannoma through positive immunohistochemical staining for S-100 protein and vimentin, whereas CD117, CD34, β-catenin, smooth muscle actin, synaptophysin, chromogranin and desmin were negative (Figure 4). The patient had an uneventful recovery and was discharged on his tenth day of hospitalization.
Gastroduodenal intussusception occurs in only 10% of adult intussusceptions[4]. Various gastric lesions, including adenocarcinoma, adenoma, GIST[5] and, as in our case, gastric schwannoma, can lead to intussusception. No previous case report has described gastroduodenal intussusception caused by gastric schwannoma, as was illustrated in our case.
A very rare complication of gastric schwannoma is gastroduodenal intussusception caused by the propulsion and prolapse of the tumor through the pylorus and into the duodenum[6]. The rarity of this condition is explained by the fact that the gastric cardia, the pylorus, and the duodenum are much more fixed than the rest of the alimentary tract. The intussusception presents as a partial or complete gastric outlet obstruction, resulting in severe, intractable pain, nausea, vomiting, and even shock[7]. The preoperative diagnosis of gastroduodenal intussusception is not difficult; however, imaging modalities, such as CT, MRI, EGD and EUS, only offer preliminary diagnostic etiologic information[8]. Schwannomas are easily misdiagnosed, frequently as GISTs, and their true nature is revealed only through accurate histological and immunohistochemical analysis. The diagnosis of schwannoma is based on immunohistochemical positivity for S-100 protein, a family of calcium-binding proteins found within cell lines of neural crest origin[9]. Digestive tract schwannomas never express CD117, CD34, c-kit, or DOG-1, in contrast to GISTs[10]. Our case was misdiagnosed as a GIST until these histological and immunohistochemical findings were revealed.
The definitive therapy for gastric schwannoma is surgical resection. Operations should follow the same principles as those for GISTs[11]. All tumors should be completely resected en bloc with the surrounding normal tissue, including the adjacent involved structures. Local extirpation, wedge resection, and partial, subtotal, or even total gastrectomy are all acceptable procedures[12]. Resection can be achieved via a laparoscopic or open approach. In our case, a symptomatic schwannoma of the gastric antrum approximately 5 cm in diameter was treated by a Billroth II distal gastrectomy, and the diagnosis was established microscopically and immunohistochemically after surgery.
Gastroduodenal intussusception is an uncommon complication of gastric schwannoma that typically presents as a gastric outlet obstruction. We report a patient with a gastric schwannoma who presented with a gastroduodenal intussusception. Moreover, we highlight how the tumor may be misdiagnosed pre-operatively despite both endoscopic and radiological assessments. The diagnosis of schwannoma is based on immunohistochemical positivity for S-100 protein. Resection surgery should be considered curative because such tumors are benign.
A 69-year-old man was admitted due to intermittent, colicky abdominal pain, nausea, and vomiting for over 4 wk, accompanied by a weight loss.
We diagnosed a likely gastric intussusception induced by a gastric tumor.
Gastrointestinal stromal tumor, gastric cancer, and gastric adenoma.
Routine blood test, metabolic panel, and liver function test were within normal limits.
A computed tomography scan revealed a gastroduodenal intussusception secondary to a gastric tumor.
Immunohistochemical staining revealed S-100/vimentin positivity, whereas tests for CD117, CD34, β-catenin, smooth muscle actin, synaptophysin, chromogranin, and desmin were negative.
A Billroth II distal gastrectomy was performed, and complete en bloc removal (R0 resection) was achieved.
Schwannomas, also known as neurinomas, are tumors originating from any nerve that has a Schwann cell sheath.
This case report demonstrates that gastroduodenal intussusception is an uncommon complication of gastric schwannomas. Moreover, such tumors may be misdiagnosed pre-operatively despite both endoscopic and radiological assessments. The diagnosis of schwannoma is based on immunohistochemical positivity for S-100 protein.
The case report entitled ”gastroduodenal intussusception due to gastric schwannoma treated by Billroth II distal gastrectomy” is interesting and well written.
P- Reviewer: Fiori E, Luo JC S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Liu XM
| 1. | Lin CS, Hsu HS, Tsai CH, Li WY, Huang MH. Gastric schwannoma. J Chin Med Assoc. 2004;67:583-586. [PubMed] [Cited in This Article: ] |
| 2. | Alvarez JF, Ben-David K. Gastric schwannoma: a rare find. J Gastrointest Surg. 2013;17:2179-2181. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Agaimy A, Märkl B, Kitz J, Wünsch PH, Arnholdt H, Füzesi L, Hartmann A, Chetty R. Peripheral nerve sheath tumors of the gastrointestinal tract: a multicenter study of 58 patients including NF1-associated gastric schwannoma and unusual morphologic variants. Virchows Arch. 2010;456:411-422. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Stubenbord WT, Thorbjarnarson B. Intussusception in adults. Ann Surg. 1970;172:306-310. [PubMed] [Cited in This Article: ] |
| 5. | Rittenhouse DW, Lim PW, Shirley LA, Chojnacki KA. Gastroduodenal intussusception of a gastrointestinal stromal tumor (GIST): case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 2013;23:e70-e73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Crowther KS, Wyld L, Yamani Q, Jacob G. Case report: gastroduodenal intussusception of a gastrointestinal stromal tumour. Br J Radiol. 2002;75:987-989. [PubMed] [Cited in This Article: ] |
| 7. | Lin F, Setya V, Signor W. Gastroduodenal intussusception secondary to a gastric lipoma: a case report and review of the literature. Am Surg. 1992;58:772-774. [PubMed] [Cited in This Article: ] |
| 8. | Atmatzidis S, Chatzimavroudis G, Dragoumis D, Tsiaousis P, Patsas A, Atmatzidis K. Gastric schwannoma: a case report and literature review. Hippokratia. 2012;16:280-282. [PubMed] [Cited in This Article: ] |
| 9. | Daimaru Y, Kido H, Hashimoto H, Enjoji M. Benign schwannoma of the gastrointestinal tract: a clinicopathologic and immunohistochemical study. Hum Pathol. 1988;19:257-264. [PubMed] [Cited in This Article: ] |
| 10. | Miettinen M, Lasota J. Gastrointestinal stromal tumors--definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch. 2001;438:1-12. [PubMed] [Cited in This Article: ] |
| 11. | Williamson JM, Wadley MS, Shepherd NA, Dwerryhouse S. Gastric schwannoma: a benign tumour often mistaken clinically, radiologically and histopathologically for a gastrointestinal stromal tumour--a case series. Ann R Coll Surg Engl. 2012;94:245-249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |